mental health awareness

Practical Training for
Carers
Facilitator Guide
Mental Health Awareness
Contents
Facilitator Guide
Workshop - 5 hours
B
EFORE YOU
B
EGIN
F
ACILITATOR
G
UIDE
SIGNS AND SYMPTONS OF COMMON MENTAL ILLNESS ................................................. 16
Please note:
This course is independently managed by Interwork Ltd and funded by a grant from the Australian
Government Department of Families, Housing, Community Services and Indigenous Affairs.
The opinions, comments and/or analysis expressed in this document are those of the author or authors and do not necessarily represent the views of the Minister for Disability Reform and cannot be taken in any way as expressions of government policy.
© Interskills
Version control is limited to the electronic document in Share point.
Once printed, this document ceases to be version controlled.
Version 1:04 Mental Health Awareness 2/38
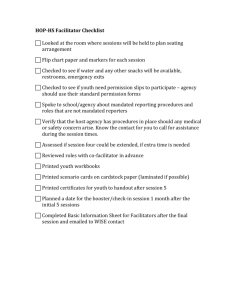
HOW TO USE THE FACILITATOR’S GUIDE
Here are some helpful hints to assist you in using this guide:
1.
Page Setup- Each page has two columns. The left column contains the current slide number and image plus the workbook page and symbol. The right column contains the segment title, description and activity instructions.
2.
Instructions- describe what you are doing and explaining. It also explains what the learner is doing.
Italicized text- This is scripted text of what the facilitator may say.
3.
Timing- The time estimates are printed for each segment. The time required varies with the group size and your experience. Times should be changed to suit learner and facilitator requirements. You can always ask the group when they would like to break.
© Interskills
Version control is limited to the electronic document in Share point.
Once printed, this document ceases to be version controlled.
Version 1:04 Mental Health Awareness 3/38
MATERIALS REQUIRED
Facilitator’s guide
Participant workbook (1 per person)
Computer, Power Point, Projector, cord/s and power board/s
USB with Power Point
Name tags (blank, 1 per participant)
Clock/timer
Coloured Markers
Pens (1 per participant)
Flipchart stand, paper and markers
Attendance sheet
Sticky notes with different mental illness written on back
Participant Evaluation
© Interskills
Version control is limited to the electronic document in Share point.
Once printed, this document ceases to be version controlled.
Version 1:04 Mental Health Awareness 4/38
SYMBOLS USED IN THE FACILITATOR’S GUIDE
#
Image here
SLIDE NUMBER AND IMAGE
Pge.
PARTICIPANT WORKBOOK
PARTNER ACTIVITY
GROUP ACTIVITY
© Interskills
Version control is limited to the electronic document in Share point.
Once printed, this document ceases to be version controlled.
Version 1:04 Mental Health Awareness
BREAK TIME
5/38
MENTAL HEALTH AWARENESS
Introduction TOTAL TIME: 40 Minutes
Ice Breaker: (10 minutes)
Facilitator to start with an Ice Breaker of their choice
Advise participants approximate break times and finish time for the day.
SLIDE 1
Introduction to module: (5 minutes)
Facilitator to give a brief description of the session, how this fits in to the Carer Training Program and using the
Workbook.
SLIDE 2
Group Rules: (5 minutes)
Discuss the rules/boundaries with the group
© Interskills
Version control is limited to the electronic document in Share point.
Once printed, this document ceases to be version controlled.
Version 1:04 Mental Health Awareness 6/38
SLIDE 3
Mental Health Awareness: (5 minutes)
1. Read through the slide
2. Advise the group of the following
“This training is a mental health awareness training only; you will not learn how to diagnose or apply therapeutic practices. You will however learn to recognise signs, reduce stigma and identify where to go for help.
Your workbook is designed to complement the training session. It should be reinforced that the workbook is a reference guide. Also I would be glad to answer questions after the training and we cannot help take down your details and pass you on to someone who can”.
SLIDE 4
Activity 1: (15 minutes)
1. GROUP ACTIVITY: Facilitator to introduce the activity .
Participants asked to choose from the list who in an ideal world they would like to be.
2. Ask individuals who they chose and why? Facilitator to share what mental illness the person had.
3. Explain to group “This introductory exercise is designed to reinforce the Mental Health Continuum – Anyone can get a mental illness!!!”
© Interskills
Version control is limited to the electronic document in Share point.
Once printed, this document ceases to be version controlled.
Version 1:04 Mental Health Awareness 7/38
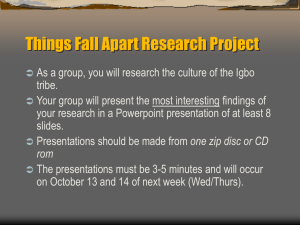
INTRODUCTION TO MENTAL HEALTH
TOTAL TIME: 1 hour 25 minutes
SLIDE 5
Overview of content: (2 minutes)
Introduce the topic- the topic will include information around what is mental health.
SLIDE 6
Activity 2: (15 minutes)
GROUP ACTIVITY: Facilitator to give participants 5 minutes to complete the myth or fact quiz
Advise group of answers and ask participants to record the number of correct responses they had in the relevant box.
Discuss responses.
© Interskills
Version control is limited to the electronic document in Share point.
Once printed, this document ceases to be version controlled.
Version 1:04 Mental Health Awareness 8/38
SLIDE 7
What is Mental Health: (15 minutes)
Ask the participants what kinds of things they do to remain mentally well.
PARTNER ACTIVITY: Break into pairs and come up with a definition of mental health and share with group.
Facilitator to describe “Good mental health - Good mental functioning, general mental wellbeing and not experiencing any problems in thinking, feeling and behaving. Has been described as ‘a state of complete physical, mental and social wellbeing and not merely the absence of disease or infirmity’ WHO 2003 and 2004. Positive Mental Health as opposed to the absence of mental health issues is described as the positively mentally healthy person experiencing these key elements. Recovery is a long and slow process and in many cases recovery focusses on positive mental health and management of symptoms rather than the illness simply going away. Empowerment, participation, community integration and building on existing strengths supports recovery and is a theme most trainers are familiar with. So put in extremely simple terms being mentally healthy is a combination of physical, emotional and social wellbeing.
It’s important to remember however that mental health may be seen on a continuum of good mental health to mental disorder and finally mental illness and most people will move up and down that continuum to a degree though not all will experience a mental disorder and less still a mental illness”.
SLIDE 8
Who is affected by mental health? (5 minutes)
Discuss the slide and pose the following statement to group “ there is a difference between mental health and mental illness”.
© Interskills
Version control is limited to the electronic document in Share point.
Once printed, this document ceases to be version controlled.
Version 1:04 Mental Health Awareness 9/38
SLIDE 9
Definition: (1 minutes)
Discuss “ Mental illness - Diagnosable illness that significantly interferes with cognitive, emotional and/or social abilities. There are specific symptoms associated with these illnesses that obviously inform diagnosis.
Significant changes in thinking, feelings and/or behaviours that are severe enough to that their day to day functioning is adversely affected which in turn causes them distress and can of course cause others distress.
BEST WAY TO DESCRIBE IT: You know it is an issue when it interferes with your day to day life…”
SLIDE 10
Activity 3: (15 minutes)
GROUP ACTIVITY: Ask the question and ask for people to guess the response.
© Interskills
Version control is limited to the electronic document in Share point.
Once printed, this document ceases to be version controlled.
Version 1:04 Mental Health Awareness 10/38
SLIDE 11
(5 minutes)
Read through and discuss slide
Facilitator to add
“This same report noted 7.3 million or
45% of Australians had experienced mental illness at some point in their lives.”
SLIDE 12
What causes mental illness? (10 minutes)
Read through and discuss slide
Facilitator to discuss “research confirms a combination of factors that influence a person’s mental health; a combination of genetics, brain chemistry and environment factors generally need to be present to induce a mental health disorder.
Combination of factors - Stressful live events can trigger a genetic predisposition of the development of a mental health illness in an otherwise mentally healthy person for example grief and loss, a traumatic accident or being the victim of a crime.
Due to the genetic link to most mental illnesses if a family member experiences mental health illness you are more likely to experience problems too.
Physical and mental health linked - There is a strong link between the quality of our physical and mental health.
Substance abuse - The use of illegal substances and alcohol have been proven to lead to mental health problems in many users. For example, there is a very strong link between psychosis and the use of marijuana and amphetamines“.
© Interskills
Version control is limited to the electronic document in Share point.
Once printed, this document ceases to be version controlled.
Version 1:04 Mental Health Awareness 11/38
SLIDE 13
Causes of Mental Illness: (10 minutes)
Discuss diagram with participants- go through each circle in diagram.
© Interskills
Version control is limited to the electronic document in Share point.
Once printed, this document ceases to be version controlled.
Version 1:04 Mental Health Awareness 12/38
ATTITUDES TOWARD MENTAL ILLNESS
TOTAL TIME: 55 minutes
SLIDE 14
Encourage client participation: (5 minutes)
Introduce the topic
SLIDE 15
Activity 4: (20 minutes)
GROUP ACTIVITY: Trainer to write a series of diagnosis
(that will be covered throughout the training session). They can stick the diagnosis on the back of the participant.
DIAGNOSIS should include- ANXIETY, DEPRESSION,
BIPOLAR DISORDER, and SCHIZOPHRENIA.
Participant asked to stand so group can see the diagnosis.
Each of the other participants is asked to say one word they associate with the diagnosis without using the word itself.
Participant to deduce their diagnosis.
SLIDE 16
Attitudes: (5 minutes)
Read slide and discuss
Facilitator to click on hyperlink http://www.youtube.com/watch?v=Dw_I-G1smoo stigma that goes along with the battle of dealing with mental illness
(1 min)
Pose question to group- I wonder how many of us would be honest to an employer and tell them they had a mental health issue?
© Interskills
Version control is limited to the electronic document in Share point.
Once printed, this document ceases to be version controlled.
Version 1:04 Mental Health Awareness 13/38
SLIDE 17
Attitudes continued…(5 minutes)
Read through slide
2. Discuss with group and say
“As we have discussed the stigma and stereotypes that surround mental health makes it increasingly difficult for people to get the right support and treatment. Stigma can be a destructive thing to live with and leads people who suffer from mental health problems to become excluded from normal society . It is now up to us to change our mind set and think about how we ourselves may stigmatise”.
SLIDE 18
(5 minutes)
Discuss “Media has played a significant role in creating stigma and incorrect stereotypes for example here are the kind of headlines you might have seen”.
Question to group: “Have they seen similar headlines and discuss.
SLIDE 19
Self and Perceived Stigma: (5 minutes)
Read through the slide
Discuss through examples “I am weak and not a man for having depression people will think less of me if I admit I need help” (work examples).
© Interskills
Version control is limited to the electronic document in Share point.
Once printed, this document ceases to be version controlled.
Version 1:04 Mental Health Awareness 14/38
SLIDE 20
(10 minutes)
Read through slide
GROUP ACTIVITY: Brainstorm ideas on changing stigma.
Suggestions might include: correcting people when they say wrong words/ tease etc.
© Interskills
Version control is limited to the electronic document in Share point.
Once printed, this document ceases to be version controlled.
Version 1:04 Mental Health Awareness 15/38
SIGNS AND SYMPTONS OF COMMON MENTAL ILLNESS
TOTAL TIME: 2 hours
SLIDE 21
Signs and Symptoms of Common Mental Illness: (2 minutes)
Introduce the topic- trainer to reiterate that we are not hear to diagnose people but to just discuss what medical experts tell us the sign and symptoms may be.
SLIDE 22
Mental Illnesses: (5 minutes)
Explain
“Mental illness covers a large area and could take up a huge part of the day. So we thought we would cover the four on the slide which I hope most of you will recognise as the illnesses that get the most press.”
SLIDE 23
Anxiety: (2 minutes)
Introduce the topic
Ask the group if they know what anxiety is? Discuss.
© Interskills
Version control is limited to the electronic document in Share point.
Once printed, this document ceases to be version controlled.
Version 1:04 Mental Health Awareness 16/38
SLIDE 24
Anxiety- Facts: (10 minutes)
Read read through slide
25% of the population experience anxiety disorders and will require treatment
These statistics are particular though I suspect they would be fairly consistent across all other developed countries.
25% more will experience less severe anxieties
These types of anxieties include fear of heights, snakes, spiders etc. Generally do not require treatment though for some people they do become so extreme and interfere with their daily lives to the extent that they do require treatment
2007 – Anxiety Disorders not common mental health issue for those aged between 16 to 85
14% of Australians suffered from Anxiety Disorders in the 12 months prior to the ABS survey reported in the 2009-10 Year
Book.
Women are 7% more likely to suffer Anxiety Disorders than men
Considered an Anxiety Disorder when significant interference in everyday life
Though many of us will experience symptoms of anxiety at times throughout our lives not all of us will develop and
Anxiety Disorder
When a persons symptoms begin to significantly interfere with their daily living their symptoms are considered to be those of an Anxiety Disorder
Considered an Anxiety Disorder when significant interference in everyday life
Typical Symptoms- Tension, Distress, Nervousness.
© Interskills
Version control is limited to the electronic document in Share point.
Once printed, this document ceases to be version controlled.
Version 1:04 Mental Health Awareness 17/38
SLIDE 25
Is stress the same as anxiety: (5 minutes)
Pose the question to the group
© Interskills
Version control is limited to the electronic document in Share point.
Once printed, this document ceases to be version controlled.
Version 1:04 Mental Health Awareness 18/38
SLIDE 26
Stress: (10 minutes)
Discuss with group
Stress is necessary part of life. May manifest in physical, mental and/or emotional responses
Stress is characterised by your body’s normal response to external and/or internal stimuli that upsets the normal balance of our lives and manifests in physical, mental, and/or emotional responses or adjustments
Perception is usually negative
Perception of stress is usually negative or bad however there is good or positive stress which is necessary for us to function
Automatic defensive physiological reaction
Enables response to threats – real and perceived
Stress is felt in and expressed through our bodies. This is nature’s way of enabling us to respond to perceived threats to our immediate safety or survival. It is often referred to as a flight or fight response. This fight or flight response is an inborn, automatic response triggered by the sympathetic nervous system which is part of the autonomic nervous system. This part of the nervous system controls many automatic functions such as those required by bodily organs than enable us to do such things as breathe and have a beating heart
Useful when needed otherwise maladaptive
If we need to react to a physical danger this stress response can be helpful however when we are stressed by an emotional experience the stress experience is negative as our bodies have received a boost of energy and strength but we have nothing to expend it on
As the body responds to a perceived threat everything around us seems to be magnified. We think, see, feel everything in our environment as a possible threat to our survival. Therefore we are constantly looking everywhere for possible danger. This explains why when stressed we tend to over react to things people say, do and behave around us. Our fears are increased and our thinking becomes distorted or simply not clear or accurate. We also tend to narrow our attention and focus to
© Interskills
Version control is limited to the electronic document in Share point.
Once printed, this document ceases to be version controlled.
Version 1:04 Mental Health Awareness 19/38
only things around us that we think can harm us which in turn makes us see everything through a filter or lens of fear when experiencing these physiological changes.
SLIDE 27
Stress and Anxiety Correlation: (5 minutes)
Read through slide
Inability to fight or flee from perceived danger
Our bodies are built to return to their previous not aroused state once the threat has been dealt with. However, in many cases today and specifically for us, when we are faced with medical conditions that require management, action, decision/s, we cannot fight or flee from our perceived danger.
Our body is prepared for physical action, fighting or fleeing/running from the danger but this physical response will not fix the problem
It seems our bodies can store stress hormones if we don’t do things to metabolise or breakdown these hormones effectively
Under great stress our ability to think is often compromised or negatively affected; we are not able to think as clearly or concentrate as well as when we are not feeling stress, anxiety, fear and pain. At these times it is also very difficult and sometimes impossible to perceive or learn new information.
This is because the additional stress we are suffering affects our short-term memory making it much more difficult for us to plan and make thoughtful and considered decisions; in this situation we are more likely to make ill-informed and hasty decisions that may not be best for us, our health and/or our family in the long-term
Excessive levels of stress are likely to lead to anxiety which is typically characterised by a feeling of overwhelming fear, worry and apprehension and often feelings of impending doom. This in turn often leads to increased stress and anxiety.
© Interskills
Version control is limited to the electronic document in Share point.
Once printed, this document ceases to be version controlled.
Version 1:04 Mental Health Awareness 20/38
SLIDE 28
Common Anxiety Disorders: (2 minutes)
Read through slide- discuss comparisons between male and female. Pose the question of why do you think female is higher? Suggested response may be because makes do not go to doctors and get a formal diagnosis.
SLIDE 29
Generalised Anxiety Disorder: (10 minutes)
Facilitator to discuss “Roughly 5% of the Australian population will suffer from GAD during their lifetime
People whose temperaments lend themselves being worriers seem to more susceptible to this disorder. Sufferers typically experience excessive and uncontrollable worry disproportionate to the activating event often expecting a disaster to occur i.e., they simply worry about things that may go wrong or that they may not cope. These events are often simple day-to-day concerns and their excessive worrying culminates in daily worry, fear and dread. This behaviour must have be recurrent on most days for at least 6 months for a diagnosis to be considered
QUOTE “I have been through some horrible things in life.
Some of them actually happened” This was someone's personal experience of anxiety and their view that they would worry over things that actually never happened
Discuss symptoms in workbook and tell participants that the workbook contains specific information about ANXIETY
DISORDERS -Panic Disorder, Agoraphobia, OCD, Social
Phobia and Post Traumatic Stress Disorder.
© Interskills
Version control is limited to the electronic document in Share point.
Once printed, this document ceases to be version controlled.
Version 1:04 Mental Health Awareness 21/38
SLIDE 30
Depression: (2 minutes)
Introduce the topic- Ask the group if they know a little about depression and asked them to share.
SLIDE 31
Depressed Mood or Depression: (5 minutes)
Read through slide.
4.1% of Australians will suffer from a major depressive disorder in any given year and the average age of onset is 25 years (8). Around 160,000 Australian youth live with depression and this is the most common mental health problem for young people. Approximately 1 in 5 people will experience depression by the time they reach adulthood
Those who experience depression and remain untreated are at higher risk of death by suicide
Unlike the low or sad moods most of us experience at times in our lives and sometimes incorrectly label as depression, depression is an illness that is much more severe, it lasts longer than two weeks and interferes with other areas of life for example, work, study, relationships (10). Depression is often comorbid with anxiety and/or substance abuse disorders
Depression is actually descriptive of emotions being depressed, lowered and/or or kept down. Depressed people often stop enjoying life and lose interest in things they used to like doing, People with depression often find it hard to cope from day to day
Refer group to workbook and discuss the symptoms.
© Interskills
Version control is limited to the electronic document in Share point.
Once printed, this document ceases to be version controlled.
Version 1:04 Mental Health Awareness 22/38
SLIDE 32
Causes: (5 minutes)
Read through slide
Discuss “ A combination of causes is again thought to lead to depression and they are different for everyone. Genetics mean there is a hereditary predisposition for some to developing depression while environmentally depression may sometimes occur as a response to something while for other people depression develops for no apparent reason”.
SLIDE 33
Words to Avoid: (5 minutes)
Prior to showing this slide, pose the following question to group “what kinds of things should not be said to someone who is clinically depressed”. Discuss
Show slide to group.
SLIDE 34
Bipolar Disorder: (2 minutes)
Introduce the topic- discuss that Bipolar was referred to as
Manic Depression. The name change became official in 1980, with the publication of the third edition of the Diagnostic and
Statistical Manual of Mental Disorders (DSM), the term manic depression was officially changed in the classification system to bipolar disorder.
In the last few decades the medical profession (psychiatry specifically) has made a concerted effort to shift the vernacular to the official DSM diagnostic term of bipolar disorder. There are a number of reasons cited for this shift.
"Manic depression" has generally been used to denote a wide array of mental illnesses, and as classification systems have become more sophisticated, the new term of bipolar disorder allows for more clarity in a diagnosis.
The term "manic depression" has been greatly stigmatized.
© Interskills
Version control is limited to the electronic document in Share point.
Once printed, this document ceases to be version controlled.
Version 1:04 Mental Health Awareness 23/38
Consider popular phrases such "manic Monday," Animanics, homicidal maniac, etc. And "depression" is commonly used for periods of sadness that don't really qualify as clinical depression.
SLIDE 35
Bipolar Disorder: (5 minutes)
Read and discuss slide
SLIDE 36
Mania: (5 minutes)
Read through slide
Facilitator to explain “
Manic symptoms are typified by an elevated mood which is exhibited by the person having plenty of energy, racing thoughts, full of ideas, little need for sleep, rapid speech, trouble focusing on tasks, frustration and irritability and lack of inhibitions which may result in risks being taken that wouldn’t normally.
During the manic phase the person tends to be optimistic, excessively happy and experience exaggerated feelings of wellbeing. Their mind is overactive and their need for sleep is significantly reduced. Although they have abundant energy they lack concentration which may result in their work and/or study suffering. It is not uncommon for them to lose touch with reality and experience episodes of psychosis”.
SLIDE 37
Bipolar 1 & 11: (5 minutes)
Read through slide
Facilitator to explain “
Bipolar I people experience one or more manic episodes and often one or more major depressive episodes. The depressive episodes can last for several weeks
© Interskills
Version control is limited to the electronic document in Share point.
Once printed, this document ceases to be version controlled.
Version 1:04 Mental Health Awareness 24/38
to several months whilst alternating with intense symptoms of mania that can last just as long. Periods of ‘normal’ mental health may occur during these extremes. Seasonal changes may affect symptoms as could stress life situations
Bipolar II symptomology is the same as Bipolar I except the manic episodes tend not to be as extreme. These less extreme manic episodes were once referred to as hypomanic episodes.”
SLIDE 38
Causes: (5 minutes)
Read through slide
Explain “ There are a number of factors which may influence the development of Bipolar Disorder. Hereditary factors are likely to play a large role; of the 2% of people who experience
Bipolar Disorder, 10% of those will have at least one parent with Bipolar Disorder
A number of environment factors may also trigger symptoms such as changes in jobs, living arrangements, family and relationship problems, having suffered from physical and/or emotional abuse or trauma including verbal and sexual abuse, grief due to the death or loss or someone and/or other major life transitions such as having a baby
Physical health matters may also trigger symptoms eg pregnancy/childbirth, hormone problems eg hyper/hypothyroidism, brain conditions eg Huntington’s
Disease, Autoimmune problems eg HIV and cancer.”
SLIDE 39
Schizophrenia: (2 minutes)
Introduce the topic- Schizophrenia is often misinterpreted as having multiple personality.
© Interskills
Version control is limited to the electronic document in Share point.
Once printed, this document ceases to be version controlled.
Version 1:04 Mental Health Awareness 25/38
SLIDE 40
Activity 5: (10 minutes)
PARTNER ACTIVITY: Break the group into pairs. In pairs discuss what schizophrenia means to you? Discuss with group.
SLIDE 41
Schizophrenia: (10 minutes)
Read through slide
© Interskills
Version control is limited to the electronic document in Share point.
Once printed, this document ceases to be version controlled.
Version 1:04 Mental Health Awareness 26/38
SLIDE 42
Schizophrenia: (5 minutes)
Read through slide
Explain:
“What are the symptoms?
If not receiving treatment, people with schizophrenia experience persistent symptoms of what is called psychosis.
These include:
Confused thinking
When acutely ill, people with psychotic symptoms experience disordered thinking. The everyday thoughts that let us live our daily lives become confused and don’t join up properly
Delusions
A delusion is a false belief held by a person which is not held by others of the same cultural background
Hallucinations
The person sees, hears, feels, smells or tastes something that is not actually there. The hallucination is often of disembodied voices which no one else can hear
Other associated symptoms are low motivation and changed feelings”.
© Interskills
Version control is limited to the electronic document in Share point.
Once printed, this document ceases to be version controlled.
Version 1:04 Mental Health Awareness 27/38
SLIDE 43
Schizophrenia Common Questions: (10 minutes)
Read through slide
One in a 100 people develops schizophrenia at some time in their life. However with support and treatment many people recover and lead normal everyday lives
It usually begins during adolescence or early adulthood, generally a little later in women than men. It may occur in people from all classes, cultures and walks of life. About half of those admitted to hospital for mental health reasons have schizophrenia.
The causes of schizophrenia are not fully understood. They are likely to be a combination of hereditary and other factors. It is probable that some people are born with a predisposition to develop this kind of illness, and that certain things — for example, stress or use of drugs such as marijuana, LSD or speed — can trigger their first episode
Treatment can do much to reduce and even eliminate the symptoms. Treatment should generally include a combination of medication and community support. Both are usually essential for the best outcome. Medication- Certain medications assist the brain to restore its usual chemical balance. This then helps reduce or get rid of some of the symptoms. Community support programs- This support should include information; accommodation; help with finding suitable work; training and education; psychosocial rehabilitation and mutual support groups. Understanding and acceptance by the community is also very important”.
© Interskills
Version control is limited to the electronic document in Share point.
Once printed, this document ceases to be version controlled.
Version 1:04 Mental Health Awareness 28/38
POSITIVE MENTAL HEALTH AND SUPPORT
TOTAL TIME: 60 minutes
SLIDE 44
Positive mental health and support: (2 minutes)
Introduce the topic
© Interskills
Version control is limited to the electronic document in Share point.
Once printed, this document ceases to be version controlled.
Version 1:04 Mental Health Awareness 29/38
SLIDE 45
10 tips to positive mental health: (10 minutes)
Explain
1. Develop and maintain strong relationships with people around you who will support and enrich your life. The quality of our personal relationships has a great effect on our wellbeing. Putting time and effort into building strong relationships can bring great rewards
2. Set aside time for activities, hobbies and projects you enjoy. Let yourself be spontaneous and creative when the urge takes you. Do a crossword; take a walk in your local park; read a book; sew a quilt; draw pictures with your kids; play with your pets – whatever takes your fancy
3. Join a club or group of people who share your interests. Being part of a group of people with a common interest provides a sense of belonging and is good for your mental health. Join a sports club; a band; an evening walking group; a dance class; a theatre or choir group; a book or car club
4. Volunteer your time for a cause or issue that you care about.
Help out a neighbour, work in a community garden or do something nice for a friend. There are many great ways to contribute that can help you feel good about yourself and your place in the world. An effort to improve the lives of others is sure to improve your life too
5. Be active and eat well – these help maintain a healthy body.
Physical and mental health are closely linked; it’s easier to feel good about life if your body feels good. You don’t have to go to the gym to exercise – gardening, vacuuming, dancing and bushwalking all count. Combine physical activity with a balanced diet to nourish your body and mind and keep you feeling good, inside and out”.
© Interskills
Version control is limited to the electronic document in Share point.
Once printed, this document ceases to be version controlled.
Version 1:04 Mental Health Awareness 30/38
SLIDE 46
10 tips to positive mental health: (10 minutes)
6. Learn a new skill or take on a challenge to meet a goal. You could take on something different at work; commit to a fitness goal or learn to cook a new recipe. Learning improves your mental fitness, while striving to meet your own goals builds skills and confidence and gives you a sense of progress and achievement
7. Be aware of what triggers your stress and how you react. You may be able to avoid some of the triggers and learn to prepare for or manage others. Stress is a part of life and affects people in different ways. It only becomes a problem when it makes you feel uncomfortable or distressed. A balanced lifestyle can help you manage stress better. If you have trouble winding down, you may find that relaxation breathing, yoga or meditation can help
8. Get plenty of sleep. Go to bed at a regular time each day and practice good habits to get better sleep. Sleep restores both your mind and body. However, feelings of fatigue can still set in if you feel constantly rushed and overwhelmed when you are awake.
Allow yourself some unfocussed time each day to refresh; for example, let your mind wander, daydream or simply watch the clouds go by for a while. It’s OK to add ‘do nothing’ to your to-do list
9. Take a moment to notice each of your senses each day. Simply
‘be’ in the moment – feel the sun and wind on your face and notice the air you are breathing. It’s easy to be caught up thinking about the past or planning for the future instead of experiencing the present. Practising mindfulness, by focusing your attention on being in the moment, is a good way to do this. Making a conscious effort to be aware of your inner and outer world is important for your mental health
10. This can be as simple as asking a friend to babysit while you have some time out or speaking to your doctor (GP) about where to find a counsellor or community mental health service. The perfect, worry-free life does not exist. Everyone’s life journey has bumpy bits and the people around you can help. If you don’t get the help you need first off, keep asking until you do.
© Interskills
Version control is limited to the electronic document in Share point.
Once printed, this document ceases to be version controlled.
Version 1:04 Mental Health Awareness 31/38
\
SLIDE 47
Where to get help: (5 minutes)
Refer to workbook page 34 and discuss
SLIDE 48
Activity 6: (20 minute
GROUP ACTIVITY:
Break group into smaller groups (2-3 people).
From the
Workbook choose one case study per group. Ask the participants to read through their case study and prepare their responses on butcher’s paper and then share with group
SLIDE 49
Activity 7: (5 minutes)
Ask participants to turn to the person next to them and tell them what they are now going to do to improve their mental health. Share with group.
SLIDE 50
Final Thought! (2 minutes)
Read through slide- How can we break down the stigma?
Suggested ideas- inclusive practices, acceptance
© Interskills
Version control is limited to the electronic document in Share point.
Once printed, this document ceases to be version controlled.
Version 1:04 Mental Health Awareness 32/38
RECAP
SLIDE 51
Summarise and overview of session (10 minutes)
Discuss the session and ask for feedback/evaluation
Ask each participant in the group to share something that they have learnt from the session with the rest of the group.
© Interskills
Version control is limited to the electronic document in Share point.
Once printed, this document ceases to be version controlled.
Version 1:04 Mental Health Awareness 33/38
REFERENCES
1. International society for the psychological treatments of the schizophrenias and other psychoses. International society for the psychological treatments of the schizophrenias and other
psychoses. [Online] [Cited: 1 February 2012.] http://ispsuk.org/?p=312.
2. ABS. National Survey of Mental Health and Wellbeing: Summary of Results, 2007. Australian
Bureau of Statistics. [Online] 2008. [Cited: 1 February 2012.] http://www.abs.gov.au/AUSSTATS/abs@.nsf/Lookup/4326.0Explanatory%20Notes12007?OpenDo
cument.
3. Beyond Blue. [Online] [Cited: 1 February 2012.] http://www.beyondblue.org.au.
4. WHO. Promoting mental health - summary report. France : World Health Organisation, 2004.
5. Investing in Mental Health pdf. World Health Organisation. [Online] 2003. [Cited: 5 February
2012.] www.who.int/mental_health.
6. Lynne Friedli, Michale Parsonage. Pdf. Community Health Exchange. [Online] [Cited: 6 February
2012.] http://www.chex.org.uk/media/resources/mental_health/Mental%20Health%20Promotion%20-
%20Building%20an%20Economic%20Case.pdf.
7. Pathways, rehabilitation and support services ltd. [Online] [Cited: 1 February 2012.] http://www.pathways.org.au/index.php?option=com_content&view=article&id=36:mental%20hea lth&catid=7&Itemid=25.
8. Kitchener BA, Jorm AF, Kelly CM. Mental health first aid manual 2edn. Melbourne : Orygen
Youth Health Research Centre, 2010.
9. ABS Australian Social Trends 4102.0 2009 - Mental Health pdf. Australian Bureau of Statistics .
[Online] 2009. [Cited: 7 February 2012.] http://www.ausstats.abs.gov.au/ausstats/subscriber.nsf/LookupAttach/4102.0Publication25.03.09
4/$File/41020_Mentalhealth.pdf.
10. Reachout Australia. [Online] [Cited: 6 February 2012.] http://au.reachout.com/.
11. 7. [Online] http://www.nald.ca/library/research/famlithea/cover.htm.
12. ABS. 2009-10 Year Book Australia. Canberra : Australian Bureau of Statistics, 2010. Vol. Number
91, ABS Catalogue No. 1301.0.
© Interskills
Version control is limited to the electronic document in Share point.
Once printed, this document ceases to be version controlled.
Version 1:04 Mental Health Awareness 34/38
13. Better Health Chanel. Better Health, Victorian Government. [Online] [Cited: 5 February 2012.] http://www.betterhealth.vic.gov.au/bhcv2/bhcarticles.nsf/pages/Anxiety_disorders_overview?op
en.
14. Neimark, MD. The Fight or Flight Response. Mind/Body Education Center. [Online] [Cited: 5 July
2011.] http://www.thebodysoulconnection.com/EducationCenter/fight.html.
15. What is Stress. Understanding and Dealing with Stress. [Online] [Cited: 7 February 2012.] http://www.mtstcil.org/skills-definition-1.html.
16. Stress. Oracle Think Quest. [Online] [Cited: 6 July 2011.] http://library.thinkquest.org/C0123421/index.htm.
17. WebMD Medical Reference. Medicine Net.com. [Online] February 2009. [Cited: 3 February
2012.] http://222.medicinenet.com/anxiety/page3.htm.
18. The Medical Journal of Australia. [Online] 1998. [Cited: 5 February 2012.] http://www.mja.com.au.
19. Fact File: Anxiety Disorders. ABC Health and Wellbeing. [Online] 7 June 2005. [Cited: 3 February
2012.] http://www.abc.net.au/health/library/stories/2005/06/07/1828950.htm.
20. End anxiety for ever. [Online] [Cited: 6 February 2012.] http://www.endanxietyforever.com/index.html.
21. Youth Beyond Blue. [Online] [Cited: 2 February 2012.]
22. Australian Government: Job Access/Disability. [Online] [Cited: 4 February 2012.] http://jobaccess.gov.au/Advice/Disability/Pages/Dysthymic_Depression.aspx.
23. Medline Plus. National Institute of Health. [Online] 2010. [Cited: 8 February 2012.] http://www.nlm.nih.gov/medlineplus/ency/article/000918.htm.
24. PubMed Health. US National Library of Medicine. [Online] 2012. [Cited: 8 February 2012.] http://www.ncbi.nlm.nih.gov/pubmedhealth.
25. Mental illness: myth versus fact. Mental Health Foundaton of Australia (Victoria). [Online]
[Cited: 7 February 2012.] http://www.mentalhealthvic.org.au/index.php?id=112.
26. Mental Health and Wellbeing: Profile of Adults, Australia, 1997. Australian Bureau of Statistics.
[Online] [Cited: 5 February 2012.] http://www.abs.gov.au/AUSSTATS/abs@.nsf/Lookup/4326.0Main+Features11997.
27. [Online] http://www.health.gov/communication/literacy/quickguide/factsbasic.htm.
28. Zarcadoolas, Pleasant, & Greer. [Online] http://www.en.wikipedia.org/wiki/health_literacy.
© Interskills
Version control is limited to the electronic document in Share point.
Once printed, this document ceases to be version controlled.
Version 1:04 Mental Health Awareness 35/38
29. [Online] http://en.wikipedia.org/wiki/health_literacy.
30. [Online] http://www.abs.gov.au/AUSSTATS/abs@.nsf/Latestproducts/4233.0Main%20Features22006?open
document&tabname=Summary&prodno=4233.0&issue=2006&num=&view=)..
31. [Online] http://www.health.gov/communication/literacy/quickguide/factsbasic.htm.
32. Quickgude. [Online] http://www.health.gov/communication/literacy/quickguide/factsbasic.htm.
33. 1. [Online] http://www.health.gov/communication/literacy/quickguide/factsbasic.htm.
34. 2. [Online] Zarcadoolas, Pleasant, & Greer, 2006 at http://en.wikipedia.org/wiki/health_literacy).
35. 3. [Online] http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1831571/; USA Department of health and Human Services, 2000.
36. 4. [Online] http://www.abs.gov.au/AUSSTATS/abs@.nsf/Latestproducts/4233.0Main%20Features22006?open
document&tabname=Summary&prodno=4233.0&issue=2006&num=&view=.
37. 5. [Online] http://heapro.oxfordjournals.org/content/24/3/285.full.
38. 5. [Online] http://en.wikipedia.org/wiki/health_literacy.
39. 6. [Online] World health Organization, 1998.
40. 7. [Online] http://www.healthliteracy.com/article.asp?PageID=3791.
41. 8. [Online] http://www.patientsorganizations.org/healthliteracy .
42. 9. [Online] http://www.ahrq.gov/qual/literacy/.
43. 9. [Online] http://definitionofwellness.com/dictionary/health-literacy.html.
44. Weiss, BD (MD). 13. Health literacy and patitent safety: help patients understand, 2nd edn. s.l. :
American Medical Association Foundation and American Medical Association, 2007.
45. The Body Soul Connection. [Online] [Cited: 10 July 2011.] http://www.thebodysoulconnection.com/EducationCenter/fight/html.
46. Dionne-Coster, S Sauve, L Shively, J. Family Literacy and Health. Canada : Centre for Family
Literacy, 2007.
© Interskills
Version control is limited to the electronic document in Share point.
Once printed, this document ceases to be version controlled.
Version 1:04 Mental Health Awareness 36/38
47. Library think quest. [Online] [Cited: 6 July 2011.] http://library.thinkquest.org/CO123421/index.htm.
48. Druss, B (MD, MPH) Reisinger Walker (MAT, MPH) E. Mental Diosrders and medical comorbidity. Robert Wood Johnson Foundation. [Online] February 2011. [Cited: 7 February 2012.] http://www.rwjf.org/files/research/021011.policysynthesis.mentalhealth.report.pdf.
49. ABS. Mental Health and Wellbeing: Profile of Adults, Australia - 1997. Canberra : Australian
Bureau of Statistics, 1998. Vol. ABS Catalogue No. 4326.0, ISBN 0 642 25726 4.
50. Statistics, Australia Bureau of. 2009-10 Year Book Australia. Canberra : Australian Bureau of
© Interskills
Version control is limited to the electronic document in Share point.
Once printed, this document ceases to be version controlled.
Version 1:04 Mental Health Awareness 37/38