Thorax VIVA`s - WordPress.com
advertisement
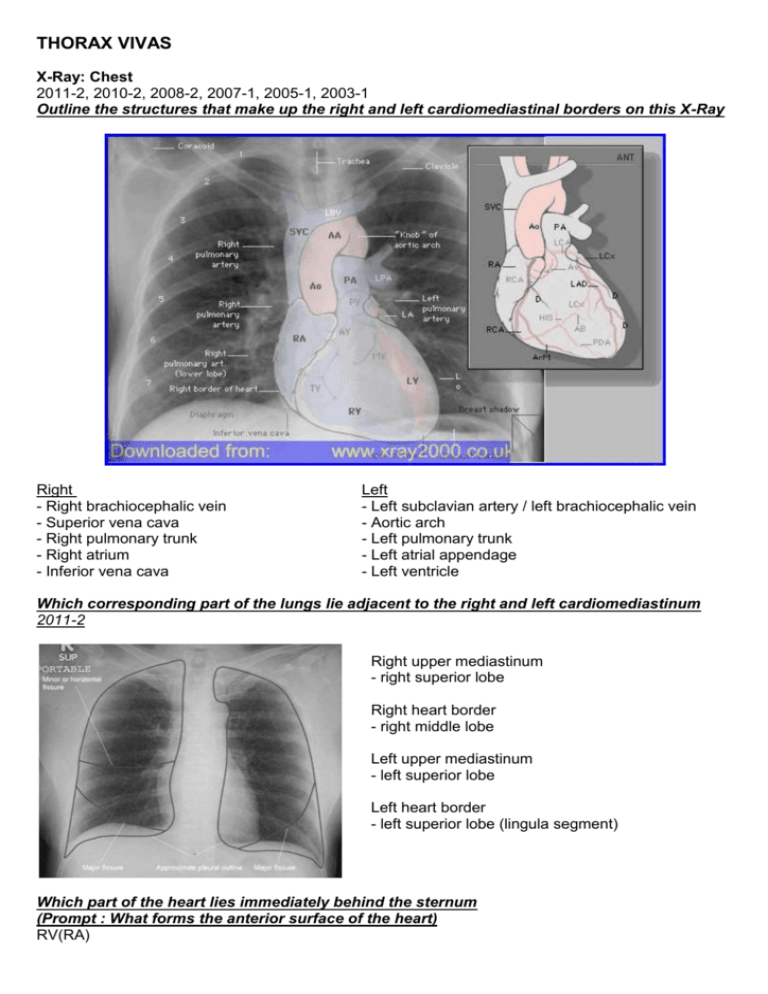
THORAX VIVAS X-Ray: Chest 2011-2, 2010-2, 2008-2, 2007-1, 2005-1, 2003-1 Outline the structures that make up the right and left cardiomediastinal borders on this X-Ray Right - Right brachiocephalic vein - Superior vena cava - Right pulmonary trunk - Right atrium - Inferior vena cava Left - Left subclavian artery / left brachiocephalic vein - Aortic arch - Left pulmonary trunk - Left atrial appendage - Left ventricle Which corresponding part of the lungs lie adjacent to the right and left cardiomediastinum 2011-2 Right upper mediastinum - right superior lobe Right heart border - right middle lobe Left upper mediastinum - left superior lobe Left heart border - left superior lobe (lingula segment) Which part of the heart lies immediately behind the sternum (Prompt : What forms the anterior surface of the heart) RV(RA) In the supine position, which mediastinal structures are located at the same level as the sternal angle. (Prompt: What mediastinal structures would you see if you looked at a transverse slice though the chest at the level of T4-5?) 2010-2 Mediastinal structures at the transverse thoracic plane Carina (bifurcation), Division of pulmonary trunk, Reflection of the pericardium, SVC (enters R atrium), Hila of the lungs, Transverse fissure of R lung, Ascending aorta becomes arch, Arch becomes descending Aorta, Phrenic nerve, Vagus nerve, L recurrent laryngeal nerve origin Azygos vein, Thoracic duct (crosses from R to L), Pleura approaches the midline anteriorly, Oesophagus Please describe the surface anatomy of the heart. 2008-2 - Left 2nd costal cartilage - Right 3rd costal cartilage - Right 6th costal cartilage - 5th Inter-costal space in left midclavicular line about 9cm from the midline - Has about 1/3 to the right of the midsternal line and 2/3 to the left Point to diaphragms: Ask: what is this structure, and what are its attachments? 2008-2, 2007-1 Diaphragm is a musculotendinous partition separating the thoracic and abdominal cavities, and is the chief muscle of respiration (inspiration). It has a trifoliate aponeurotic central tendon attached to the IVC and pericardium but no boney attachments – it is completely surrounded by the muscular part that is divided into 3 parts based on peripheral attachments: Sternal part: 2 muscular slips to posterior aspect of the xiphisternum Costal part: Internal surfaces of 7th -12th (inferior 6) costal cartilages Lumbar part: Arises from medial and lateral arcuate ligaments, and the (L) and (R) crura centrally: 1. Medial arcuate is thickening of psoas fascia, from L1/L2 vertebrae to a ridge on transverse process of L1 2. Lateral arcuate ligament starts from L1 transverse process and goes to 12th rib lat to quadratus lumborum (covering this muscle) 3. Crura: (R) is fixed to upper 3-4 lumbar vertebrae and discs between, (L) is attached to upper 2-3, (R) crus fibres slope up to (L) and surrounds the oesophagus (as the hiatus) 4. Median arcuate ligament is fibers from medial edge of each crus that unite with each other in front of aorta at T12, and with the crura form the aortic hiatus What are the openings in the diaphragm 2007-1 Opening Location Aortic T12 in midline Oesophageal Caval Other smaller Transmits Aorta, thoracic duct, azygos vein T10 2.5cm to (L) Surrounded by sling from (R) crus T8 just to (R) Oesophagus, vagal trunks (ant and post), (L) gastric vessels, lymphatics IVC (attached – aids return), (R) phrenic nerve Splanchnic nerves, sympathetic trunk, subcostal nerve and vessels, (L) phrenic, neurovascular bundles of 7-11 intercostal spaces, superior epigastric vessels What is the nerve supply of the diaphragm? 2008-2 Phrenic nerves (C3-5): Entire motor supply via (L) and (R) to corresponding side of the diaphragm from the inferior surface. Sensory innervation also mostly from the phrenic, but the periphery (costal portion) also from the lower 6-7 intercostal and the subcostal nerves. How does contraction of the diaphragm result in ventilation of the lungs? 2008-2 - With inspiration contraction causes descent of the central part (periphery is attached) - The domes flatten - Results in decrease in intrathoracic (and pleural) pressure -> lungs inflate - Diaphragmatic contractions responsible for 75% of inspiratory respiratory muscle action - Much of expiration is passive recoil, so the diaphragm is considered the chief muscle of respiration - Note paradoxical movement seen with paralysis (i.e. phrenic nerve injury) – the affected dome will rise with inspiration - Also there is a slight rise in intra-abdominal pressure, and opening of the IVC (via is attachment at the caval opening) – this mechanism aids central venous return Mnemonic: AOC = 12,10,8 2008-1 Describe the intercostal muscles Muscle Levator costarum External intercostal Internal intercostal Innermost intercostal Subcostal Transversus thoracis - - - Sup. Attach Transverse processes of T7-11 Inferior Attach Subjacent ribs between tubercle and angle Innervation Posterior primary rami of C8-T11 nerves Main Action Elevate ribs Elevate ribs during forced inspiration Inferior border of ribs Internal surface of lower ribs near their angles Posterior surface of lower sternum Superior border of ribs below Superior borders of 2nd or 3rd ribs below Internal surface of costal cartilages 2-6 Interosseous part: depresses ribs During active (forced) respiration Interchondral part: elevates ribs Probably act in same manner as internal Intercostal nerve intercostal muscles Weakly depress ribs (Proprioception?) External intercostal: from tubercles of ribs posteriorly to costochondral junction (thence external intercostal membrane) run infero-anteriorly and are most active during inspiration (to increase tonus of intercostal space) and during forced inspiration Internal intercostal: deep to and at right angles to externals from sternum to angle of ribs posteriorly (continued posteriorly as internal intercostal membrane) run infero-posteriorly and are most active during expiration (to increase tonus of intercostal space). Interosseous portions act during forced expiration whilst interchondral portion act during active inspiration Innermost intercostals: essentially the deeper parts of the internals separated from them by the intercostal nerves and vessels. Occur laterally Subcostals: run in the same direction as the internals, but cross 2 or 3 spaces, lower spaces Transverse thoracic: run from sternum and xiphisternum transversely to lower ribs Levator costarum: from transverse processes to ribs Describe the pattern of distribution of neurovascular structures in the thoracic wall - Enter the most medial part of posterior intercostal space - Intercostal (and collateral) nerve from anterior rami of T1-11, T12 is subcostal nerve - Run between parietal pleura and internal intercostal membrane in the middle of the space - Near the angle of ribs pass between internal and innermost intercostal muscles - Located in costal grooves on inferior border of the ribs with nerve inferior to artery inferior to vein - Collateral branches arise here and run along superior border of rib, nerve superior to artery to vein - Vessels also have anterior supply and drainage (internal thoracic artery) Describe the arterial supply of the intercostal spaces - Posterior intercostal arteries: Branches of the supreme/superior intercostal artery from the costocervical trunk of the subclavian -> 1 & 2, and of the thoracic aorta -> others - Anterior intercostal arteries: Branches of the internal thoracic -> spaces 1 to 6, musculophrenic artery -> spaces 7 to 9) - The internal thoracic artery arises from the subclavian, passes inferiorly lateral to the sternum, between costal cartilages and transverse thoracic muscle, divides at 6 th ICS into musculophrenic (lateral) and superior epigastric arteries 2006-1 What are the surface landmarks for the insertion of anterior and lateral intercostal tubes Anterior: 2nd intercostal space in the mid clavicular line Lateral: 4th or 5th intercostal space just anterior to the mid axillary line What are the layers traversed when inserting through the lateral chest wall? 2006-1, 2007-1 1. Skin & subcutaneous tissue 2. Layers of muscle (3 layers), external, internal and innermost intercostals 3. Parietal Pleura Where do the intercostal vessels run? - Under the rib above - Between the middle and innermost intercostal muscles - There is also collateral vessels at the lower section of the intercostal space 2004-2 Identify the major parts of this bone (Rib & Thoracic Vertebrae) What are the contents of the intercostal space - Three layers of muscle, external, internal and innermost - Between middle & inner under rib above lies: - Vein - Artery - Nerve 2010-1, 2007-1, 2005-2 Bone: First Rib What bone is this? First Rib Appropriate side What are the bony landmarks? - Head (with single facet for T1) - Neck - Tubercle for transverse process of T1 - Superior surface, lateral to medial Groove for subclavian artery Scalene tubercle and ridge Groove for subclavian vein - Costal groove What muscles attach to this bone? - Anterior scalene (tubercle) - Middle scalene (medial to groove for artery) - Intercostals - Serratus anterior - Subclavius (at costochondral junction) - Longissimus portion of erector spinae attaches between tubercle and angle 2007-1, 2005-2 What are the neurovascular relations of this bone? Nerves - C8-T1 above and below neck - Sympathetic trunk in contact with neck next to head - Underneath the first intercostal neurovascular bundle - In groove for subclavian artery is lower trunk of brachial plexus Vessels - Subclavian artery touching outer border of rib - Subclavian vein - Under is the costal groove is the neurovascular bundle of first intercostal space Other - The cervical pleural and apex of lung 2010-2, 2009-2, 2005-1 (CXR) Describe the surface anatomy of the parietal pleura. Posteriorly - Small section medially are inferior to the 12th rib - Parallel to vertebral column to T1 - Cupola rises 2-3 cm above medial 1/3 of clavicle to the level neck of the 1st rib (but not above it) What is the clinical significance of the attachment of the pleura? 2010-2 - Cervical pleura may be injured, e.g. subclavian or IJ line insertion or penetrating injury to neck - Deviation of pleura to the left provides a window for pericardiocentesis without traversing the pleura - The attachment of the pleura at a lower level than the lungs (posterolaterally) favours collection of pleural fluid in this area (drainage, clinical findings) - Penetrating injuries to the upper lumbar region (Mnemonic: 2-4-6-8MCL-10MAL-12PAL) 2009-2 How does surface anatomy of the lung compare to that of the pleura? - Assuming quiet respiration… - Lungs: 2 ribs higher below the 6th rib/at MAL and posteriorly - The costodiaphragmatic recesses are not occupied by lung and thus fluid will accumulate here 2010-2, 2008-2, 2008-1, 2007-1, 2005-2, 2004-2 (great vessels and ligamentum arteriosum) Model of Heart (Somso HS1) Identify the chambers and valves of the heart on this model Demonstrate the chambers of the heart and their borders 2008-1 - Atria are separated from the ventricles externally by the coronary sulcus (AV groove) - Internally by the fibrous skeleton (rings and trigone) that provides attachments and insulates - Left and right ventricles demarcated by the anterior and posterior interventricular (IV) sulci - The crux is where the coronary sulcus and posterior IV sulci meet Demonstrate where the major components of the conducting system would be found - SA-node: Ant-lat near junc of SVC and RA - AV-node: Post-inf interatrial septum near coronary sinus opening - AV bundle of His: via the fibrous skeleton of the heart, along the membranous part of the inter-ventricular septum - Right and left bundles: pass on each side of the muscular IV septum 2005-2 Identify the structural components of the tricuspid valve. 1. 3 cusps (ant, post and septal attached to fibrous A-V ring) 2. Chordae tendinae 3. Papillary muscles Identify the main features of the right atrium POINTS REQUIRED 1. SVC 2. IVC 3. Auricle 4. Coronary sinus 5. Fossa ovalis (remnant of foramen ovale) Identify the Ligamentum Arteriosum What is the role of the ductus arteriosus in the foetus? POINTS REQUIRED 1 Bypasses Lungs – deoxygenated blood from head – BCVs – RA – RV – Pulmonary Trunk – DA – Aorta – Umbilical Artery - Placenta – Reoxygenated 2010-1, 2008-1, 2007-1, 2006-1 Using this model, describe the arterial supply of the heart - Main coronary vessels arise from corresponding aortic sinus above aortic valve RCA in (R)AV groove gives off: - SA nodal to supply SAN (in 60%) - (R) atrial - (R) marginal - Post interventricular (in 2/3) which supplies post 1/3 of IV septum - AV nodal (in 80%) Supplies: RA, most of RV, inferior surface of heart (diaphragmatic part of LV), post 1/3 septum, and more commonly the SA (60%) and AV (80%) nodes LCA in (L)AV groove bifurcates: - Circumflex - LAD (anterior I-V artery) to supply the ant 2/3 of IV septum - Circ gives off left marginal branch - LAD gives off lateral diagonal Supplies: LA, most of LV, ant 2/3 IV septum (more of His and Purkinje), less commonly the SA or AV nodes Demonstrate the venous drainage of the heart - Major drainage is via the Coronary sinus - 3 main tributaries are 1. Great cardiac vein (accompanies LAD, then Circ) 2. Middle cardiac vein (accompanies PIV) 3. Small cardiac veins (accompanies R marginal) - Oblique vein (L) atrium marks start of sinus - Ant cardiac veins start ant surface RV, drain straight into RA - Smallest cardiac veins (venae cordis minimae, Thesbian veins) drain direct into chambers 2006-1 Describe the arterial supply to the cardiac conduction system 1. SA node: RCA 60%, LCA via Circumflex 40% 2. AV Node: RCA 80% 3. AV bundle of His Purkinje fibres – LCA via LAD 2011-1, 2009-2, 2009-1, 2007-2, 2006-2, 2004-2 (great vessels on model), 2003-2 Photo: Thoracic inlet. Major vessels and relationships Identify the vascular structures in this photo (pg 210) Veins: Arteries: Superior vena cava (26) Brachiocephalic trunk (4) Thyrocervical trunk (32): L (13) and R (18) brachiocephalic v. Right common carotid a. (19) Inferior thyroid art. (6) Left and right subclavian v. (24) Left common carotid a. (14) -> Ascending cervical art (3) Left internal jugular vein (8) Right subclavian artery (21) Transverse -> Superficial cervical a. (25) Inferior thyroid veins (7) Internal thoracic a. (9) Suprascapular a. (27) Nerves: Upper trunk BP (35), phrenic (17), vagus (R=22, L=15), right recurrent laryngeal (20) Others: Thyroid (12), cricoid (2), trachea (33), thymus (31), parietal pleura (16) What are the posterior relations of the thyroid gland? 2009-2 Cricothyroid membrane, trachea, right and left common carotid arteries laterally Describe the course of the right subclavian artery 2009-1, 2005-1 - Arises from brachiocephalic trunk - Runs posterior to right sternoclavicular joint as ascends through thoracic inlet - Arches superolaterally and passes posterior to anterior scalene muscle - Relationship to this muscle defines its 3 parts - Descends posterior to middle of clavicle and crosses over 1st rib to become axillary artery Name the branches of the subclavian artery 1st Part - Verterbral artery - Internal thoracic a - Thyrocervical trunk nd 2 Part - Costocervical trunk 3rd Part - Dorsal scapular (Mnemonic: Vit C&D, and Tits for thyrocervical) 2006-2 Name branches of the thyrocervical trunk - Inferior thyroid a. - Transverse cervical a. (-> superficial +/dorsal scapular a) - Suprascapular a. 2007-2 Describe the branches of the descending thoracic aorta Posterior intercostal arteries, paired x9, run laterally Bronchial, 1-2 branches, usually paired laterally Medisatinal Oesophageal, unpaired 4-5 branches anteriorly Subcostal Superior phrenic Subphrenic