Cell Quiz Review
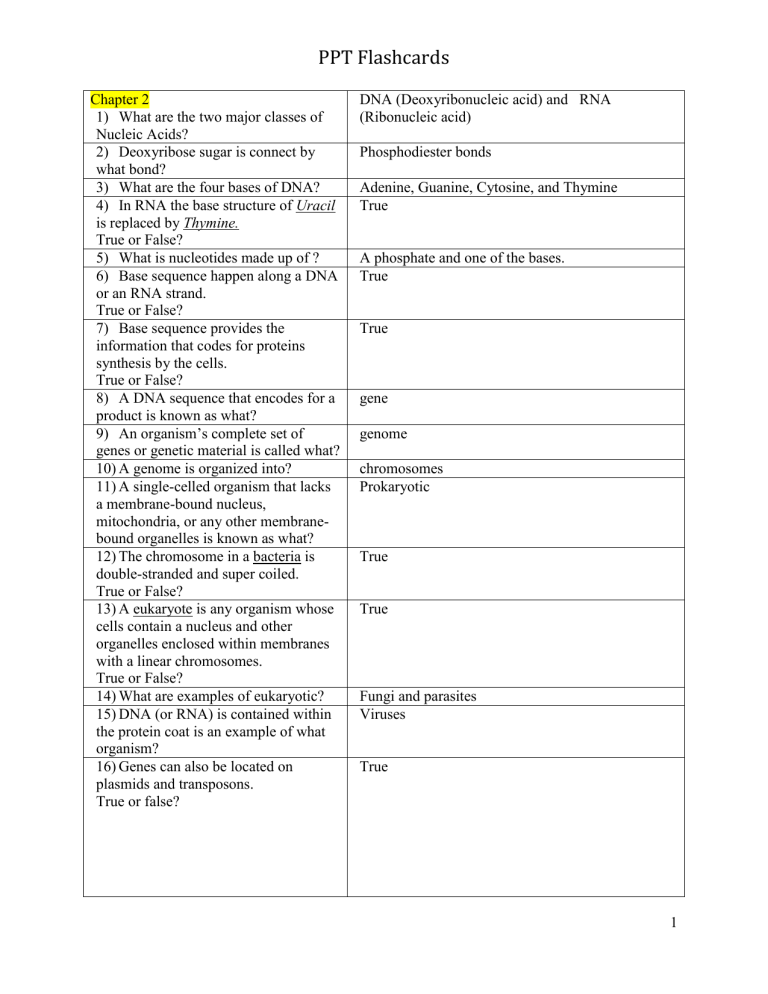
PPT Flashcards
Chapter 2
1) What are the two major classes of
Nucleic Acids?
2) Deoxyribose sugar is connect by what bond?
3) What are the four bases of DNA?
4) In RNA the base structure of Uracil is replaced by Thymine.
True or False?
5) What is nucleotides made up of ?
6) Base sequence happen along a DNA or an RNA strand.
True or False?
7) Base sequence provides the information that codes for proteins synthesis by the cells.
True or False?
8) A DNA sequence that encodes for a product is known as what?
9)
An organism’s complete set of genes or genetic material is called what?
10) A genome is organized into?
11) A single-celled organism that lacks a membrane-bound nucleus, mitochondria, or any other membranebound organelles is known as what?
12) The chromosome in a bacteria is double-stranded and super coiled.
True or False?
13) A eukaryote is any organism whose cells contain a nucleus and other organelles enclosed within membranes with a linear chromosomes.
True or False?
14) What are examples of eukaryotic?
15) DNA (or RNA) is contained within the protein coat is an example of what organism?
16) Genes can also be located on plasmids and transposons.
True or false?
DNA (Deoxyribonucleic acid) and RNA
(Ribonucleic acid)
Phosphodiester bonds
Adenine, Guanine, Cytosine, and Thymine
True
A phosphate and one of the bases.
True
True gene genome chromosomes
Prokaryotic
True
True
Fungi and parasites
Viruses
True
1
PPT Flashcards
17) Double-stranded “miniature” chromosome that is made up of several genes that mediate replication and transfer or encode for products with a special function is an example of what nonchromosomal elements?
18) Pieces of DNA that move between genetic material is an example of what nonchromosomal elements?
19) Chromosomal DNA are relaxed.
Strands of DNA are separated.
New strands are synthesized on the replication forks.
Completion is terminated when the two forks meet (one parent, one daughter).
Above is an example of what process?
20) What two sub-unit make up Gene
Expression?
21) What is the term that explain the process of DNA base sequence is converted into messenger RNA
(mRNA), while RNA polymerase identifies where transcription is initiated?
22) What is the term that describe the genetic code mRNA is translated into specific amino acid sequences with the help of transfer RNA (tRNA) and ribosomal RNA (rRNA)?
23) Single-Celled Organism uses complex mechanisms to respond and adapt to environmental challenges.
True or False?
24) Regulation allow the organism to do what?
25) Genes that encode anabolic enzymes are repressed in the presence of an end product.
Genes that encode catabolic enzymes are induced when the substrate is present.
These are describing what?
Plasmids
Transposons
Replication
Transcription and Translation
Transcription
Translation
True
Control the transfer of information
Transcriptional (genetic control)
2
PPT Flashcards
26)
The definition of “Translational” express how enzyme production is controlled at the protein synthesis level.
True or False?
27) What is the term that describes regulation of enzymes is already synthesized?
28)
An alter in the organism’s genotype is known as what?
29) Genetic Recombination describes how segment of DNA from original bacteria enters a second cell where
DNA is exchanged.
True or False?
True
Posttranslational
Mutation
True
30) Free DNA fragments recombine with the recipient’s DNA is explaining what process?
31) DNA is integrated into the recipient’s DNA via a bacteriophage is explaining what process?
Transformation
Transduction
32) When DNA is transferred between two living cells is explaining what process?
33) What are some examples of
Conjugations?
Conjugation
1.
Sex Pilus
2.
Plasmids and Transposons
34) Example of an acquisition of nutrients for metabolism?
35) Acquisition of nutrients such as water,oxygen, and carbon dioxide is an
1.
Simple Diffusion
2.
Active Transport
Simple diffusion example of what type of acquisition?
36) Acquisition of nutrients such as sugars, amino acids, and inorganic ions are example of what type of acquisition?
37) An example of production of precursor metabolites?
38) What is created during energy production in metabolism?
Active Transport
Pentose phosphate shunt
ATP (adenosine triphosphate)
39) Substrate-level phosphorylation is an example of what pathway?
40) Oxidative phosphorlation is an example of what type of respiration?
41) What is the term that describe the use of precursor products to produce a variety of building blocks?
Fermentative pathway
Aerobic Respiration
Biosynthesis
3
PPT Flashcards
42) The building blocks into macromolecules is called what?
43) Cellular structure are the product of all genetic and metabolic processes.
True or False?
44) The following are example of which type of cells?
Fungi and Parasites
Single or Multicellular
Membrane-enclosed organelles
Endoplasmic reticulum
Golgi body
Mitochondria
Lysosomes
Nucleus
45) The following are example of which type of cells?
Bacteria
Singled-celled
Do NOT contain organelles
Cell wall made of peptidoglycan
46) Bacteria range in size from 0.25 – 1 μm in width and 1 to 3 μm in length.
True or False?
47) In a gram stain procedure what color will the bacterial cell wall stain if the organism is gram-positive organism?
48) In a gram stain procedure what color will the bacterial cell wall stain if the organism is gram-Negative organism?
49) Refering to the common shape of bacteria, what shape does Cocci express?
50) Refering to the common shape of bacteria, what shape does Coccobacili express?
51) Refering to the common shape of bacteria, what shape does Bacillus express?
52) Refering to the common shape of bacteria, what shape does Fusiform express?
53) Refering to the common shape of bacteria, what shape does Curved express?
54) Refering to the common shape of bacteria, what shape does Spiral express?
55) Refering to the common shape of bacteria, they can all appear as singles, pairs or groups
(tetrads). True or False?
Polymerization
True
Eukaryotic
Prokaryotic
True
Purple color
Pink color
Circular
Ovoid
Rod-shaped
Pointed-end
Curved
Spiral
True
4
PPT Flashcards
56) Gram-positive cell contains a thick layer of peptidoglycan. True or False?
57) Gram-Negative cell contain a thin layer of peptidoglycan. True or False?
58) Acid Fast contains waxy substances.
True or False?
66) What is the mode of interaction between
Human and Microbe?
67) How animal can be a microbial reservoir?
True
True
True
59) What does Periplasm (gram-negative) contains?
60) The Deepest layer of the cell is known as the what?
Gel-like substance and enzymes
Cell membrane
61) What does the cell membrane contain?
62) How does the cell membrane help the cell
Proteins and enzymes
Serves as osmotic barrier function?
63) What are the structure and substance that are bound internally?
Cytosols
Plysomes
Inclusions
Nucleoids
Plasmids
Endospores
Humans, animals, water, air, and soil Chapter 3
64) What are microbial reservoirs?
65) What can transmit microbe? Vectors (living) and fomites (nonliving)
Direct (birth), indirect
68)
69)
How insects act as vector in transmitting?
How does environment act as a Microbial
Reservoir?
70) What does first lines of defense in the host include?
71) Where mucous membrane can be found?
Agents are transmitted directly (e.g., animal bite) or indirectly (e.g., insect vectors).
It transmits viral, parasitic, and bacterial disease.
Microorganisms can be acquired by inhalation or through wounds.
Skin and skin structures
Mucous membranes
Mouth and oral cavity
Gastrointestinal tract
Upper respiratory tract
Urogenital tract
72) What is normal flora?
73) Does transient colonizers multiply?
74) Does resident flora multiply?
75) What are the certain condition that microbes must survive to colonize the host surface?
Microbes that inhabit the body
No
Yes
Survive environmental conditions.
Attach and adhere to host cell surfaces.
Produce substances that compete for host nutrients.
Coexist with other microorganisms
5
PPT Flashcards
76) What does Disruption of Host Barriers include?
Trauma
Inhalation
Implantation of Medical Devices
Diseases
Childbirth
Overuse of Antibiotic Medications
77) How many types of trauma are there?
78) How many types of Diseases are there?
79) What are the soluble components of immune system?
80) What are the two types of Adaptive Immune
Responses?
81) What does Antibody-Mediated do?
Two: Wounds , Burns
Three: Malignancies, Diabetes, Alcoholism
Antibodies (immunoglobulin [Ig] G, A, M,
D, E) Antigens
Antibody-Mediated (also called Humoral
Immunity )
Cell-Mediated (also called Cellular
Immunity)
•
B cells and antibody production.
•
Mediated by helper T cells.
•
Release Cytokines.
82) What does Cell-Mediated do? Involve T-cell interaction with antigenpresenting cells.
+Macrophages
+B lymphocytes
83) What are pathogens?
84)
85)
86)
What are Virulent Factor?
What are Opportunistic Infection?
What does Virulent Factor include?
They are Microorganisms that cause infections
Characteristics that help microorganisms cause disease
Infections that occur when one or more of the host’s defense mechanisms are disrupted
Attachment—Outcompete colonizers
•
Invasion—By traumatic factors or by direct action of virulence factors
•
Survival against Inflammation—By avoiding phagocytes and the complement system
•
Survival against the Immune System
•
Toxin Production
87) What type are Toxin Productions?
88) What does the Outcome of Infectious Disease depend on?
_Endotoxins: released by gram-negative bacteria
_Exotoxins: produced by gram-positive bacteria
State of host’s health
Virulence of the pathogen
Whether host can clear pathogen
6
PPT Flashcards
89)
90)
What types of Infections are there?
91) What types of Immunization are there?
92) What is Active Immunization?
93)
94)
What are the strategies to Prevent infectious disease?
What is Passive Immunization?
What is Epidemiology?
Chapter 4
95) What process kills all forms of life?
96) Which of the following are used for sterilization?
A.
Boiling, pasteurizing, UV light
B.
Alcohols, aldehydes, phenolic compounds
C.
Incineration, moist or dry heat, filtration, gamma radiation
D. All of the above
97)
98)
99)
Which process destroys most pathogenic organisms?
What is an antiseptic?
List the factors that influence the activity of disinfectants?
100) How can hazardous waste be reduced?
A.
Shredding or compacting with chemicals
B.
Thermal decontamination
C.
Radiation
D.
All of the above
101) How is infectious waste disposed of?
102) Tubes and reagents should be disposed of in _____________?
103) Pipettes, swabs, & glass should be disposed of in _____________?
104) Broken glass should be disposed of in
_____________?
105) Scalpels and needles should be disposed of in _____________?
Acute—Develops quickly
Chronic—Develops slowly
Latent—Silent phase with no symptoms
Prevents transmission.
Controls microbial reservoirs.
Minimizes risk before and after exposure.
2 types: Active , Passive
Modified antigens introduced into the body.
Are long lasting
Antibodies transferred to the host for temporary protection
Is the science that characterizes the circumstances associated with the acquisition and dissemination of infectious diseases
Sterilization
C. Incineration, moist or dry heat, filtration, gamma radiation
Disinfection
Disinfectant used on living tissue
Temperature, pH, the type and number of organisms, the concentration of disinfectant, amount of organic material, nature of surface to be disinfected, length of contact time, and type of water available
D. All of the above
Autoclaved or incinerated
Two leak proof plastic bags
Rigid cardboard containers
Boxes lined with bags
Sharps container
7
PPT Flashcards
106) A chemical hygiene plan is required for every lab. True or False
107) What plan contains the following: guidelines on labeling containers, SDSs, and written chemical safety training and retraining programs?
108) SDSs must contain which of the following:
A.
Information on the nature of the chemical.
B.
Precautions if the chemical is spilled.
C.
Disposal recommendations.
D.
All of the above
True
Chemical Hygiene Plan
D. All of the above
109) What type of fire extinguisher is used for trash, wood, and paper?
110) What type of fire extinguisher is used for chemical fires?
111) What type of fire extinguisher is used for electrical fires?
112) What type of fire extinguisher is a
Type A
Type B
Type C
Type ABC combination extinguisher?
113) What type of plan identifies tasks that are hazardous and promote safety?
114) Which plan includes appropriate disposal of hazardous waste, PPE, and a postexposure plan?
115) Standard precautions require that blood
Exposure control plan
Exposure Control Plan
Potentially infectious and body fluids from every patient be treated as?
116) List 5 examples of standard precautions. Do not eat, drink, smoke, or apply cosmetics
Do not insert or remove contact lenses
Do not mouth pipette
Thoroughly wash hands
Attempt to avoid injuries with sharp objects
117) Which biosafety level has no potential for infection?
118) Which biosafety level includes common agents of disease?
119) Which biosafety level has organisms that are transmitted by aerosol?
120) Which biosafety level includes exotic agents, maximum containment is required.
Biosafety level 1
Biosafety level 2
Biosafety level 3
Biosafety level 4
8
PPT Flashcards
121) Matching:
Salmonella
Mycobacterium tuberculosis
Bacillus subtillis
Marburg virus
Choices:
133) What are some conditions for rejecting a specimen?
Salmonella – Biosafety level 2
Mycobacterium tuberculosis – Biosafety level 3
Bacillus subtillis – Biosafety level 1
Marburg virus – Biosafety level 4
Biosafety level 1
Biosafety level 2
Biosafety level 3
Biosafety level 4
122) Which infectious agent shipping classification causes disease in humans and
Category A animals?
123) Which infectious agent shipping classification includes biological substances?
Category B
124) Chapter 5
125) Name a Collection technique used on
Clear instructions should be given to the patient, if he or she is collecting their own patients specimen
126) When should specimen collection occur?
During the acute phase of a patient’s illness
127) How should specimens be transported? Specimens should be transported in leakproof biohazard labeled bags.
128) How soon should specimens be transported to the lab?
129) Why are preservatives used in specimen collection?
130) Why are anticoagulants used in specimen collection?
131) At what temperature should specimens not immediately process be refrigerated at?
132) What information should be contained on a specimen requisition order?
Within 2 hours of time from collection
To maintain colony counts without encouraging further growth
To prevent clotting of the patient’s blood
4 degrees Centigrade
Patient’s name, age (date of birth), sex, and hospital number, the ordering physician, site, date and time of collection.
Specimen is improperly labeled, transported, is leaking, dried, in a fixative, collected on the wrong media, or the quantity collected is insufficient
134) What are some of the steps involved in processing a specimen upon arrival at the lab?
135) What are the reasons for directly examining a specimen microscopically?
The receiving time and date is documented, the specimen is grossly examined and cultured, status and priority is determined, it is directly examined microscopically.
To assess quality of the specimen, gain an early indication of what is wrong with the patient, observe the smear for later comparison with what is cultured.
9
PPT Flashcards
136) Name the different types of culture media. Nutritive, differential, selective, back-up broth
137) What is a differential culture media? One that differentiates organisms based on specific characteristics
138) What is the difference between a Nutritive and a selective culture media?
A nutritive culture media supports the growth of a wide range of organisms, while a selective culture media supports the growth of only one group of organisms.
Sheep’s blood agar and chocolate agar
139) Give two examples of Nutritive culture media
140) When is back-up broth used? In conjunction with solid media and to detect a small number of organisms.
141) What are anaerobes?
142) What are aerobes?
Microorganisms that cannot grow in an oxygen environment
Microorganisms that grow in ambient air
(require 21% oxygen and 0.03% carbon dioxide)
143) True or false, Capnophiles are microaerophiles?
144) What are microaerophiles?
True.
Microorganisms that grow under reduced oxygen and increased carbon dioxide conditions.
145) True of False, most medically important bacteria are facultative anaerobes?
True.
Chapter 6
146) What is the use of a microscope to magnify objects too small to be visualized with the naked eye?
147) One function that microscopy is useful for includes what?
148) Another function of microscopy is?
Microscopy
Directly detects microorganisms in clinical specimens
Characterizes organisms growing in culture.
Bright-Field Microscopy 149) Visible light passes through the specimen and through a lens that results in the magnification of the organism occurs in what kind of microscopy?
150) What are the three main principles of bright-field microscopy?
151) For magnification, the 10x, 20x, 40x, and
100x magnifications describe what part of the microscope?
152) The ocular lens is what magnification?
153) Detail of the magnified object can be observed in which principle of bright-field microscopy?
Magnification, resolution, and contrast
Objective lenses
10x
Resolution
10
PPT Flashcards
154) What method is used to increase resolution?
155) Which bright-field microscopy principle allows objects to stand out from the background?
156) What provides the maximum illumination and resolution?
157) What properly positions the condenser to ensure that light is focused through the specimen?
158) Beams of light pass through a specimen to create different light intensities and greater contrast in what kind of microscopy?
159) Staining is not necessary in what kind of microscopy?
160) What can be observed in phase contrast microscopy?
161) Phase contrast microscopy is most useful in observing what in a culture?
162) Fluorochromes are raised to higher energy levels after excitation in which microscopy?
163) Excess energy is released in the form of visible light when molecules return to a normal state in which microscopy?
164) In fluorescent microscopy, how to objects appear?
165) Which microscopy directs light at an oblique angle to achieve contrast?
166) Only light that hits the object will be visualize in what type of microscopy?
167) Which type of microscopy uses electrons instead of light to visualize small objects?
168) In electron microscopy electromagnetic fields are focused by what?
169) In electron microscopy, magnification is in excess of how much?
170) What stain is the principle stain used for the examination of bacteria?
171) Clinical material is fixed to a slide before staining on what type of stain?
172) Primary stain is made of what?
173) Mordant is made of what?
174) Decolorizer is what type of chemical?
175) Counterstain is made of what?
176) On a Gram stain, what type of organism will stain deep purple?
Oil Immersion
Contrast
Köhler Illumination
Köhler Illumination
Phase Contrast Microscopy
Phase Contrast Microscopy
Living Organisms
Fungi
Fluorescent Microscopy
Fluorescent Microscopy brightly lit against a dark background.
Dark-Field Microscopy
Dark-Field Microscopy
Electron Microscopy
Electrons
100,000x
Gram stain
Gram stain
Crystal violet
Gram's iodine alcohol
Safranin
Gram-positive
11
PPT Flashcards
177) On a Gram stain, what type of organism will stain pink to red?
178) What stains Are used to detect bacteria whose cell walls contain mycolic acids (e.g.,
Mycobacterium)?
179) What two methods are used in acid fast staining?
180) Primary stain enters the cell wall by heating in which acid-fast stain?
181) Primary stain contains phenol (cold method) in which acid-fast stain?
182) What organisms will stain pink
(carbolfuchsin)?
183) what are the colors of the counterstains in an acid-fast stain?
184) Fluorochromes retain which 3 stains?
Gram-negative
Acid-Fast Stains
Ziehl-Neelsen stain and Kinyoun stain
Ziehl-Neelsen stain
Kinyoun stain
Acid-fast organisms
Blue (methylene blue) and Green
(malachite green)
Acridine orange stain, Calcofluor white stain and Auramine-rhodamine stain
Acridine orange stain 185) Which fluorochrome stain stains nucleic acid and is nonspecific?
186) What is the function of Acridine orange stain?
Confirms the presence of bacteria in blood cultures when blood cultures are indeterminate.
Calcofluor white stain 187) Which fluorochrome stain greatly enhances fungal visibility in tissue and in other specimens?
188) Which fluorochrome stain nonspecifically will bind to nearly all mycobacteria?
189) Cells appear bright yellow or orange against a green background on which fluorochrome stain?
Chapter 7
190) What is bacterial growth required for?
191) What are the purposes of bacterial cultivation?
Auramine-rhodamine stain
Auramine-rhodamine stain
For identification and characterization
- Grow and isolate all bacteria present in a clinical specimen.
- Determine bacteria that are most likely causing infection and which are likely the contaminants.
- Obtain sufficient growth of clinically relevant bacteria to allow identification and characterization.
12
PPT Flashcards
192) What are the types of bacterial media?
193) What are the environmental requirements which sustain bacteria growth?
194)
195)
196) identification?
What are the types of bacterial
What is genotypic criteria?
What is phenotypic criteria?
Enrichment—Contains specific nutrients for the growth of particular pathogens.
- Buffered charcoal-yeast extract agar and thioglycollate broth
Nutritive—Supports growth of the most nonfastidious organisms.
- Tryptic soy agar
Selective—Inhibits all organisms except those “selected.”
- May contain bile salts, dyes, and antibiotics
- Phenylethyl alcohol agar
Differential—Allows colonies of one species to be differentiated from other bacteria growing on the plate.
- MacConkey agar (differential and selective)
Oxygen and carbon dioxide availability
- Most clinically significant organisms are facultatively anaerobic.
Temperature
- Bacterial pathogens multiply best at the internal human temperature. pH
- Most clinically relevant bacteria prefer a near neutral pH (6 to 7.5).
Moisture content
- Agar plates are sealed to trap moisture.
- Humidified incubators are used to maintain moisture levels.
- Genotypic criteria
- Phenotypic criteria
- Bacterial genome is characterized using molecular techniques.
- Presence of a specific gene definitively identifies the organism.
Observable physical characteristics include:
- Microscopic morphologic and staining characteristics
- Colonial morphologic characteristics
Metabolic characteristics include:
- Environmental requirements for growth
- Susceptibility results to antimicrobial agents
- Nutritional requirements and metabolic capabilities
13
PPT Flashcards
197)
204)
205)
206)
207)
What are the enzymatic tests?
What are the metabolic pathways?
What are the characteristics of carbohydrate oxidation and fermentation?
What determines amino acid degradation?
What are single substrate uses for?
- Catalase
- Oxidase
- Urease
- Indole
- Pyrrolidonyl arylamidase (PYR)
- Hippurate hydrolysis
198)
199) test?
What are the characteristics of catalase
What are the characteristics of oxidase test?
- Differentiates staphylococci from streptococci
- Catalase catalyzes water and oxygen from hydrogen peroxide.
- Differentiates groups of gram-negative bacteria.
- Oxidase is indicated when it reacts with
1% tetra-methyl-p-phenylenediamine dihydrochloride
200) What are the characteristics of urease test?
- Helps identify some members of the
Enterobacteriaceae family.
- Urease hydrolyzes urea into ammonia, water, and carbon dioxide.
201) What are the characteristics of indole test? - Presumptively identifies Escherichia coli.
- Tryptophanase degrades tryptophan into pyruvic acid, ammonia, and indole.
202) What are the characteristics of pyrrolidonyl arylamidase (PYR) test?
203) What are the characteristics of hippurate hydrolysis test?
- Identifies Streptococcus pyogenes
Enterococcus sp.
- 1-pyrroglutamyl-aminopeptidase hydrolyzes PYR to produce
β-naphthylamine. and
- Identifies Gardnerella vaginalis ,
S .
agalactiae , Campylobacter jejuni , and
Listeria monocytogenes .
- Hippuricase hydrolyzes hippurate to produce glycine (deep purple color).
- Carbohydrate oxidation and fermentation
- Amino acid degradation
- Single substrate uses
- Oxidative processes require oxygen; fermentative processes do not.
- Oxidative-fermentative medium is used.
- Determines the ability of bacteria to produce enzymes that:
- Deaminate (occurs in air).
- Dihydrolyze.
- Decarboxylate (anaerobic process).
Organism is inoculated on citrate, malonate, or acetate and observed for growth or detection of metabolic end products.
14
PPT Flashcards
208)
209)
210)
211)
216)
217)
What are the basic components of test systems? substrate utilization?
What is the purpose of detection of metabolic activity (substrate utilization)?
What is the purpose of selection and inoculation of tests?
What is the purpose of incubation and
212) What is the purpose of metabolic profiles?
Chapter 11
213)
214)
215) actively inhibiting or killing them? agents are obtained?
Which substances eradicate organisms by
How the antibiotics as antimicrobial
What is bacteriostatic?
What is bactericidal?
What are the targets of antimicrobial agents on the organisms?
- Selection and inoculation of tests
- Incubation for substrate utilization
- Detection of metabolic activity (substrate utilization)
- Analysis of metabolic profiles
- Number and type of tests selected depend on type of organism to be identified, clinical significance of isolates, and availability of reliable methods
- Identification systems must be inoculated with pure cultures
- Duration depends on whether bacterial multiplication is or is not required for substrate utilization (i.e., growth-based test vs. a non-growth-based test)
- Colorimetry, fluorescence, or turbidity are used to detect products of substrate utilization
- Detection is done visually or with the aid of various photometers
- Involves conversion of substrate utilization profile to a numeric code (see figure 7-18)
- Computer-assisted comparison of numeric code with extensive taxonomic data base provides most likely identification of the bacterial isolate
- For certain organisms for which identification is based on a few tests, extensive testing and analysis are not routinely needed
Antimicrobial agents that are a group of natural and synthesized substances that target organisms.
Antibiotics are obtained and purified from other microbial organisms.
Antimicrobial agents that inhibit bacterial growth but generally do not kill the organism are known as bacteriostatic.
Antimicrobial agents that usually kill target organisms are said to be bactericidal.
Cell Wall
DNA and RNA Synthesis
Metabolic Pathways
Protein Synthesis
Cell Membrane
15
PPT Flashcards
218)
219) What is the chemical principle for the mechanism of betalactam antimicrobial agents?
220) By what mechanism an organism become resistant to beta-lactam antimicrobial agents?
221)
222)
223)
224)
225)
226)
227)
228)
229) antimicrobial agents? of microorganisms mechanisms of glycopeptide agents?
Why glycopeptide agents are ineffective for most gram-negative?
What is the function of cell membrane inhibitors?
What are the other methods of resistance
Why cell membrane inhibitors are more effective against gram-negative bacteria than to gram-positive bacteria?
What is the basic structure of beta-lactam
List the beta-lactamase classes.
What are glycopeptides?
What is the peptidoglycan?
What is the chemical principle for the
What is the action of Polymyxin antibiotics?
Beta-lactam antimicrobial agents contain a four-membered, nitrogen-containing ring at the core.
Beta-lactam antimicrobial agents bind the enzyme inhibiting transpeptidation and inhibit cell wall synthesis.
A common mechanism for resistance to beta-lactams is the production of enzymes
(e.g., beta-lactamases)
Beta-lactamase classes:
Class A—Serine peptidases
Class B—Metallo-β-lactamases
Class C—Cephalosporinases
Class D—Serine peptidases
Genetic mutations with the penicillinbinding proteins (PBPs)
Genetic recombination
Overproduction of normal PBP
Glycopeptides are the other major class of antibiotics that inhibit bacterial cell wall synthesis
Bacterial cell wall or murein layer that gives the bacterial cell shape and strength to withstand changes in environmental osmotic pressures. glycopeptide agents bind to the end of the peptidoglycan, interfering with transpeptidation.
Inhibit cell wall synthesis and growth. glycopeptide agents are large and cannot penetrate gram-negative outer membrane to reach cell wall layer well.
They disrupt bacterial cell membrane, similar to detergents: interact with phospholipids to increase permeability.
Results in leakage of macromolecules and ions to cause cell death.
The membrane of gram- positive is protected with a thicker peptiodoglycan or murein layer, compare to gram-nagative that its outer membrane is exposed to the action of inhibitors of cell membrane
Polymyxin antibiotics (Polymyxin B and
Colistin) are cyclic polypeptide agents that disrupt bacterial cell membrane, and act as detergents.
16
PPT Flashcards
230)
231) antibiotics?
How is the effictiveness of polymyxin
Why polymaxin antibiotics may be used as an agent of last resort for Pseudomonas aeruginosa and Acinetobacter spp.
Their effectiveness varies with the molecular makeup of the bacterial cell membrane.
They are more effective against gram-negative bacteria than gram-positive, because of easier access to the cell membrane of gam-negative
These antibiotics are effective as an inhibitors cell membrane. They are used when gram-negative are resistant to all other available agents are encountered.
Pseudomonas aeruginosa is a gramnegative rod, and
Acinetobacter spp. are gram-negative cocci.
Humane host cells also have membranes, therefore polymyxine pose a risk of toxicity. The major side effects are neurotoxicity and nephrotoxicity.
Target protein synthesis and severely disrupt cellular metabolism.
They bind 30S OR 50s ribosomal subunits
232) What is the function of the inhibitors of protein synthesis
233) What is the chemical principle for the mechanisms of protein synthesis inhibitors
234)
235)
236)
237)
How binding to 30S ribosomal subunit interrupts protein synthesis by
Aminoglycosides and aminocyclitols? interrupts protein synthesis by Macrolidelincosamide-streptogramin group (MLS)?
How binding to 50S ribosomal subunit
Which other inhibitors of protein synthesis bind to 30S ribosomal subunit?
Which other inhibitors of protein synthesis bind to 50S ribosomal subunit?
This process interrupts several steps, including initial formation of the protein synthesis complex, accurate reading of the messenger RNA (mRNA) code, and formation of the ribosomal-mRNA complex
Protein synthesis is inhibited by drugs binding to the 23sRNA on the bacterial 50S ribosomal subunit and subsequent disruption of the growing peptide chain by blocking of the translocation reaction.
Tetracyclines
Glycylglycines
Ketolides
Oxazolidinones
Chloramphenicol
Fluoroquinolones and Metronidazole 238) What are two primary antimicrobial agents that target DNA metabolism?
239) How fluoroquinolones and Metronidazole act on DNA synthesis?
-Fluoroquinolones
Bind to and interfere with DNA gyrase enzymes.
Newer quinolones inhibit topoisomerase IV
(similar to DNA gyrase).
-Metronidazole
Nitro group is reduced in bacterial cytoplasm, generating cytotoxic compounds that disrupt DNA.
17
PPT Flashcards
240)
241)
242)
243)
244)
245)
246)
247) synthesis and how?
What antibacterial agent inhibit RNA
What is the action of Sulfonamide? bacteria to effect resistance to antimicrobial agents?
What is the action of Trimethoprim?
What is the action of Nitrofurantoin?
What is the intrinsic resistance?
What is the acquired resistance?
What are the pathways or strategies of
In term of evolution what is the meaning of antibacterial resistance of the microorganisms?
Rifamycin
Binds to DNA-dependent RNA polymerase and inhibits RNA synthesis.
Sulfonamide
Inhibits dihydropteroate synthase in the folic acid pathway.
Trimethoprim
Inhibits dihydrofolate reductase in the folic acid pathway.
Nitrofurantoin
Drug intermediates bind to bacterial ribosomal proteins and ribosomal RNA
(rRNA).
Antimicrobial resistance resulting from the normal genetic, structural, or physiologic state of a microorganism is referred to as intrinsic resistance. Resistance Inherited characteristics are associated with the vast majority of strains in a particular bacterial group, genus, or species.
Antibiotic resistance resulting from altered cellular physiologic structure caused by changes in a microorganism’s usual genetic makeup is known as acquired resistance
-Enzymatic destruction or alteration of the antibiotic
-Decreased intracellular uptake or accumulation of drug.
-Altered antibiotic target
With the introduction of the antibiotics into medical practice, clinically relevant bacteria have adopted resistance mechanism as part of their survival strategy. As a result of the increased use of antimicrobial agents, a survival of the fittest strategy has been documented as bacteria adapt to the pressures of antimicrobial attack. standardization Chapter 12
248) To optimize bacterial growth conditions to ensure that the inhibition of growth can be attributed to the antimicrobial agent
249) To optimize conditions for maintaining antimicrobial integrity and activity, attributing the failure to inhibit bacterial growth to organism-associated resistance standardization
18
PPT Flashcards
250) To maintain reproducibility and consistency in the resistance profile of an organism, regardless of what laboratory performs the test
251) ____________are compared with the turbidity of the organism suspension
252) _____________ is often used for susceptibility testing
253) ______challenges the organism of interest with an antimicrobial agent in a liquid environment
254) Dilution totaling .05-.1mL
255) volume greater than 1mL
256) Medium for broth dilutions
Dilution
257) Temperature for broth dilutions
258) Incubation duration for broth dilutions
259) The well with the lowest concentration that inhibits growth is called?
260) An organism is ________ to a antimicrobial agent if it inhibits the growth of an organism
261) An organism is ______to a antimicrobial agent if the agent is ineffective
262) The specific concentrations that separate or define the different categories of the MIC are called
263) In ________,Antibiotic disks of known concentrations are placed on the surface of an agar plate that has been seeded with a lawn of bacteria (0.5 McFarland turbidity standard).
264) In disk Diffusion what agar is the standard medium
265) In _______antimicrobial concentrations and organism are brought together on an agar based medium
266) Commercially available panels contain dry lyophilized agents for which susceptibility test
267) Instruments apply an antimicrobial agent to the agar in susceptibility test
268) Strips containing an antimicrobial agent generate MIC data
269) Disk diffusion is digitally analyzed standardization
McFarland Standard
0.5 McFarland turbidity standard
Broth Dilution
Microdilution (micro titer tray)
Macrodilution (tubes)
Mueller Hinton agar
35 degrees Celsius
16 to 20 hours
Minimum inhibitory concentration(mic) susceptible resistant
Breakpoints
Disk Diffusion
Mueller-Hinton
Agar dilution
Broth microdilution methods
Agar dilution derivations
E-test
BIOMIC
19
PPT Flashcards
270) Contain substances (e.g., oxacillin) that screen for specific organisms, Growth on the screens correlates with resistance to the antimicrobial agent.
271) Uses disks impregnated with antimicrobial agents that screen for specific organisms, Zones greater than the established value for the antimicrobial agents are considered susceptible
272) Differentiates clindamycin resistance among Staphylococcus aureus resulting from efflux (methicillin-resistant S. aureus
[MSRA] or macrolide-lincosamidestreptogramin-B [MLSB] methylase). A Dshaped zone indicates inducible clindamycin resistance.
273) Contain substances (e.g., oxacillin) that screen for specific organisms, Growth on the screens correlates with resistance to the antimicrobial agent.
274) Uses disks impregnated with antimicrobial agents that screen for specific organisms, Zones greater than the established value for the antimicrobial agents are considered susceptible
275) Differentiates clindamycin resistance among Staphylococcus aureus resulting from efflux (methicillin-resistant S. aureus
[MSRA] or macrolide-lincosamidestreptogramin-B [MLSB] methylase), A Dshaped zone indicates inducible clindamycin resistance.
276) A chromogenic cephalosporin (Cefinase disk) is used to detect
277) Is useful for detecting resistance in:
Neisseria gonorrhoeae
Haemophilus influenzae
Staphylococci
278) ________are useful for thoroughly characterizing the resistance of bacterial collections
279) Molecular methods are important for investigating
Agar screens
Disk Screens
D Test
Agar screens
Disk screens
D test
Beta-lactamase production
Beta Lactamase detection
Molecular methods
Equivocal results
20
PPT Flashcards
280) What do these have in common?
Use of probes or oligonucleotides for specific resistance genes; divergent genes could be missed.
Presence of one gene does not guarantee resistance,
Genes may be silent and incapable of expressing resistance,
Using molecular methods in the clinical setting may be impractical since the majority of testing can be accomplished using conventional methods.
281) _______determine the ability of antimicrobial agents to kill bacteria.
282) An aliquot of the MIC tube is subcultured to agar to determine the CFUs.
283) MBC is the concentration resulting in a
99.9% reduction
284) ________measure the rate of killing over time
285) Medium uses patient serum containing the antimicrobial agent,
286) Trough specimens are collected before the drug is administered,
287) Peak specimens are collected when the concentration is highest
288) _______determines the effectiveness of combinations of antimicrobial agents
Chapter 13
289) What test methodology differentiates group A streptococci from other betahemolytic streptococci?
290) What test methodology differentiates staphylococci (resistant) from micrococci
(sensitive)?
291) True or False:
In order to determine bacitracin susceptibility, a Taxo A disk is placed on an inoculated agar and zone of inhibition are observed.
292) For bacitracin susceptibility, what size of the zone of inhibition is considered susceptible (sensitive)?
293) What are the limitations of bacitracin susceptibility?
Factors that complicate molecular testing
Bactericidal test
Minimum bactericidal concentration
Time kill studies
Serum bactericidal test
Synergy testing
Bacitracin Susceptibility
Bacitracin Susceptibility
True any zone >10 mm
Performance depends on the integrity of the disk.
21
PPT Flashcards
294) What two quality control organisms would test positive for bacitracin susceptibility?
295) What two quality control organisms would test negative for bacitracin susceptibility?
296) What test methodology differentiates enterococci and group D streptococci from nongroup D viridans streptococci?
297) Bile esculin agar determines whether organisms can hydrolyze ____ to ____.
298) What color precipitate would form for a positive reaction of bile esculin agar?
299) What are the limitations of bile esculin agar?
300) What quality control organism would test positive on bile esculin agar?
301) What two quality control organism would test negative on bile esculin agar?
Streptococcus pyogenes
Micrococcus luteus dark brown to black
(susceptible)
(susceptible)
Streptococcus agalactiae
Staphylococcus aureus
Bile Esculin Agar esculin to esculetin
(resistant)
(resistant)
Some organisms may grow poorly.
Enterococcus faecalis (growth, black precipitate)
Escherichia coli (growth, no color change)
Streptococcus pyogenes (growth, no color change)
Bile Solubility Test 302) What test methodology differentiates
Streptococcus pneumoniae from alphahemolytic streptococci?
303) True or False:
For the bile solubility test, bile or bile salts rapidly lyse pneumococcal colonies on blood agar.
304) What are the limitations of the bile solubility test?
305) What quality control organism would test positive for the bile solubility test?
306) What quality control organism would test negative for the bile solubility test?
307) What test methodology differentiates group B streptococci from other streptococci species?
308) True or False:
Listeria monocytogenes produces a positive
CAMP reaction.
309) True or False:
A diffusible hemolytic protein (Christie,
Atkins, Munch-Petersen [CAMP] factor) acts synergistically with the beta-lysin of
Staphylococcus aureus causing enhanced lysis.
True
Old cultures may not have strong activity.
Streptococcus pneumoniae
Enterococcus faecalis
CAMP Test
True
True
22
PPT Flashcards
310) If an arrowhead zone of hemolysis is observed during the CAMP test, does this show a positive or negative result?
311) What are the limitations of the CAMP test?
312) What quality control organism would test positive for the CAMP test?
313) What quality control organism would test negative for the CAMP test?
314) What test methodology differentiates catalase-positive organisms and staphylococcus species from catalasenegative streptococcus species?
315) True or False:
For the catalase test, the catalase enzyme converts hydrogen peroxide to water and oxygen, producing bubbles.
316) What are the limitations of the catalase test?
317) What quality control organism would test positive for the catalase test?
318) What quality control organism would test negative for the catalase test?
319) What test methodology identifies the organism’s ability to use sodium citrate as the sole source of carbon?
320) For citrate utilization, the bacteria that is capable of growing on the medium uses citrate to convert ammonium phosphate into ammonia and ammonium hydroxide, creating an ____ pH which is indicated by a blue color change.
321) What are the limitations of citrate utilization?
322) What quality control organism would test positive for citrate utilization?
323) What quality control organism would test negative for citrate utilization?
324) What test methodology differentiates
Staphylococcus aureus (positive) from coagulase-negative staphylococci?
325) During coagulase test, the coagulase or
“clumping factor” reacts with ____ in plasma, producing a fibrin clot.
326) What are the limitations of the coagulase test? positive
Some group A streptococci are positive for
CAMP.
Streptococcus agalactiae arrowhead hemolysis)
Streptococcus pyogenes
(enhanced
(beta hemolysis without enhanced arrowhead formation)
Catalase Test
True
Some organisms (enterococci) appear weakly positive.
Staphylococcus aureus
Streptococcus pyogenes
Citrate Utilization alkaline
Some organisms will not produce a color change but will grow.
Enterobacter aerogenes (growth, blue color)
Escherichia coli (little to no growth, no color change)
Coagulase Test fibrinogen
Positive results can revert back to negative after 24 hours.
23
PPT Flashcards
327) What quality control organism would test positive for the coagulase test?
328) What quality control organism would test negative for the coagulase test?
329) What test methodology is used to visualize the presence and arrangement of flagella for the presumptive identification of motile bacterial species?
330) The flagella stain contains a mordant to better visualize ____.
331) What are the limitations of the flagella stain?
332) Match the following quality control organisms to their correct flagella stain results.
Quality control organism:
Escherichia coli
Pseudomonas aeruginosa
Klebsiella pneumonia
Flagella Stain Results: nonmotile
Polar
Peritrichous
333) What test methodology is used to identify organisms that produce tryptophanase?
334) True or False:
During indole production, tryptophanase will hydrolyze tryptophan to pyruvate, ammonia, and indole.
335)
Kovac’s reagent used for indole production will produce what color when reacted with indole?
336) The alternative spot indole test will produce a ____ color when positive.
337) What quality control organism would test positive for the Kovac’s method of indole production?
338) What quality control organism would test negative for the Kovac’s method of indole production?
339) What two test methodology differentiates members of the Enterobacteriaceae family?
340) A positive result for the Methyl Red Test which detects mixed acid fermentation is indicated by what color?
Staphylococcus aureus
Staphylococcus epidermidis
Flagella Stain flagella
Visualization requires expertise and is not an entry-level technique.
Escherichia coli
–
Peritrichous
Pseudomonas aeruginosa – Polar
Klebsiella pneumonia
– nonmotile
Indole Production
True red blue
Escherichia coli
Klebsiella pneumoniae
Methyl Red and Voges-Proskauer Tests
Red
24
PPT Flashcards
341) A positive result for the Voges-Proskauer
Test which detects the ability of an organism to convert the acid products to acetoin and
2,3-butanediol is indicated by what color?
342) For the Methyl Red and Voges-Proskauer
Test, is it possible for an organism to be positive for one test but not for both of the tests.
343) What are the limitations of the Methyl
Red and Voges-Proskauer Tests?
344) What quality control organism would test positive for Methyl Red but negative for
Voges-Proskauer Tests?
345) What quality control organism would test negative for Methyl Red but positive for
Voges-Proskauer Tests?
346) What test methodology determines whether an enteric organism is motile and must possess flagella?
347) For mobility testing, ____ agar is used to visualize a diffuse zone of growth extending from the line of inoculation.
348) What are the limitations of the motility testing?
349) What quality control organism would test positive for motility testing?
350) What quality control organism would test negative for motility testing?
351) What test methodology determines whether an organism can reduce nitrite?
352) True or False:
Microorganisms capable of reducing nitrite to nitrogen will not turn a color and will produce gas in the nitrate reduction (nitrate to nitrite) test.
353) What are the limitations of nitrate reduction?
354) What quality control organism would test positive for nitrate reduction?
355) What quality control organism would test negative for nitrate reduction?
356) What test methodology differentiates pneumococci (sensitive) from other alphastreptococci (resistant)? red yes
MR test should not be read before 48 hours.
Escherichia coli
Enterobacter aerogenes
Motility Testing semisolid
Some organisms do not display sufficient growth.
Escherichia coli
Staphylococcus aureus
Nitrate Reduction
True
Zinc dust is added if broth does not become red or no gas is observed.
Proteus mirabilis (colorless, gas)
Acinetobacter baumanii (red, no gas)
Optochin (P Disk) Susceptibility
25
PPT Flashcards
357) True or False:
In order to determine optochin susceptibility, a Taxo P disk is placed on an inoculated blood agar plate, incubated, and observed for zone of inhibition.
358) For optochin susceptibility, what size of the zone of inhibition is considered susceptible (sensitive)?
359) What are limitations of optochin susceptibility?
360) What quality control organism would test positive for optochin susceptibility?
361) What quality control organism would test negative for optochin susceptibility?
362) What test methodology determines the presence of cytochrome oxidase activity for oxidase-negative enteric bacteria from other gram-negative rods?
363) The oxidase test determines the presence of cytochrome oxidase using tetramethyl-pphenylenediamine dihydrochloride to indophenol, resulting in what color end product?
364) What are the limitations of the oxidase test?
True any zone ≥14 mm
Any zone less than 14 mm is questionable.
Streptococcus pneumoniae (susceptible)
S. pyogenes (resistant)
Oxidase Test purple
Nickel-base alloy wires that contain chromium and iron may cause a falsepositive result.
Pseudomonas aeruginosa 365) What quality control organism would test positive for oxidase test?
366) What quality control organism would test negative for oxidase test?
367) What test methodology is used for the presumptive identification of group A streptococci and enterococci?
368) Beta-naphthylamine, a byproduct of hydrolyzation by
L -pyrrolidonyl arylamidase (PYR), will turn
____ in the presence of
N,N-dimethylamino cinnamaldehyde reagent.
369) What two quality control organism would test positive for pyrrolidonyl arylamidase test?
370) What quality control organism would test negative for pyrrolidonyl arylamidase test?
Escherichia coli
Pyrrolidonyl Arylamidase Test red
Enterococcus faecalis
Streptococcus pyogenes
Streptococcus agalactiae
26
PPT Flashcards
371) What test methodology determines whether a gram-negative rod ferments glucose and lactose or sucrose to forms hydrogen sulfide?
372) Triple sugar iron (TSI) agar contains __ parts lactose, __ parts sucrose, and __ part glucose & peptone; and ferrous sulfate.
373) For the triple sugar iron agar, the butt of tube turns ____ if glucose is fermented (acid).
374) For the triple sugar iron agar, the slant of tube turns ____ if lactose or sucrose are fermented (acid).
375) For the triple sugar iron agar, the tubes turns ____ if hydrogen sulfide is produced.
376) Match the following quality control organisms to their correct TSI results.
Quality control organism:
Pseudomonas aeruginosa
Proteus mirabilis
Shigella flexneri
TSI Results:
K/A (alkaline/acid)
K/K (alkaline/alkaline)
K/A (alkaline/acid), hydrogen sulfide
377) What test methodology differentiates
Haemophilus species?
378) X, V, or XV strips or disks are placed on
____ inoculation.
379) True or False:
For X and V factor tests, organisms will grow around the disk that provides the appropriate factor for growth.
380) Match the following quality control organisms to their correct X and V factor test results.
Quality control organism:
Haemophilus influenza
Haemophilus parainfluenzae
Haemophilus ducreyi
X and V factor test results: requires X disk; grows around XV and X disks requires V disk; grows around XV and V disks requires XV disk only
Triple Sugar Iron Agar
10, 10, 1 yellow yellow black
Pseudomonas aeruginosa – K/K
(alkaline/alkaline)
Proteus mirabilis – K/A (alkaline/acid), hydrogen sulfide
Shigella flexneri – K/A
X and V Factor Tests confluent
True
Haemophilus influenza – requires XV disk only
Haemophilus parainfluenzae – requires V disk; grows around XV and V disks
Haemophilus ducreyi - requires X disk; grows around XV and X disks
27
PPT Flashcards
381) True or False:
Additional tests exist and result in growth, turbidity, or color changes.
382) True or False:
Other test examples include the following:
Use of substances as a source of carbon
Esculin hydrolysis
Fermentation tests
Detection of enzymes
Growth on specific agars
Growth around impregnated disks
Chapter 14
383) What are the general characteristics of
Staphylococcus aureus?
True
True
384)
385)
What are the types of media used for observation and identification of bacterial growth?
What is coagulase, and what are some examples of coagulase positive and negative organisms?
386) What diseases are the normal flora
Micrococci and staphylococci responsible for causing?
387) What is MRSA and what is the treatment for the infections?
388) What is a D zone test?
Gram-positive cocci
Catalase positive
Nonmotile
Aerobic or facultatively anaerobic
Medium, circular and entire, smooth, convex, usually white-to-yellow colonies
5% sheep blood agar
(Routine medium)
Mannitol salt
(High concentration of salt, sugar mannitol, and phenol red dye)
PEA
Columbia CNA agar
CHROMagar
(Used for the identification of MRSA)
Coagulase is an enzyme that clots plasma.
Staphylococcus aureus is the most common coagulase-positive staphylococci [CoPS] and S. epidermidis is the most common coagulase-negative staphylococci [CoNS].
Micrococci and staphylococci are associated with skin and urinary tract infections (UTIs) such as S. epidermidis and S. epidermidis.
Strains that carry the mecA gene are referred to as methicillin-resistant
Staphylococcus aureus (MRSA). Two types of MRSA are Hospital acquired (HA-
MRSA) and Community acquired (CA-
MRSA). Infections are usually treated with vancomycin.
A D-zone test (modified Kirby-Bauer test) determines the inducible clindamycin resistance in Staphylococcus sp.
28
PPT Flashcards
389) What methods of prevention are used for
Staphylococcus aureus ?
Chapter 15
390) What are general characteristics of
Streptococcus sp. and
Enterococcus sp.?
391) What is Alpha Hemolysys?
392) What is Beta Hemolysys?
393) What is Gamma Hemolysys
394) Most streptococci are placed in which
Lancefield group.
395) Which Lancefield group is Streptococcus pyogenes placed in?
396) Which Lancefield group is S. agalactiae placed in?
397) Which Streptococci organisms do not belong to a Lancefield group?
398) What infections are usually associated with Streptococcus pyogenes?
399) What infections are usually associated with S.agalactiae?
400) What infections are usually associated with S. pneumoniae?
401) What infections are usually associated with Enterococcus sp?
402) Which two organisms do not grow on routine media?
403) Which agar will Streptococcus sp.
and
Enterococcus sp . not grow in?
404) Which selective media will Streptococcus sp.
and Enterococcus sp . grow in?
405) Which broth can be used to detect
Streptococcus agalactiae from a genital specimen?
406) Individuals with Streptococcus pyogenes produce antibodies to the which of the following?
407) Which gram-positive cocci are catalase positive?
Chapter 16
408) Which soil species primarily causes disease in wild and domestic herbivores?
409) Which bacillus produces endospores, which are highly resistant to heat and desiccation
Health care workers and newborns are treated with antibiotics to prevent spreading infection, and patients are screened for MRSA.
Catalase negative; gram positive cocci appearing; nonmotile
Partial lysis of red blood cells
Complete lysis of red blood cells
No hemolysys
Lancefield group (A-G)
Group A
Group B
S. pneumoniae and viridans streptococci
Bacterial pharyngitis, Skin infections,
Scarlet fever, Poststreptococcal diseases
Septicemia, pneumonia, and meningitis in newborns
Bacterial pneumonia, meningitis, and otitis media
Urinary tract infections (UTIs), bacteremia, and intraabdominal infections
Abiotrophia & Granulicatella
MacConkey agar
Columbia colistin-nalidixic acid (CNA) agar and Penylethyl alcohol (PEA) agar
Todd-Hewitt broth
Streptolysin O, Deoxyribonuclease (DNase)
B, Streptokinase, Hyaluronidase
Staphylocci sp, Micrococci sp
Bacilus sp.
Bacilus anthracis
29
PPT Flashcards
410) Necrotic lesion caused by bacillus anthracis is?
411) What is the major infection caused by bacillus anthracis ?
412) What is the disease caused by inhalation of spore from exposure to animals?
413) Which species demonstrates following growth pattern on mediea?: nonhemolytic on sheep blood agar. Majority of other species are beta-hemolytic
Bacillus anthracis
414) Which characteristic can be observed for bacillus anthracis on gram stain?
415) Which agar plate induces capsule
Gram positive rods
Bicarbonate agar formation in bacillus antracis?
416) Which media can isolate bacillus cereus? Media containing different mixtures of egg
417) Production of lecithinase is used to differentiate which species?
418) What is recommended after aerosol exposure?
419) Chapter 20
420) Which group of gram-negative rods is eschar cutaneous
Woolsorter’s disease, pulmonary yoks, mannitol and polymyxin B
Differentiation among bacillus, brevivacilus and paenibacilus.
Chemoprophaylaxis with ciprofloxacin
Enterobacteriacea facultatively anaerobic, can ferment glucose and is oxidase negative?
421) What is the general appearance of
Enterobacteriacea on blood agar?
422) Can Enterobacteriacea reduce nitrates? medium to large mucoid, gray colonies
423)
424)
On which routine media can
Enterobacteriacea grow?
On which selective agar can
Enterobacteriacea grow?
Yes (except Photorhabdus and
Xenorhabdus)
5% sheep blood, chocolate and MacConkey agars
Hektoen enteric (HE), Xylose-lysinedeoxycholate (XLD), Salmonella-shigella
(SS), Cefsulodin-irgasan-novobiocin (CIN),
MacConkey-sorbitol (MAC-SOR)
Triple sugar iron (TSI) agar 425) What is a special media used to identify
Enterobacteriacea?
426) What method can help differentiate
Salmonella, Shigella and Escherichia coli ?
427) Which antigens on Salmonella are used as targets for serotyping?
428) Which antigens of Shigella are targets for serotyping?
429) Which bacteria has the somatic 157 and flagellar 7 antigens?
430) What are the two pathogenic groups of
Enterobacteriacea?
Serotyping somatic (O) antigens, capsular (K) antigen and flagellar (H) antigen somatic antigens (A, B, C and D)
E.coli
O157:H7
Opportunistic pathogens and intestinal pathogens
30
PPT Flashcards
431) What is a key difference between opportunistic and intestinal pathogens?
432) Which type of pathogens are most likely to cause disease only in immunocompromised individuals?
433) What makes intestinal pathogens more dangerous than opportunistic enteric pathogens?
434) Name the five types of E.coli
that are intestinal pathogens.
Intestinal pathogens are not usually normal flora whereas opportunistic pathogens are
Opportunistic pathogens intestinal pathogens have greater virulence factors
Enterohemorrhagic (EHEC), enterotoxigenic (ETEC), enteropathogenic
(EPEC), enteroinvasive (EIEC), enteroaggregative (EAEC) uropathogenic E.coli
(UPEC) and meningitis-sepsis pathotypes (MNEC)
Enterohemorrhagic E.coli
(EHEC)
435) Which two classes of E.coli
are extraintestinal pathogens?
436) Which E.coli infection causes hemorrhagic diarrhea?
437) Which bacteria causes neonatal meningitis and is positive for K1 antigen?
438) Which type of pathogenic E.coli
is associated with aggR gene?
439) What type of infection causes watery to bloody diarrhea?
440) Name the four intestinal pathogens in the
Enterobacteriacea group.
441) Hemolytic uremic syndrome (HUS) is a serious condition that can cause what symptoms?
442) What selective media will help differentiate E.coli
O157:H7 from other
E.coli
strains?
443) What parts of the body do Klebsiella normally inhabit?
444) What Enterobacteriacea pathogen can cause pneumonia, septicemia, UTIs and liver abscesses?
445) What test will help differentiate between
K.pneumoniae and K.oxytoca
?
446) Which Enterobacteriacea pathogen ferments lactose, is positive on Voges-
Proskauer test and citrate positive?
447) What is the most common mode of infection by Enterobacter spp.?
448) Is Enterobacter spp. indole positive or negative?
449) Which Enterobacteriacea pathogen produces deoxyribonuclease (DNase)?
Meningitis-sepsis
Enteroaggregative
Enteroinvasive
Salmonella
Yersinia
(all serotypes), spp.,
Shigella
Escherichia coli
spp.,
Hemolytic anemia, low platelet count, kidney failure and death
Klebsiella
Indole test
Klebsiella medical devices negative
Serratia
spp.
spp.
spp.
E.coli
E.coli
E.coli
(MNEC)
(EAEC)
(EIEC)
MacConkey-sorbitol agar nasopharynx and gastrointestinal tract
31
PPT Flashcards
450) Are Serratia spp. motile or sporeforming?
451) What bacteria commonly causes infections through urinary catheters and intravenous fluids?
452) What are three common species of
Citrobacter spp.?
453) How is Citrobacter commonly transmitted?
454) Is Citrobacter citrate positive?
455) What Enterobacteriacea contain phenylalanine deaminase and are non-lactose fermenters?
456) What do extended-spectrum betalactamases hydrolize?
457) Chromogenic agar is used to detect
ESBLs in what group of bacteria?
Both
Serratia
C.freundii
person to person
Yes
Proteus
spp.
, C.koseri
and
, C.braakii
Providencia
Enterobacteriacea penicillins an cephalosporins
458) What is reported if an organism is ESBL positive?
459) Which type of typhoid fever is resistant to chloramphenicol, ampicillin, and cotrimoxazole? organism is resistant
Multidrug-resistant typhoid fever
460) What causes Multidrug-resistant typhoid fever?
Overuse, misuse and the inappropriate use of antibiotic therapy
461) What is the Modified Hodge test used for? The identification of carbapenemase production
462) What are three main differences between Salmonella is motile, produces hydrogen sulfide and can decarboxylate lysine the plague
Salmonella and Shigella?
463) What deadly infectious disease is caused by Yersinia pestis ?
464) What illness is Yersinia enterocolitica mainly associated with?
465) What does the unique Gram staining of
Yersinia look like? foodborne illness related to undercooked food products bipolar staining ("safety pin")
466) Which Enterobacteriacea species exhibits a rough, cauliflower appearance on agar?
467) What does Yersinia enterocolitica look like when plated on CIN agar?
Yersinia pestis red bull's eye colonies
Chapter 22
468) How is Pseudomonas aeruginosa transmitted?
A.
Via ingestion
B.
Exposure to contaminated food, water, or medical devices.
C.
Via inhalation
D.
Only A & B
D. Only A & B.
32
PPT Flashcards
469) How is Burkholderia cepacia transmitted? Exposure to contaminated medical devices
470) How is Burkholderia pseudomallei Via inhalation or direct inoculation through transmitted? mucosa
471) How is Burkholderia mallei transmitted? Close animal contact
472) Which bacterium is found in tropical and Burkholderia pseudomallei subtropical areas?
473) Which bacterium causes glanders in horses?
474) Which bacterium survives well in domestic environments?
475) Which bacteria can colonize the respiratory tract of cystic fibrosis patients?
476) Pseudomonas aeruginosa is an opportunistic pathogen that can cause
Burkholderia mallei
Pseuomonas aeruginosa
Burkholderia cepacia
True community- or hospital- acquired infections.
True or False
477) Which endotoxin does Pseudomonas aeruginosa produce?
478) Which bacteria is associated with the following virulence factors:
479) Endotoxins, endotoxin A, proteolytic enzymes, alginate, pili, and intrinsic resistance to many antimicrobial agents.
480) Which of the following are communityacquired infections
481) Pseudomonas aeruginosa hospitalacquired infections include _______?
Endotoxin A
Pseudomonas aeruginosa
Respiratory tract
Urinary tract
Wounds
Bacteremia
Central nervous system
482) Folliculitis, eye infections, osteomyelitis, and respiratory tract infections in cystic fibrosis patients are all examples of what type of Pseudomonas aeruginosa infections?
483) Burkholderia infections may result from exposure to ______?
484) What are Burkholderia infections caused by exposure to contaminated medical devices?
485) What infections can cause sudden lung infections and bacteremia?
486) Cystic fibrosis and chronic granulomatous disease are associated with what bacteria?
487) What is the appearance of Brevundimonas diminuta?
Community-acquired infections
Contaminated medical solutions or devices
Septicemia
Urinary tract infections
Respiratory tract infections
Burkholderia
Burkholderia
Long straight rods
33
PPT Flashcards
488) What is the appearance of Burkholderia mallei?
489) What is the appearance of Pseudomonas pseudomallei?
490) What temperature does Pseudomonas aeruginosa grow at?
491) Is Pseudomonas aeruginosa arginine dihydrolase positive or negative?
492) Is Pseudomonas aeruginosa alpha-, beta-, or gamma-hemolytic?
493) Does Pseudomonas aeruginosa ferment lactose?
494) What is the appearance of Pseudomonas aeruginosa colonies?
495) Pseudomonas aeruginosa oxidizes glucose and xylose? True or False
496) What organism will not grow on
MacConkey agar?
497) What organism will turn red on Ashbrown medium?
498) What is the antimicrobial therapy for
Burkholderia cepacia?
Coccobacillus
Small with bi-polar staining
42 C positive
Beta-hemolytic
No
Flat colony with metallic sheen
True
Brevundimonas vesicularis
Burkholderia pseudomallei
499) What is the antimicrobial therapy for
Burkholderia pseudomallei?
Piperacillin
Ceftazidime
Ciprofloxacin
Chloramphenicol
Trimethoprim-sulfamethoxazole
Ceftazidime
Piperacillin-tazobactam
Ticarcillin-clavulanate
Amoxicillin-clavulanate
Imipenem
Trimethoprim-sulfamethoxazole
Pseudomonas aeruginosa 500) Which Pseudomonas species is intrinsically resistant to various antimicrobial agents?
501) Which Pseudomonas species readily acquires resistance to active agents?
Chapter 25
502) Alcaligenes, Bordetella, and Comamonas are gram positive or gram negative?
503) Alcaligenes, Bordetella , and Comamonas are
A.
oxidase positive
B.
non-glucose users (asacchrolyitic)
C.
grow on MacConkey agar
D.
all of the above
Pseudomonas aeruginosa
Gram negative
D. all of the above
34
PPT Flashcards
504) What organisms are aerobic, non sporulating, motile rods?
505) What organsims are aerobic rods or coccobacilli and motile?
506) Comamonas and Delftia are aerobic, nonsporulating, straight or slightly curved gram negative rods. True or false?
507) What genus has motile and non-motile species?
508) What organisms are plump rods found in pairs or short chains?
509) What organism involves the exposure of debilitated patients to contaminated fluids or medical solutions?
510) What organism can occur in patients with exposure to animals?
511) B. holmesii has only been found in human blood. True or false
512) Achromobacter has been associated with
A.
Bacteremia
B.
meningitis
C.
pneumonia
D.
all of the above
513) What organism can be isolated from pharyngeal swabs, wound, blood, and ear dishcharge?
514) What organism can be recovered from patients with cystic fibrosis?
515) What organism can be recovered from urine, prostate secretions, buccal cavity, pleural fluid, and eyes secretions?
516) What organism is associated with bacteremia, pancreatic abscess, and occular, bone, urinary, and ear infections?
517) Comamonas can be associated with
A.
meningitis
B.
bacteremia
C.
endocarditis
D.
all of the above
518) What organism can be found in the urinary tract?
Achromobacter
Alcaligenes
True
Oligella- O. ureolytica is motile, O. urethralis is non-motile
Roseomonas
Achromobacter denitrificans
Bordetalla bronchoseptica
True
D. all of the above
Achromobacter piechaudii
Achromobacter xylosoxidans
A. denitrificans
Alcaligenes faecalis
D. all of the above
Oligella
35
PPT Flashcards
519) Alcaligenes, Bordetella, and Comamonas gorw well on
A.
chocolate agar
B.
blood agar
C.
MacConkey agar
D.
all of the above
520) Alcaligenes faecalis can make colonies with feathered edges surrounded by green discoloration. True or false
521) What organism produces a fruity odor
(apples or strawberries)?
522) What organism can produce yellow, spreading colonies with a fruity odor?
523) Roseomonas has a pink pigment with some mucoid colonies. True or false
Chapter 26
524) Vibrio, Aeromonas, Chromobacterium, and Related Organisms
525) Which organisms are best described as facultative anaerobic curved rods gramnegative bacilli?
526) Which organisms are best described as straight rods with rounded ends to coccobacillary facultative anaerobes that occur singly or in pairs?
527) Which organisms are best described as a facultatively anaerobic motile rod or cocci?
528) What is the other general characteristics of Vibrio, Aeromonas, Chromobacterium, and Related Organisms?
529) Which organisms habitat is: Brackish or salt water (halophilic)?
530) Which organisms habitat is: Aquatic environments around the world?
531) Which organisms habitat is:
Environmental; soil and water of tropical regions?
532) What is the mode of transmission of
Vibrio spp.?
533) What is the mode of transmission of
Aeromonas spp.
534) What is the mode of transmission of
Chromobacterium violaceum
D. all of the above
True
A. faecalis
Myroides
True
Vibrionaceae
Aeromonas spp.
Chromobacterium
Oxidase positive
Ferment glucose
Grow on MacConkey agar
Vibrio spp.
Aeromonas spp.
Chromobacterium violaceum
Exposure or ingestion to water or seafood
Ingestion of contaminated food; exposure to contaminated water or soil; traumatic inoculation of fish fins or hooks
Exposure to contaminated soil or water
36
PPT Flashcards
535) Which media used to isolate Vibrio spp? Stool samples should be collected only in
Cary-Blair medium. Buffered glycerol saline is toxic for Vibrio strains.
Stool is plated to thiosulfate citrate bile salts sucrose (TCBS) agar.
Chromogenic Vibrio agar supports the growth of
536) What is the colonial appearances of
Vibrio spp?
537) What is the colonial appearances of V. parahaemolyticus and other Vibrio spp. in
Chromogenic Vibrio agar?
V. parahaemolyticus and other Vibrio spp.
Sucrose fermenters are yellow.
Nonsucrose fermenters are green.
Colonies range from white to pale blue and violet
538) What are the three major groups of V. cholera?
539) What is the physiologic activity of the cholera toxin?
540) What cause the “rice-water” stool?
541)
542)
543)
What some other virulence factors of
V.cholera are known?
What are the Spectrum of disease of
Cholera?
V. cholerae O1
V. cholerae O129
V. cholerae non-O1
Cholera toxin—Causes mucosal cell hypersecretion of water
Cholera toxin
Enterotoxins (zonula occludens toxin
[ZOT] and accessory cholera enterotoxin
[ACE]); O1 and O139 antigens
Spectrum of disease:
Cholera
Profuse, watery diarrhea leading to dehydration (“rice-water” stool)
Hypotension
544) Nonepidemic diarrhea, associated with what group of V. cholera?
545) Which Vibrio spp. are associated with ear infections and wound infections? non-O1 group
V. alginolyticus
.
V. mimicus 546) Which Vibrio spp. are associated with gastroenteritis.
547) Which Vibrio spp. are associated with wound infections and septicemia.
548) Are all Vibrio spp. associated with infection?
549) Which species causes rare but dangerous infections that can rapidly progress to septic shock?
V. vulnificus
No. Most Vibrio spp. are rarely associated with infection.
Chromobacterium violaceum
Chapter 28
550) Moraxella and Neisseria are what kind of gram-negative rods?
Coccobacilli or short to medium sized G- rods
551) These organisms do not ferment glucose. Moraxella and Neisseria
37
PPT Flashcards
552) These organisms grow well on routine media, but most do not grow on MacConkey agar
553) What species is normal flora of the mucous membranes and endogenous strains can cause infection?
554) What organism is normal flora of the upper respiratory tract and endogenous strains can cause infection?
555) What organism is oral flora of dogs and can cause infections from dog bites?
556) What organisms are susceptible to penicillins and cephalosporins?
557) Betalactamase production is common in this organisms.
558) The colonial appearance of Moraxella atlantae on BAP medium is:
559) The colonial appearance of Moraxella atlantae on Mac medium is:
560) The colonial appearance of M. lacunata on BAP medium is:
561) The colonial appearance of M. lacunata and M. lincolnii on Mac medium is:
562) The colonial appearance of M. lincolnii and M. osloensis on BAP medium is:
563) The colonial appearance of M. nonliquefaciens, M. osloensis, Neisseria elongate, N. weaverii in Mac medium is:
564) The colonial appearance of M. nonliquefaciens on BAP medium is:
Moraxella and Neisseria
Moraxella spp.
Neisseria elongate
Neisseria weaverii
Moraxella spp. Neisseria elongata and N. weaverii
Moraxella spp
Small, pitting and spreading
NLF
Small colonies that pit the agar
No growth
Smooth, translucent to semiopaque
NLF, if growth
Smooth, translucent to semiopaque; occasionally colonies spread and pit the agar
Resembles colonies of enterobacteriaceae 565) The colonial appearance of M. canis on
BAP medium:
566) The colonial appearance of M. canis on
Mac medium is:
567) What is the colonial appearance of
Neisseria elongata on BAP medium?
568) What is the colonial appearance of N. weaverii on BAP medium?
Chapter 32
569) What genus exhibits small, pleomorphic gram-negative coccobacilli or rods?
570) In Haemophilus, protoporphyrin IX, Xfactor (hemin), and X-factor (hemin) are required for what?
NLF
Gray, translucent, smooth, glistening, may have dry claylike consistency
Small, smooth, semiopaque
Haemophilus
Growth
38
PPT Flashcards
571) Is Haemophilus facultatively anaerobic or aerobic?
572) What Haemophilus species has capsulated or unencapsulated strains and causes infections that ranging from meningitis
(encapsulated strain) to otitis media and conjunctivitis (unencapsulated)?
573) What Haemophilus species causes
Purulent conjunctivitis and azilian purpuric fever (high mortality in children)?
574) What Haemophilus species is capsulated, has toxins that may be involved in attachment, and causes Chancroid (genital lesions)?
575) What are the two categories of
Haemophilus Influenzae?
576) What category of Haemophilus Influenzae produce a capsule, has six groups that include types A through F, and Type B is the most commonly encountered cause of serious infections?
577) What category of Haemophilus Influenzae do not produce a capsule and are often normal flora of the upper respiratory tract?
578) Do most strains of Haemophilus grow aerobically and anaerobically?
579) Haemophilus spp. is stimulated by 5% to
10% of what?
580) Haemophilus spp. grow well on ____ but not on _____.
581) What factor(s) does the Chocolate agar provide?
582) What factor(s) does the Sheep blood agar provide?
583) What is Haemophilus spp. exhibiting on blood agar when tiny colonies of
Haemophilus grow around Staphylococcus aureus (produces V factor)?
Chapter 34
584) General characteristics of these species include slow growing, fastidious, curved gram-negative rods and they are oxidase positive:
Anaerobic
Haemophilus Influenzae
Haemophilus influenzae biogroup aegyptius
Haemophilus ducreyi
Typeable and Nontypeable strains
Typeable Strains
Nontypeable Strains
Yes
Carbon dioxide (CO2)
Chocolate agar; Sheep blood agar
X and V factors (NAD)
Only X factor
Satelliting
Campylobacter and Arcobacter spp.
39
PPT Flashcards
585) Being microaerophilic and the exhibition of urease activity in most species are classic characteristics of what curved gram-negative rod?
586) Which species are considered mostly pathogenic, inhabits the GI tract of animals, esp. poultry, and produces three syndromes in humans (febrile systemic disease, periodontal disease, and gastroenteritis)?
587) Which species is associated with gastroenteritis, are found in the environment and in untreated water, and are prevalent in prepared meats?
588) Which of the following is known to inhabit the human gastric mucosa but with unknown cause of transmission?
589) This particular species of Helicobacter colonizes the mucous layer of the stomach, produces urease thus increasing pH, produces cagA proteins that increase the risk for peptic ulcers, and include other virulence factors such as vacA, babA, and iceA:
590) Which of these causes gastrointestinal or extraintestinal infections?
591) Extraintestinal infections mostly occer in what kind of individuals?
592) Which of these conditions is self-limiting and does not require antibiotics?
593) Postinfectious complications of
Campylobacter spp. Include arthritis and which syndrome?
594) Which two species of Helicobacter cause proctitis, enteritis, and sepsis in homosexual men?
595) Helicobacter pylori is most commonly associated with which disorders?
596) Campy-blood agar (Campy-BAP) is used in the cultivation of what specific
Campylobacter species?
597) What medium is used in the cultivation of
Campylobacter spp?
598) Campylobacter blood-free selective agar base is known as:
599) How many selective agars are recommended for Campylobacter cultivation in stool?
Helicobacter spp.
Campylobacter spp.
Arcobacter spp.
Helicobacter spp.
Helicobacter pylori
Campylobacter spp.
Immunocompromised indivduals gastroenteritis
Guilain-Barre syndrome
H. cinaedi and H. fennelliae
Gastritis, peptic ulcers, and gastric cancer
Campylobacter jejuni cefoperazone vancomycin amphotericin
[CVA]
CCDA
Two
40
PPT Flashcards
600) Incubation temperature differentiates
Campylobacter spp. and Arcobacter spp.
What is the incubation temperature for
Campylobacter spp?
601) What is the incubation temperature for
Arcobacter spp?
602) How long may it take to detect growth of
Campylobacter spp. on blood culture media?
603) Physical characteristic s of
Campylobacter colonies reflect what color and type?
604) Darting motility on wet preparation is characterstic of what what bacterial family?
605) Morphologic characteristics of on Gram stain of Campylobacter include what variation of its rod shape that helps one identify it?
606) Helicobacter biopsy specimens are stained with silver or what type of stain?
607) How does one presumptively identify a
Helicobacter specimen?
608) H. pylori stool antigen test and the onestep immunochromatographic assay are examples of what kind of laboratory tests?
609) The process of a patient ingesting radioactively labeled urea and exhaling bicarbonate as carbon dioxide is indicative of what laboratory test?
610) Which two Helicobacter species are inoculated on Campy media without cephalothin?
611) Which Helicobacter species can be inoculated to chocolate, Brucella, Skirrow’s, and Thayer-Martin agars?
612) How long may it take to detect
Helicobacter growth?
613) Identification of Helicobacter can be determined by being positive to which three enzymes?
614) True or false: No vaccine is available for
Helicobacter .
615) Since it is one of the treatments for
Helicobacter, susceptibility testing to which antibiotic is recommended?
42°C
37°C
May take up to 2 weeks to detect growth.
Gray-to-pink mucoid colonies
Campylobacter
Curved morphologic characteristics
Giemsa stain place biopsy material into urease broth
Enzyme immunoassays
Urea breath test
H. cinaedi and H. fennelliae
H. pylori
4-7 days
Oxidase positive
Catalase positive
Rapid urease positive
True
Metronidazole
41
PPT Flashcards
616) Metronidazole, bismuth salt, and amoxicillin or tetracycline are used together to treat an infection of what bacteria?
Chapter 36
617) What are the general characteristics of the Brucella?
618)
What does mean “Brucellosis is a zoonotic disease”?
619) Organisms tend to localize in which kind of tissues?
620) What are the primary routes of transmission for Brucella spp.?
621)
622)
623)
624)
What class of pathogens Brucella spp. belong?
What are the direct detection method of the brucellosis?
What cause granulomas?
What is the procedure for the rapid test for presumptive identification of Brucella?
Helicobacter
Small, gram-negative coccobacilli
Facultatively intracellular
Nonmotile
Aerobic (some prefer carbon dioxide [CO2] for growth)
May require supplementary CO2 on primary isolation
Zoonosis is a disease of lower animal transmissible to humans ( e.g. Brucellosis).
Each of four Brucella spp. that are pathogenic for humans has a limited number of preferred animal hosts
In tissue that is rich in erythritol (e.g., placental tissue), a four carbon alcohol that enhances their growth.
Routes of transmission:
Ingestion of infected unpasteurized animal milk
Inhalation of aerosolized particles
Direct contact with infected animal parts
Accidental inoculation of mucous membranes
After infecting a host brucellae are ingested and replicate in neutrophils.
Neutrophils are phagocytized by reticuloendothelial cells of the spleen, liver, and bone marrow.
Untreated infections may cause granulomas in the organism.
Class III pathogens.
Direct detection:
Gram stain reveals small coccobacilli.
Conventional and real-time polymerase chain reaction (PCR) methods are the most reliable.
Cultivation
Presumptive identification uses the particle agglutination test with anti-smooth Brucella serum.
42
PPT Flashcards
625) What incubation condition needed to achieve optimal recovery of the Brucella spp.?
626) How are the appearances of the colonies of the Brucella spp.?
627) Name four organism of the Brucella spp. that are pathogenic for humans.
628) Identify the signs and symptoms associated with brucellosis.
These organism are fastidious. Exhibits growth on blood and chocolate agars.
Brucella agar is recommended for specimens other than blood. Incubation in enriched medium.
Colonies are small, convex, smooth, translucent, nonhemolytic, and slightly yellow after 48 hours of incubation.
Rough variants may be observed with B. canis.
B. abortus,
B. melitensis, B. suis, and B. canis.
The clinical manifestations of brucellosis vary, ranging from asymptomatic infection to serious, debilitating disease. For the most part, brucellosis is a systemic infection that can involve any organ of the body.
Symptoms, which are nonspecific, include fever, chills, weight loss, sweats, headache, fatigue, and depression.
Lymphadenopathy and splenomegaly are common physical finding.
Initial therapy includes doxycycline or tetracycline in combination with streptomycin or rifampin.
E. all of the above
629) Which regimen of antibiotics is recommended for Brucella infections?
Chapter 37
630) Factors that affect B pertussis infection include
A.
age
B.
previous immunization/infection
C.
passively acquired antibody
D.
antibiotic treatment
E.
all of the above
631) What symptoms in the catarrhal phase does whooping cough produce?
632) In the Paroxysmal stage of whooping cough, what are the symptoms?
633) Lymphocytosis is seen in what stage of whooping cough?
634) Lots of other species are associate with infections in those who are ________?
635) Pertussis plate are incubated at ___ degrees with humidity and without___?
Mild cold symptoms
Severe and violet coughing
Convalescent
Immunocompromised
35 degrees carbon dioxide
43
PPT Flashcards
636) Pertussis colonies appear
A.
small a.
shiny b.
resemble mercury droplets c.
whitish-gray with age d.
all of the above
637) Gram stained Pertussis exhibit what?
638) With a 2 minute safranin counterstain,
Pertussis visibility is?
639) Bordetella species exhibit _______ characteristics with regard to mobility, oxidase, catalase etc.
640) Routine susceptibility to antimicrobials of
____is not usually performed.
641) Pertussis is susceptible to
A.
erythromycin
B.
newer macrolides
C.
Ketolides
D.
all of the above
642) Pertussis is susceptible to
A.
tetracyclines
B.
chloramphenol
C.
Trimethoprim-sulfamethoxale
D.
all of the above
643) Some isolates of B. pertussis are resistant to erythromycin. True or false
644) Are there vaccines for Pertussis ?
645) What are three common vaccinations available for Pertussis ?
E. all of the above
Faintly staining coccobacilli
Enhanced
Different
B. pertussis
D. all of the above
D. all of the above
True
Yes
DTaP
Tdap
Td
Diptheria, tetanus, pertussis
Five doses
646) What does DTaP stand for?
647) DTaP is admistered to kids before six years of age how many times?
648) Tdap is administered to who?
649) Td (Tetanus-diptheria) boosters should be given_____
Chapter 40
650) Organisms are found in the normal flora of the upper respiratory tract except?
651) Which organism is a significant pathogen of the urogenital tract?
652) How are N. gonorrhoeae and N. meningitides transmitted?
653) M. catarrhalis usually causes which types of infections? adolescents and adults
Every ten years.
N. gonorrhoeae
N. gonorrhoeae
Person to person
Respiratory tract infections
44
PPT Flashcards
654) Which organism is a major cause of sexually transmitted diseases?
655) Where are infections caused by N. gonorrhoeae localized?
656) Which organism causes fatal bacterial meningitis?
657) For specimen collection, dacron or rayon fibers are recommended for which organism?
658) Neisseria and Moraxella catarrhalis should be inoculated on this media system immediately after collection:
659) Neisseria and Moraxella catarrhalis plates are incubated at what temperature?
660) Neisseria and Moraxella catarrhalis plates are incubated at what percent carbon dioxide?
661) Molecular assays have replaced enzymelinked immunosorbent assay (ELISA) systems for the rapid identification of which organism?
662) Sequence-based typing methods combined with serologic testing are used to detect which organism?
663) Which testing method is no longer recommended in the United States for N. gonorrhoeae and N. meningitides?
664) N. meningitides, M. catarrhalis, and
Saprophytic Neisseria should be cultivated on which two agars?
665) For N. gonorrhoeae, which selective media contains colistin, nystatin, and vancomycin?
666) For N. gonorrhoeae, which selective media contains trimethoprim added to colistin, nystatin, and vancomycin?
667) For N. gonorrhoeae, which selective media contains colistin, anisomycin, and an increase in vancomycin?
668) For N. gonorrhoeae, which selective media contains lysed horse blood, plasma, yeast dialsate, and antibiotics from MTM?
669) For N. gonorrhoeae, which selective media inhibits oral flora?
670) Isolates that must be unequivocally identified are from which source?
N. gonorrhoeae
Mucosal surfaces
N. meningitides
N. gonorrhoeae
John E. Martin Biological Environmental
Chamber; [JEMBEC] system
35 degrees C
3% to 5%
N. gonorrhoeae
N. meningitidis
Antigen detection
5% sheep blood and chocolate agars
Thayer-Martin agar
Modified Thayer-Martin (MTM) agar
Martin Lewis agar
New York City medium
GC-LECT agar
Children or those who have been sexually abused
45
PPT Flashcards
671) Isolates that are completely identified are from which source?
672) Isolates that are presumptively identified are from which source?
673) A specimen that shows an oxidase positive reaction, is gram-negative diplococci, and growth on gonococcal selective agar would be a specimen from which source?
674) Which organism is from an eye or ear culture and yields an oxidase-positive reaction, is gram-negative diplococci, and hydrolyzes tributyrin?
Chapter 41
675) What will not grow in oxygen?
676) Anaerobes lack which enzymes?
677) Name one of the anaerobic transport system used.
Sterile body fluids
Genital sites
Genital sites
M. catarrhalis
Strict anaerobes
Superoxide dismutase and catalase
678) Plates are incubated under anaerobic conditions at 35 to 37 C for __ hours
679) Plates showing no growth are incubated for __ additional days
680) Anaerobes are usually present in ____ cultures
681) T or F: joint fluid specimen is suitable for anaerobic culture.
Chapter 42
682) What are examples of pathogenic anaerobes that are soil and water inhabitants?
48 hours
5 days
Mixed
T
Clostridium botulinum and Clostridium tetani
683) (T or F) Most anaerobes are normal flora. True
684) Most anaerobes gain entry to sterile sites as a result of what?
A disruption of an anatomic barrier.
True 685) (T or F) Person-to-person nosocomial spread can occur.
686) What are the characteristics of the
Clostridium species?
Gram positive, obligate anaerobes, catalase negative, endospore-forming rods
687) What type of testing will differentiate spore-forming from non–spore forming bacilli?
688) What is the purpose of ethanol shock spore isolation?
689) In ethanol shock spore isolation, what is added to a culture for 1 hour before inoculating to an anaerobic plate?
Rubber stoppered collection vial for liquid or oxygen free collection tube for swab or self contained anaerobic bag for tissue
Shock spore testing
Identifies Clostridium populations.
species from mixed
Ethanol
46
PPT Flashcards
690) In ethanol shock spore isolation, what does the ethanol denature?
691) When will Clostridial endospores germinate?
692) What produces exotoxins that cause gas gangrene and food poisoning?
693) What produces a potent neurotoxin that is responsible for botulism?
694) What produces toxins A and B that may cause pseudomembranous colitis?
695) What is associated with neutropenic enterocolitis?
696) What produces tetanospasmin that disrupts nerve impulses to the muscles?
The cell membrane but has no effect on bacterial spores
On inoculation
Clostridium perfringens
Clostridium botulinum
Clostridium difficile
Clostridium septicum
Clostridium tetani
697) For Clostridium difficile, what is used to for culture and toxin assays?
698) For Clostridium difficile, what can specimens be plated to?
699) What is botulism caused by?
700) What is Clostridium botulinum acquired from?
Fresh stool
Cycloserine cefoxitin fructose agar (CCFA) and anaerobic blood agar
Clostridium botulinum
Ingestion (foodborne), Colonization of the gastrointestinal (GI) tract (infant botulism), and infected wounds
701) What does Clostridium botulinum cause? Complete flaccid paralysis of respiratory and other muscle groups.
702) What is tetanus caused by?
703) What does Clostridium tetani cause?
Clostridium tetani
Muscle spasms (e.g., lockjaw) that lead
704) What can paralysis be caused by? to exhaustion and respiratory failure
Clostridium botulinum and Clostridium tetani
Actinomyces , Bifidobacterium ,
Eubacterium , Eggerthella
Non-spore forming bacilli
705) What are examples of anaerobic, grampositive, non-spore forming bacilli?
706) What type of bacilli is identified with polymicrobic infections?
707) What is the differentiation of grampositive, non-spore forming anaerobes based on?
708) What tests may be used for the diagnosis of Gram-positive rods?
709) What does the Rapid testing include?
Colony and Gram stain morphology
Aerotolerance testing, Rapid testing, and
Antibiotic susceptibility
15% catalase test, production of Indole, and
Nitrate reduction
710) What are the typical results of Antibiotic susceptibility screening for Gram-positive rods?
Resistant to colistin (10 μg), Susceptible to vancomycin (5 μg), and Variable sensitivity to kanamycin (1 mg)
47
PPT Flashcards
711) What are examples of anaerobic Gramnegative rods?
712) What Gram-negative rod is isolated from the mucosal surfaces of the oral cavity and GI tract, saccharolytic, bile resisitant, and nonpigmented?
713) What are common isolates of the
Bacteroides fragilis Group?
714) What Gram-negative rod produces a foul odor from most infections, reduces nitrate, requires formate and fumarate for growth, and colonies are small and may corrode agar?
715) What Gram-negative rod is typically isolated from oral cavity (biofilms), sensitive to kanamycin, fluoresce chartreuse, and bread crumb-like colonies?
716) Where are the Gram-positive anaerobic cocci typically found?
717) What are examples of Gram- positive anaerobic cocci?
718) Where are Gram-negative anaerobic cocci typically found?
Bacteroides fragilis group, Nonpigmented
Prevotella spp ., Pigmented Porphyromonas and Prevotella spp.,
Bacteroides ureolyticus, Fusobacterium,
Proteobacteria
Bacteroides fragilis Group
B. fragilis (most common), B. thetaiotaomicron,
B. ovatus
Bacteroides ureolyticus
Fusobacterium
As part of normal flora of the oral cavity and the upper respiratory and GI tracts.
Peptostreptococcus, Finegoldia, Gallicola,
Parvimonas, Staphylococcus
As part of the Normal flora of the oral cavity and the respiratory, genitourinary, and GI tracts.
Veillonella, Megasphaera, Anaeroglobus,
Negativicoccus, Acidaminococcus
Mycobacteria
719) What are examples of Gram-negative anaerobic cocci?
Chapter 43
720) Which micro organism has this characteristics: Aerobic, Intracellular pathogens, slightly curved or straight rods,
Slow growing (2 to 60 days) and Acid-fast cell wall?
721) What is Mycobacteria Acid-fast cell wall made of?
722) What kind of disease does
Mycobacterium tuberculosis cause?
723) Name 4 species in the Mycobacterium tuberculosis complex.
724) How Mycobacterium tuberculosis is transmitted?
725) What test is used to detect mycobactria tuberculosis infection?
1- N-glycolylmuramic acid
2- Very high lipid content pulmonary disease
M. tuberculosis, M. bovis, M. africanum,
M. caprae, is transmitted person to person via inhalation of droplets
PPD test
48
PPT Flashcards
726) What is the vaccine to prevent TB?
727) Which Mycobacterium associated with the ingestion of milk from infected cows?
728) ____ epidemic is considered a major risk factor for opening the door for active TB infection?
729) Runyon classification categories are? bacille Calmette Guerin (BCG)
M. bovis
AIDS
730)
731)
732)
733)
734)
735)
What is NTM Runyon group I? group I?
What organisms are classified as Runyon
What is NTM Runyon group II? group II?
What organisms are classified as Runyon
What is NTM Runyon group III?
What organisms are classified as Runyon group III?
Runyon 1-3 are slow growers
Runyon 4 are fast growers
Photochromogens slow growing, pigment when exposed to light.
M. kansasii, M. asiaticum, M. marinum,
M. intermedium and M. novocastrense
Scotochromogens slow growing, pigment in light or in the dark
M. szulgai, M. scrofulaceum, M. interjectum,
M. heckeshornense, M. tusciae, M. kubicae,
M. gordonae, M. cookie, M. hiberniae
Nonphotochromogens slow growing, Produce no pigment, regardless of whether they are grown in the dark or the light, Most are pathogenic microorganisms.
M. avium complex, M. xenopi, M. ulcerans,
M. malmoense, M. genavense, M. haemophilum,
M. heidelbergense
Rapid growers
Rapid growers
736) What is NTM Runyon group IV?
737) When micro organism Appear on solid media within 7 days, Can grow on routine media, Appear weakly gram positive on Gram stain and Most common infections are posttraumatic wound infections are characteristic of?
738) What organisms are classified as Runyon group IV?
Common species:
Mycobacterium abscessus subsp abscessus
M. fortuitum
M. chelonae
Mycobacterium avium Complex 739) Most commonly isolated nontuberculous mycobacteria (NTM) species is?
740) In which nonPhotochromogens Infections include, Respiratory disease in adults,
Lymphadenitis in children and Disseminated infection in patients with HIV?
Mycobacterium avium Complex
49
PPT Flashcards
741)
742)
743)
744)
745)
746)
747)
748) Which stain will confirm myobactria positive test?
749) What are the 3 acid fast staining procedures?
750) In acid-fast stain Extent of infection is assessed by quantifying _________on smear
751) In Conventional phenotypic tests
Preliminary identification of mycobactrial are?
752)
What is two major forms of
Mycobacterium leprae?
Mycobacterium leprae can not cultivatable in? in? identification of mycobacterium spp.?
What is pathology of Hansen disease?
Mycobacterium leprae can be cultivated
What is characteristic of Tuberculoid?
What is characteristic of Lepromatous?
What are Direct detection methods for antitubercular agents commonly tested against M. tuberculosis What are primary drugs?
753) antitubercular agents commonly tested against M. tuberculosis What are secondary drugs?
1- Chronic disease of the skin, mucous membranes, and nerve tissue
2- Bacilli multiplying in peripheral nerves to cause sensory impairment
Tuberculoid and Lepromatous vitro armadillo or mice footpads
No immune defect
Localized to skin and nerves
Few organisms present in lesions
Extensive skin lesions
Numerous acid-fast bacilli
May disseminate
Acid-fast stains, Antigen-protein detection,
Immunodiagnostic testing, Genetic sequencing and nucleic acid amplification,
DNA microarrays,
Chromatographic analysis
Acid-fast stain
Ziehl-Neelson, Kinyoun, Fluorochrome bacilli
Growth rate—Rapid grower versus slow grower,
Pigment production, Biochemical testing
Niacin (nicotinic acid), Nitrate reduction
Catalase--Most species are positive, Tween
80 hydrolysis--Scotochromogens annonphotochromogens,
Tellurite reduction--All rapid growers reduce tellurite in 3 days, Arylsulfatase,
Growth inhibition by thiophene-2carboxylic acid hydrazide (TCH)
Isoniazid (INH), Rifampin, Pyrazinamide,
Ethambutol and Streptomycin
Ofloxacin, cycloserine, capreomycin, kanamycin, ethionamide, ciprofloxacin,
Rifabutin
50
PPT Flashcards
Chapter 46
754) Genera of this type of bacteria are differentiated by:
A.
number of axial fibrils
B.
number of insertion disks
C.
biochemical tests
D.
metabolic features
755) General characteristics of spirochetes include:
756) Treponema spp are best observed using what type of microscopy?
757) Treponema spp have what type of air requirement?
758) Treponema pallidum is known to cause:
759) Characteristics of what disease (caused by
Treponema pallidum) include the appearance of chancre, fever, weight loss and widespread rash?
760) In what direction are antibodies travelling in treponemal antibody testing?
761) What is the purpose of nontreponemal antibody testing?
762) Two common flocculation tests in nontreponemal antibody testing are:
763) This type of bacteria is known to cause borreliosis or relapsing fever.
Spirochetes helical, gram-negative bacilli dark-field microscopy microaerophilic syphilis syphilis
Toward the organism
Reagin antibodies produced toward mammalian cells
VDRL and RPR
Borrelia spp.
764) This disease caused by B. burgdorferi is transmitted by the hard tick (genus Ixodes ):
765) Relapsing fever due to Borrelia spp can be transmitted from what two sources?
766) What is the first stage of Lyme disease?
Lyme disease
Lice and ticks
Erythema migrans—Ring-shaped skin lesion
767) What is the second stage of Lyme disease?
Arthritis and neurologic disorders—Weeks to months after infection
768) What is the third stage of Lyme disease? Chronic arthritis or acrodermatitis chronica atrophicans (ACA)
769) True or False: Observation of the True organism using dark- or bright-field microscopy is useful in cases of relapsing fever.
770) B. burgdorferi is best visualized using what stain?
771) What organism is cultivated using Kelly medium?
Warthin-Starry silver stain
Borrelia spp
51
PPT Flashcards
772) What is the standard method for diagnosing Lyme disease?
773) What method is used for confirming positive tests for diagnosing Lyme disease?
774) What species of Brachyspira is not isolated from animals?
775) What species of Brachyspira is found in animals?
776) What species of Brachyspira is transmitted via fecal-oral contamination?
777) What species of Brachyspira acquired from the ingestion of water contaminated by infected animal feces?
Serodiagnosis
Immunoblotting
B. aalborgi
B. pilosicoli
B. aalborgi
B. pilosicoli
778) What grows best on brain-heart infusion of tryptic soy agar?
779) Two major groups of this are Leptospira interrogans sensu stricto (human leptospirosis) and L. biflexa (environmental strain):
780) Epidemiologic factors and pathogenesis of what bacteria causes leptospirosis, a zoonosis;
L. interrogans; and can enter through breaks in the skin or conjunctivae?
781) What type of bacteria is best cultured to semisolid media enriched with Fletcher or
Stuart rabbit serum?
Chapter 47
782) What are the classification of Human
Parasite?
783) What are the types of Transmission in
Epidemiologic Factors?
Brachyspira
Leptospira
Leptospira
Leptospira spp
Protozoa
Nematoda (roundworms)
Platyhelminthes (flatworms)
Pentastomids (tongue worms)
Acanthocephala (thorny-headed worms)
Arthropoda
Venereal transmission ( Trichomonas vaginalis )
Ingestion of contaminated food or water
•
Giardia lamblia
•
Cryptosporidium spp.
Skin penetration of infective larvae
•
Strongyloides stercoralis
•
Hookworm
Bites of various arthropods
•
Plasmodium
•
Trypanosoma
•
Leishmania
52
PPT Flashcards
784) What are the characteristics of
Pathogenesis?
_ Disease ranges from mild to serious and life threatening.
_ One, some, or multiple body sites may be infected.
_ Life cycles of parasites are important in pathogenicity.
785) How specimens should be transported? Immediately to the laboratory, or preservatives should be used if a lag time
786) What is the benefit of preservatives? exists
Maintain parasite morphologic characteristics
787) Processing depends on the use of what? _ Appropriate fixatives
_Immediate fixation upon arrival
788) What situations are considered for immediate processing?
_ Adequate mixing of fixative and specimen
_Central nervous system (CNS) specimens for free-living amebae
_ Blood films for potential malaria
Yes: 789) Is two-vial system commonly used for fecal samples?
790) What are two-vial system used for fecal sample?
791) What are the procedures used to detect organism?
_ 5% or 10% formalin for immunoassays
_ PVA for stained smears
_ Formalin-ether sedimentation
_ Trichrome stain
_ Modified iron hematoxylin stain
_ Modified acid-fast stain.
_ Modified trichrome stains: Differentiate microsporidia.
•
Weber-green
•
Ryan-blue
•
Kokoskin—hot method
792) What does Formalin-ether sedimentation do?
793) What does Trichrome stain do?
Fix eggs, larvae, oocysts, and spores.
Distinguishes cysts and trophozoites.
794) What does Modified iron hematoxylin stain do?
Demonstrates cysts and trophozoites.
795) What does Modified acid-fast stain do? Highlights Coccidia
796) What does Modified trichrome stains do? Differentiate microsporidia.
•
Weber-green
•
Ryan-blue
•
Kokoskin—hot method
797) What does microscopic examination involves?
798) What is stools used for?
The use of multiple magnifications and a skilled microbiologist
For suspected parasites of the intestinal tract.
53
PPT Flashcards
799) What are the common procedures used for intestinal tract procedure?
Ova and parasites (O&P) examination
Recovery of tapeworm scolex
Examination for pinworm
Sigmoidoscopy
Duodenal drainage
Duodenal capsule technique
800) What are included in Ova and parasite exam?
Direct wet mount
Concentration
Permanent stain
Trichomonas vaginalis 801) What is typically observed in urogenital specimens?
802) How Motile organisms are observed? Under low power (100x).
803) Are Direct antigen tests useful to defect
Trichomonas vaginalis ?
804) So how many methods are there used to
Yes
806) What organism can found in sputum?
Microscopically and Direct antigen tests detect Trichomonas vaginalis?
805) How often parasites are found in sputum? Rarely
Ascaris lumbricoides larvae
Strongyloides stercoralis
807)
808)
When is Induced Sputa are collected?
What does Liquid specimens from a variety of sites include?
Hookworm
Paragonimus spp. eggs
Echinococcus granulosus hooklets
Protozoa
Microsporidia
Induced sputa are collected after appropriate cleansing.
Fine-needle aspirates
Duodenal aspirates
Bronchoalveolar lavages
Bronchial washings
Bone marrow
Spinal fluid
Biopsy 809) What is Procedures used on tissue samples called?
810) What does biopsy include?
811) What are the important notes for blood film?
Impression smears
Tease mounts
Squash preparations
_Slide is scanned for microfilariae using low power (10x).
_Feathered edge is examined for intracellular and extracellular parasites
812) What are the important notes for thick blood film?
_Microfilariae are observed under low power.
_Oil immersion is used to search for malaria and trypanosomes
54
PPT Flashcards
813) What is the common blood film stain procedure?
814) How is buffy coat film done?
Wright stain
Giemsa stain
A smear of the white blood cell (WBC) layer of peripheral blood is scanned.
815) What are other organisms that also found in buffy coat film?
Organisms such as L. donovani , trypanosomes, and Histoplasma capsulatum
(fungus) are found in WBCs
816)
817) What procedures are included in Intestinal
824)
What does direct detection test for? parasite?
What are other measures to prevent parasites?
Chapter 48
825) What are main characteristics of
Protozoa?
826) What is pseudopodia?
Intestinal and blood parasites
_ Antigen detection using direct fluorescent antibody (DFA)
_ Enzyme immunoassay (EIA)
_ Immunofluorescent antibody (IFA),
_ Cartridges
818) What will most immunoassay used in intestinal parasite confirm?
Entamoeba histolytica
Entamoeba histolytica–Entamoeba dispar group
Giardia lamblia
Cryptosporidium spp
819) What is blood parasite based on?
820) What is cultivation?
821) What is cultivation useful for?
An antigen capture system (dipstick format)
Culture of feces for larvae
_ Reveal organisms that cannot be detected after concentration.
_ Distinguish S. stercoralis, hookworm, and
Trichostrongylus .
_ Allow the development of larvae into
822) What are the few laboratories culture for protozoan parasites? filariform stages
•
Entamoeba histolytica
•
Naegleria fowleri
•
Acanthamoeba spp.
•
Trichomonas vaginalis
•
Toxoplasma gondii
•
Trypanosoma cruzi
•
Leishmaniasis
823) What does preventive measure focus on? Personal hygiene
Proper sanitation
Elimination of sexual activities that potentiate fecal-oral contact
Chemoprophylactic agents for malaria
Vector control and awareness of blood transmission
Adequate cooking of meats
- unicellular eukaryotic organisms, possess numerous specialized organelles, multiply by binary fission.
Cytoplasmic protusions
55
PPT Flashcards
827) What are main characteristics of
Entamoeba histolytica?
Agent of amebic colitis and amebic liver abcess, rapid and unidirectional movement, cytoplasm is finely granular, there are RBC in the blood cytoplasm.
828) What are four major forms of Blastocytis hominis?
- Cyst (thick- and thin-walled), central vacuole (central body), amoeboid,
829) How are some of the ways Blastocytis hominis can be detected? granular?
- routine stool examination, antigen detection using ELISAs, antibody detection using ELISA and fluorescent antibody tests.
830) What are common species of Flagellates? Giardia lamblia, Dientamoeba fragilis,
Chilomastix mesnili, Pentatrichomonas hominis
831) Which of the common species of
Flagellates are sucking disk and have axonomes?
832) Which of the common species of
Flagellates have cytostome and spiral groove?
833) Which of the common species of
Flagellates have undulating membrane?
834) How can Giardia lamblia be acquired?
-
- Chilomastix mesnili
-
Giardia lamblia
Pentatrichomonas hominis
835) What can Giardia lamblia cause?
- acquired from contaminated food or drink?
- Giardia lamblia can cause diarrhea with no blood, mucus, or exudate
- Diarrhea, abdominal pain, Nausea, Poor weight gain, Eosinophilia
- Balantidium coli
836) What are some of the symptoms that can manifest having Dientamoeba fragilis?
837) Which protozoa is the only ciliate that infects human?
838) Which animal is Balantidium coli associated with?
839) Which three Sporozoa are in the gastrointestinal tract of vertebrates throughout life?
840) Which Sporozoa are cyst-forming coccidia?
841) How can Cryptosporidium spp.
be acquired?
842) What do Cryptosporidium spp.
infect?
- pigs
-
-
Isospora, Cyclospora, Cryptosporidium sarcocystis, toxoplasma
- acquired from contaminated water or infected persons.
843) What is the lifecycle of spp?.
Cryptosporidium
- infect epithelial cells of gastrointestinal tract
- Ingestion of oocyts--> Trophozoite development --> Merogony (asexual amplification) --> Gametogony (sexual differentiation)--> Formation of new oocytes (sporogony)
56
PPT Flashcards
844) How can people having Cryptosporidium be diagnosed?
845)
846)
850)
851)
852)
853)
854)
856)
857)
How are transmitted?
How are
How can
Chapter 49
How is
Cyclospora cayetanensis
What is the pathogenesis of cayetanensis?
Cyclospora
847) How are Cyclospora cayetanensis diagnosed?
848) How can Cyclospora cayetanensis be prevented?
849) How can Isospora (Cystoisospora) belli be diagnosed?
What are Microsporidia?
Microsporidia
Microsporidia
What are the five Plasmodium
What is the vector for
What does
acquired? be diagnosed?
Plasmodium vivax species?
Plasmodium spp.
855) How Parasites feed on red blood cell
(RBC) hemoglobin as they mature
Plasmodium vivax cause?
distributed?
- Special (modified acid- fast) stains,
Antigen detection (e.g. direct fluorescent antigen), Polymerase chain reaction (PCR), histologic examination.
- fecal, oral, or fresh produce.
- exhibits an influenza like illness with nausea, vomiting, and explosive diarrhea.
-Can be associated with biliary disease.
- Special (acid-fast) stains- Oocysts appear pink to red, Ultraviolet (UV) epifluorescence, flow cytometry.
- by wearing gloves while gardening in endemic areas and washing produce thoroughly.
- Examination of fresh material, auraminerhodamine stain may be helpful, histologic examination.
- they are obligate intracellular, spore forming parasites displaying characteristics of prokaryotes.
- from inhalation or ingestion of spores.
- common stains; chromotrope-based stains and chemifluorescent agents (e.g., calcofluor white)
-Histologic exmaination; spores may be observed by using periodic acid- Schiff
(PAS), silver, or acid-fast stains, Eelctron microscopic (EM) techniques are useful in the differentiation of genera.
P. vivax (80% of infections)
P. falciparum
P. malariae
P. ovale
P. knowlesi
The female anopheline mosquito
_ Merozoite—Is the young trophozoite.
_ Schizont—Is a trophozoite with dividing nuclei.
_ Mature schizont—Contains merozoites that invade RBCs.
_Gametocytes—Includes mature male or female merozoites
Benign tertian malaria
Widely distributed in the tropics, subtropics, and temperate zones.
57
PPT Flashcards
858) What are the characteristics of
Plasmodium vivax?
_ Infection of young cells
_ Enlargement of RBCs (one to two times the normal size)
_ Schüffner dots
_ Delicate ring
_ Very amoeboid trophozoites
_ Schizont containing 12 to 24 merozoites
Yes 859) Does relapses occur?
860) How long does paroxysm occur?
861) What are resting stages called?
862) Where is Plasmodium ovale confined to
Geographically
863) What are the characteristics of
Plasmodium ovale?
Paroxysms may cycle every 48 hours
Hypnozoites
Central West Africa and some South
Pacific islands.
_ Infection of young cells
_ Enlargement of RBCs with fimbriated edges (oval)
_ Early appearance of Schüffner dots
_ Smaller ring than P. vivax
_ Schizont containing eight merozoites
864) Does relapse occur? Relapses are possible but with spontaneous recovery
865) How long does paroxysm occur?
868) What might associate it?
Plasmodium malariae
Paroxysms cycle every 48 hours
866) What Plasmodium malariae does cause? Quartan malaria
867) How is Plasmodium malariae distributed? Sporadically distributed
May be associated with nephrotic syndrome
869) What are the characteristics of
Plasmodium malariae?
_ Infection of older cells
_ Normal-size RBCs
_ No stippling
870) Does relapse occur?
_ Thick ring, large nucleus
_ Trophozoites that form “bands” across the cell
_ Schizont containing 6 to 12 merozoites
No, relapses do not occur, but recrudescence is recognized
Paroxysms cycle every 72 hours 871) How long does paroxysm occur?
872) What does Plasmodium falciparum cause?
873) Where does Plasmodium falciparum confine?
874) What are the characteristics of
Plasmodium falciparum?
875) Does relapse occur?
876) How long does paroxysm occur?
Causes malignant tertian malaria
Confined to tropical areas
_Invasion of all stages of RBCs (heavy parasitemia)
_Comma-like red dots (Maurer dots)
_Multiple ring forms, some appliqué forms
_Crescent-shaped gametocytes
No relapse occurs.
Fever cycles every 36 to 48 hours
58
PPT Flashcards
877) What is the complication of falciparum?
Plasmodium Vessels of organs become plugged, causing fatal complications (e.g., black water fever).
Thick and thin blood films (gold standard) 878) How is Plasmodium spp. diagnosed
879) How are thick and thin blood films used to diagnose Plasmodium?
_ Between 200 and 300 oil immersion fields are examined.
_ Giemsa or Wright stain is acceptable.
_ Ethylenediaminetetraacetic acid (EDTA) anticoagulant tubes are preferred
Dipstick, cartridge 880) What are the Rapid malaria tests now available?
881)
882)
883) used?
How is Polymerase chain reaction (PCR)
Can automated instruments detect intracellular parasites?
What therapies are used to treat
Plasmodium?
Polymerase chain reaction (PCR) with specific deoxyribonucleic acid (DNA) probes is used
No.
_ Schizonticides, gametocytocides, and sporonticides are directed against relapses.
_ Chloroquine-resistant P. falciparum is present in most endemic areas
By ticks
Has a lifecycle similar to Plasmodium spp
884) How is Babesia spp. transmitted?
885) What is the life cycle of Babesia?
886) How does the trophozoites look like? Trophozoites are smaller than P. falciparum .
887) What is its ring form characteristic?
888)
889)
890)
891)
What diseases associate with
Trypanosomiasis?
What is other unique in
What is
What are the disease spectrum in
Leishmania
Trypanosoma spp.?
Babesia?
spp.?
Ring forms are pleomorphic
Maltese cross tetrads may be present
Hemoflagellate protozoa
African sleeping sickness:
+East African
+West African
Chagas’ disease
_Cutaneous lesions (flattened plaque or ulcer)
_Mucocutaneous infections
_Visceral involvement
892) What are the two phases of Leishmania?
_ Amastigote—Intracellular parasite in humans
_ Promastigote—Form found in vector
893) What is Exudate from the lesion used for? Exudate from the lesion is smeared and stained
894) What is the test also available for the detection of antiLeishmania antibodies
A rapid dipstick
Chapter 50
895) Infections caused by which Protozoa are not very well known?
Free-Living Amebae
59
PPT Flashcards
896) Most laboratories do not offer methods to diagnose what type of Protozoa?
897) Some free-living amebae encountered include what genera?
898) Free-Living Amebae tend to cause infections of which body system?
899) What is one infection of the central nervous system (CNS) caused by free-living amebae?
900) What is another infection of the central nervous system (CNS) that is caused my freeliving Amebae?
901) Which Amebae genera enter the nasal cavity and migrate to the brain?
902) What are the two Trophozoite forms?
903) Naegleria fowleri cause what kind of growth on the brain that is round with a thick double wall?
904) Which amebae genera Rapidly causes fatal PAM?
905) No flagellate stage is known for what type of protozoa?
906) What can be observed in acanthamoeba samples?
907) What infections are associated with
Acanthamoeba?
908) Which infection is associated with underlying disease (no freshwater contact)?
909) Which infection might it take several weeks or months to establish disease?
910) Which infection is associated with direct exposure to contaminated material or solutions?
911) Wearing contacts is the leading risk factor of which infection?
912) Culture with nonnutrient plates overlaid with Escherichia coli can be used to diagnose which protozoa?
913) Diagnosis for infections caused by acanthamoeba can be determined using what body fluid?
914) Diagnosis of infections associated with acanthamoeba can be determined using what kind of slide preparation?
Free-Living Amebae
Naegleria, Acanthamoeba, Balamuthia,
Sappinia, Paravahlkampfia central nervous system (CNS)
Primary amebic meningoencephalitis
(PAM)
Granulomatous amebic encephalitis (GAE)
Naegleria fowleri
Amoeboid and Flagellate
Cysts
Naegleria fowleri
Acanthamoeba spp
Cysts and trophozoites
Granulomatous amebic encephalitis and
Amebic keratitis
Granulomatous amebic encephalitis
Granulomatous amebic encephalitis
Amebic keratitis
Amebic keratitis
Acanthamoeba spp
Cerebrospinal fluid (CSF) examination
Cytospin slides preparations using bronchoalveolar lavage
60
PPT Flashcards
915) Diagnosis of infections associated with acanthamoeba can be determined using what kind of biopsy?
916) Which protozoa genera is a rare cause of human amebic encephalitis?
917) Death may occur 1 week to several months after symptoms when infected with what protozoa?
918) Balamuthia mandrillaris lifecycle is similar to what other protozoa genera?
919) How is Balamuthia differentiated from
Acanthamoeba?
920) Which protozoa can be cultured using monkey kidney cells and mucosal replicating cells (MRC), human epidermoid carcinoma
(HEp-2), and macrophages?
921) What protozoa is nonpathogenic?
922) What protozoa is the third most commonly identified flagellate?
923) What is not known in Pentatrichomonas hominis?
924) What is the appearance of
Pentatrichomonas hominis?
925) Pentatrichomonas hominis Is similar to what other protozoa except its undulating membrane extends the entire length of the body?
926) Toxoplasmosis in patients who are immunocompetent generally exhibit what?
927) Some immunocompetent patients with toxoplasmosis will have what?
928) What body system is primarily involved in immunocompromised patients with toxoplasmosis?
929) What can develop in immunocompromised patients with toxoplasmosis?
930) What illness is prevalent in immunocompromised patients with toxoplasmosis?
931) What toxoplasmosis disease is severe if the mother acquires the organism during the first or second trimester?
932) What are the symptoms of congenital toxoplasmosis?
Tissue biopsy
Balamuthia mandrillaris
Balamuthia mandrillaris
Acanthamoeba spp on the basis of nuclear morphologic characteristics (multiple nucleoli compared with only one)
Balamuthia mandrillaris
Pentatrichomonas hominis
Pentatrichomonas hominis
No cyst stage is known
Trophozoite has five anterior flagella and a parabasal body
Trichomonas vaginalis
No clinical symptoms are observed in most patients
Some will have an acute infection (e.g., lymphadenopathy)
CNS
Myocarditis
Pneumonitis
Congenital Toxoplasmosis retinochoroiditis, cerebral calcification, and hydrocephaly
61
PPT Flashcards
933) Congenital or acquired chorioretinitis infection develops in which kind of toxoplasmosis?
934) What is the most common method for the diagnosis of Toxoplasma gondii?
935) What is another method for the diagnosis of Toxoplasma gondii?
936) Examination of biopsy specimens, buffy coats, or CSF are useful for the diagnosis of what?
937) Diagnosis of Toxoplasma gondii can also be accomplished by what?
Chapter 51
938) Name the round worm species which are nonsegmented.
939) ---------- are elongated and cylindrical.
940) Following characteristics belong to what multicultural species?
Nonsegmented.
Elongated and cylindrical.
Adult worms have separate sexes.
Eggs are usually found in stool samples.
Infective stages vary with the species.
941) Name the most common and largest roundworm.
942) How Ascaris Lumbricoides is transmitted?
943) Ascaris Lumbricoides Eggs are ingested and hatched in the -----------
944) Where do adult worms of Ascaris
Lumbricoides live?
945) ----------may migrate to the lungs.
946) What are two different types of ovum in
Ascaris Lumbricoides?
947) What infertile egg looks like in Ascaris
Lumbricoides?
948) What physical characteristics male worm has in Ascaris Lumbricoides?
949) What type of worm is Enterobius vermicularis?
950) Name a pinworm which is more prevalent in children up to 14 years of age.
951) Where does Enterobius vermicularis deposit its eggs?
Ocular
Serologic method
Polymerase chain reaction (PCR)
Toxoplasma gondii
Isolation in tissue culture or laboratory animals
Nematodes
Nematodes
Nematodes
Ascaris lumbricoides
By the fecal-oral route.
Duodenum
In the small intestine.
Roundworms mammillated or nonmammillated.
Infertile eggs are oval or irregular shaped with a thin shell.
Male worms have a curved posterior end with three lips.
Is a pinworm.
Enterobius vermicularis
Female pinworm migrates out of the anus at night and lays eggs.
62
PPT Flashcards
952) How transmission occurs in Enterobius
Vermicularis?
953) Name the pinworm whose Symptoms include perianal itching.
954) What ovum looks like in Enterobius vermicularis?
955) How are Enterobius vermicularis identified?
956) What do the adults look like?
957) In Enterobius vermicularis -------------will be completely filled with eggs.
958) What type of worm is Strongyloides stercoralis?
959) What is the life cycle of Strongyloides stercoralis?
960) Where does Strongyloides stercoralis mature?
961) The larvae of what type of worm has the following characteristics?
Short buccal capsule
Large bulb on esophagus
Prominent genital primordium
962) Filariforme larvae of What type of worm has notched tail and
1:1 esophageal-intestinal ratio
Transmission occurs by the ingestion or inhalation of eggs
Enterobius vermicularis
Is a flat-sided ovum
Eggs are collected from the perianal region using tape.
Female worm has a pin-shaped tail.
Gravid females
Is a threadworm.
Filariform larvae penetrate the skin and migrate to the heart and lungs.
In the gastrointestinal (GI) tract.
Strongyloides stercoralis
Strongyloides stercoralis
963) What type of egg has Strongyloides stercoralis?
964) How Trichostrongylus spp is acquired?
965) Name a worm which is identified by oval eggs or hatched larvae in stool.
Segmented egg
Via ingestion.
Trichostrongylus spp
966) Where do worms in Trichostrongylus spp live?
Worms live in the mucosa of the small intestine.
967) What type of worm is Trichuris trichiura? Is a whipworm
968) Does the tissue migration occur in No
Trichuris trichiura?
969) The following is the life cycle of what type of worm?
Is acquired via ingestion:
Eggs are ingested.
Larvae mature in the intestine.
Eggs are passed in feces.
970) Trichuris trichiura Worms burrow into the
---------mucosa and feed on-------------.
971) This type of worm is prevalent in the
Philippines.
Trichuris trichiura
Intestinal- tissue secretions
Capillaria philippinensis
63
PPT Flashcards
972) How Capillaria philippinensis is transmitted?
973) In Capillaria philippinensis, Larvae burrow into the ---------, causing weight loss
974) Name the worm infection disease which its long-term infections may result in death
975) Following are diagnosis of what type of worm?
Eggs, worms, or larvae are identified in stool.
Eggs resemble T. trichiura with less prominent polar plugs.
Female worms produce thick- and thinshelled eggs.
976) The following is the life cycle of what type of worm?
Filariform larvae penetrate the skin.
Larvae migrate to the lungs where they are swallowed.
Worm attaches to the GI mucosa and ingest blood.
Eggs are passed in feces and mature into rhabditiform larvae.
977) Name the worm which is related to the following species infect human:
Ancylostoma duodenale
Necator americanus
978) Following are diagnosis of what type of worm?
Eggs or rhabditiform larvae are identified in stool.
Rhabditiform larvae have a long buccal capsule with small genital primordium.
Filariform larvae have pointed tails.
Chapter 52
979) What are the stages of tissue nematodes?
Transmitted by the ingestion of uncooked fish.
GI mucosa
Capillaria philippinensis
Capillaria philippinensis
Hookworms
Hookworms
Hookworms
980)
981)
How are nematodes transmitted?
How is Trichinella spiralis transmitted?
- Adult male
- Adult female
- Four larval stages
- Biting and blood-feeding arthropods
- Ingestion of small freshwater crustaceans
- Ingestion of contaminated meat
- Encysted larvae are ingested from undercooked meat.
- Larvae are deposited in striated muscle.
64
PPT Flashcards
982) The cycle of Trichinella spiralis
983) What are the characteristics of
Trichinosis?
984) What are two important species of
Toxocara spp.?
985) What are the characteristics of
Toxocariasis?
986) How is Toxocara spp. diagnosed?
987) What is Ancylostoma spp.?
988) Ancylostoma spp. is predominant in?
989) How is Ancylostoma spp. transmitted?
990) How is Ancylostoma spp. diagnosed?
991) What is Dracunculus medinensis ?
992) How is Dracunculus medinensis acquired?
- Ingestion of undercooked pork containing encysted larvae.
- Larvae liberated when cyst digested.
- Parasites mature and mate in upper intestine.
- Female worms penetrate mucosa and liberate larvae.
- Larvae carried via bloodstream to muscle.
- Encysted larvae cause disease of muscle.
- Adult stages reside in the intestine.
- Larvae will not encyst in the brain or heart tissue.
- Diagnosis is made from a muscle biopsy.
- Toxocara canis (intestinal ascarid of dogs)
- Toxocara cati (intestinal ascarid of cats)
- Is a zoonotic disease with worldwide distribution.
- Humans accidentally ingest the eggs.
- Larvae are released in the small intestine and migrate to other tissues.
- Adult worms are unable to mature in the human host.
- Diagnosis requires a biopsy of tissue.
- Serologic classification may be useful in ocular larval migrans (OLM).
Are the common hookworms of dogs and cats.
- Ancylostoma braziliense
- Ancylostoma caninum
- Are found in the southeastern United
States.
- Infective larvae penetrate the skin of the human.
- Larvae migrate through subcutaneous tissue forming tracks.
- Diagnosis is made by the evidence of visible tracks.
- Is a guinea worm.
- Is acquired from the ingestion of infected copepods in freshwater ponds.
65
PPT Flashcards
993) medinensis
994) What is Parastrongylus cantonensis ?
995) Parastrongylus cantonensis is an endemic threat in what country?
996) What is the cycle of Parastrongylus cantonensis ?
997)
998)
999)
How is diagnosed?
What is found in? endemic?
1001)
1006)
What is the cycle of
How is
?
Where is
What is diagnosed?
Gnathostoma spinigerum diagnosed?
Dracunculus
Parastrongylus costaricensis
Parastrongylus costaricensis associated with?
1002) How is Parastrongylus costaricensis
1003) What is Gnathostoma spinigerum ?
1004) Who are the definitive hosts of
Gnathostoma spinigerum ?
1005) What is the cycle of Gnathostoma spinigerum ?
1000) What does Parastrongylus costaricensis cause?
Parastrongylus cantonensis
Parastrongylus costaricensis
- Larvae are released from copepods and migrate through the thoracic musculature.
- Gravid female worm migrates to the lower extremities and produces blisters containing larvae.
- Worms are attached to a stick and slowly retract from the host by turning the stick.
- Is a rat lungworm.
- Is an endemic threat in Southeast Asia.
- Rodents shed larvae that infect mollusks
(intermediate host), which are consumed by paratenic hosts (e.g., shrimp).
- Humans ingest the intermediate or paratenic host.
- Larvae migrate to the central nervous system
(CNS) or the eye.
- Diagnosis is based on the histologic examination of the adult female.
- Is found in cotton or in the black rat.
- Is endemic in Central and South America.
Causes abdominal angiostrongyliasis:
- Inflammatory lesions in bowel walls
- Symptoms similar to appendicitis
- Is associated with the ingestion of salad contaminated with infected slugs or snails.
- Diagnosis is based on the presence of larvae or eggs in tissue.
- Is a gastric spirurid nematode.
- Dogs and cats are the definitive hosts.
- Larvae hatch in water and infect copepods.
- Humans accidentally ingest larvae from contaminated fish.
- Worms cannot mature in humans and migrate in tissue.
Diagnosis:
- Larvae are found in tissue.
- Head contains four rows of cephalic hooklets.
- Body is covered with transverse rows of spines.
66
PPT Flashcards
Chapter 53
1007) In what way are filarial nematodes transmitted by?
1008) Where do larval stages of filarial nematodes reside?
1009)
What stage of filarial nematodes’s development is pathogenic for human?
1010) What worms of nematodes produce microfilariae?
1011) In what way are Wuchereria bancrofti transmitted by?
1012) What are humans for Wuchereria bancrofti?
1013) What forms of periodicities that demonstrate W. bancrofti are known?
1014) What diseases can be caused by W. bancrofti?
1015) What methods of diagnosis W. bancrofti are used?
1016) What lymphatic filarial parasites are known?
1017) In what way are Brugia Spp worms transmitted by?
1018) What forms of periodicities that demonstrate Brugia Spp. are known?
1019) Do the Brugia Spp involve genital lymphatic vessels?
1020) Which form of Brugia has four to five subterminal and two terminal nuclei in the tail?
1021) Which form of Brugia has five to eight subterminal nuclei and one terminal nucleus in the tail?
1022) What form of microfilaria is referred as eye worm?
1023) In what way is Loa Loa transmitted by?
1024) In what testing samples can Loa Loa be identified?
1025) Does the sheath of Loa Loa stain with
Giemsa?
1026) How does nuclei of Loa Loa extend to the tail?
1027) Where in the body does Onchocerca volvulus reside?
1028) In what way is Onchocerca volvulus transmitted by?
They are transmitted by blood-sucking arthtropods.
In insect vectors
Adult worm
Female worms
By a mosquito
The definitive host
Nocturnal form and Day form
Bancroftian filariasis, Elephantiasis,
Tropical pulmonary eosinophilia
Identification of parasites in blood, fluids, or tissue and Molecular diagnostics
Brugia Malayi and Brugia Timori
By mosquitos Anopheles and Mansonia
Nocturnal and Nonperiodic
No, they do not
Brugia Malayi
Brugia Timori
Loa Loa
By the tabanid or deerfly
Worm is identified in the eye, tissue, or peripheral blood.
No
In an irregular fashion
In tissue nodules by the female black fly
67
PPT Flashcards
1029) What diseases can be caused by
Onchocerca volvulus?
1030) How the microfilariae of Onchocerca volvulus does look like?
1031) In what way is Mansonella Spp transmitted by?
1032) What form of Mansonella is found in the skin and causes a pruritic rash?
1033) What form of Mansonella does reside in pericardial, pleural, and peritoneal cavities?
1034) What form of Mansonella is found in the blood?
1035) Does Mansonella Spp have sheath?
1036) What form of Mansonella have nuclei that extend to the end of the tail?
1037)
What form of Monsanella’s nuclei does not extend to the tip?
1038) What form of Monsanella’s tail is referred to as a “shepherd’s crook?
Chapter 54
1039) What are the characteristics of Intestinal
Cestodes?
1040) What is Diphyllobothrium latum, what hosts does it infect, and what are the physical characteristics including transmission?
River blindness, skin infections, lymphadenopathy
Microfilariae lack a sheath and have nonnucleated tapered tails. by biting midges (Culicoides)
M. streptocerca
M. perstans
M. ozzardi
No
M. streptocerca and M. perstans
M. ozzardi
M. streptocerca
They are also known as tapeworms.
Mature cestodes are hermaphroditic.
Scolex: Attachment structure
Proglottids: Egg-producing units
Rostellum: Crown or scolex (smooth or hooked)
Integument: Outer covering of skin used for food absorption
Oncosphere (hexacanth) embryo: Embryos within the egg
Strobila: Adult worm segments
Freshwater broad fish tapeworm.
Largest human tapeworm.
Fish: reservoir host.
Humans: definitive host.
Mild gastrointestinal symptoms may occur.
May cause megaloblastic anemia.
Eggs and proglottids are transmitted in feces.
Ovoid, operculated, yellow-brown eggs.
Proglottids are wider than they are long; rosette-shaped central uterus.
68
PPT Flashcards
1041)
1042)
1043) can it be found, and how common is it?
1044)
Dipylidium caninum
Hymenolepis nana
What is Hymenolepis diminuta, where
What are some characteristics of Taenia solium, the hosts it infects, symptoms, and appearance?
1045) What is Taenia saginata, its diagnosis, and location?
Cat or dog tapeworm.
Double-pored with many proglottids.
Resembles a “cucumber seed” (wet) and a grain of rice (dry).
Humans acquire the tapeworm through the accidental ingestion of fleas.
Flea: Intermediate host
Humans, dogs, and cats: Reservoir host
Isolated.proglottids in stool (seedlike)
Groups of egg packets are recognized.
Scolex has four suckers and a rostellum with four to seven rows of hooklets.
Is a dwarf tapeworm.
Person-to-person transmission is possible.
Symptoms similar to pinworm
Diarrhea
Abdominal discomfort
Itchy bottom
Eggs in stool (with polar filaments)
Rat tapeworm.
Rare in humans
Infection is acquired from contaminated grains.
Lifecycle is similar to H. nana.
Eggs are in stool.
Large, ovoid, yellowish, and moderately thick eggs
Eggs contain six hooked oncospheres (no polar filaments).
Pork tapeworm.
Pigs: Intermediate host
Humans: Definitive host
Intestinal infection: Abdominal pain and diarrhea
Extraintestinal (cysticercosis) Larvae in tissue
Tapeworm segments in stool (7 to 13 uterine branches)
Round and oval eggs with thickly striated shell and six oncospheres
Beef tapeworm.
Similar lifecycle to T. solium.
Cattle: the intermediate host.
Proglottids in stool (15-18 lateral branches)
Eggs in stool
69
PPT Flashcards
Chapter 55
1046) Larvae do not reach adult stage in humans and Eggs are accidentally acquired by
________ from an intermediate host
1047) Cysticercosis, Larval infection may invade the ________, eye, or other tissues
1048) What Is the smallest of all tapeworms
1049)
What is echinococcus granulosus’s definitive host?
1050) What causes alveolar hydatid disease?
1051) coenurosis?
What causes
1052) The following characteristic describes what organism?: Larvae (spargana)—Are white, wrinkled, and ribbon-shaped.
Sparganum has bothria (grooves) instead of suckers.
Does not contain a scolex
Chapter 56
1053)
What are some characteristics of intestinal trematodes?
1054) Where are fasciolopsis buski trematodes found?
1055) How is infection acquired?
1056)
1057)
1058)
What is the definitive host?
What's the reservoir host?
Describe the life cycle of the intestinal trematodes?
1059)
1060) How does F. buski trematodes cause disease?
1061)
How is water contaminated?
What are the symptoms of F. buski disease?
1062) What are other intestinal trematodes?
1063)
What are the characteristics of H. heterophyes & M. yokogawai? ingestions
CNS
Echinococcus granulosus canine
Echinococcus multilocularis
Taenia multiceps
Spirometra mansonosides
Are flukes, dorsoventrically flattened, need at least one intermediate host (freshwater snail), most trematodes are hermaphroditic
Southeast Asian countries
By the ingestion of raw water chestnuts or caltrop.
Pig
Fish eating animals
Adult worms reside in the small intestine, eggs are shed in feces & must reach water, larvae are freed & penetrate snail, they emerge from snail(water), encyst on vegetation or fish, ingested by humans
When feces is used for fertilization
Adult worms attach to the intestine, edema and malabsorption of vitamin B12 may result
Abdominal pain, diarrhea, gastrointestinal
(GI) obstruction
H. heterophyes, M. yokogawai
M. yokogawai is a little larger than H. heterophyes. H. heterophyes has an additional sucker, eggs are small, yellow brown, embryonated and operculated.
70
PPT Flashcards
1064) disease of M. yokogawai?
1065)
1066) heterophyes?
1067) What's the diagnostic characteristics of M.
Yokogawai?
1068)
What are the epidemiologic factors &
What's the diagnosis of F. Buski?
What's the diagnostic characteristics of H.
What's the treatment for intestinal trematode infections?
The most common fluke in the Far East, acquired from ingesting pickled or uncooked fish, heavy infections result in abdominal pain, ulceration of the GI wall.
Freshwater vegetation, operculated, yellow brown, unembryonated egg
Pickled or uncooked fish, operculated with slight opercular shoulders, yellow brown, embryonated egg
Pickled or uncooked fish, operculated with slight opercular shoulders, yellow brown, embryonated egg
Drugs: Praziquantel (Biltricide) orally in 3 doses for 1 day, mild side effects, niclosamide (Niclocide) administered for 1 to 2 days.
Adult trematodes live in the biliary ducts. Chapter 57
1069) Where does Liver Flukes live?
1070) What is the intermediate host of Liver
Flukes?
1071) What are common liver flukes?
Freshwater Snail.
1072) What are the Epidemiologic Factors of liver flukes?
Clonorchis sinensis (Chinese liver fluke)
Opisthorchis viverrini (Southeast Asian liver fluke)
Fasciola (sheep liver fluke)
Reservoir hosts:
Infected feces contaminates water.
Eggs enter the snail and develop into cercariae.
Dogs, Pigs, Rabbits. 1073) What are the reservoir hosts of liver flukes?
1074) Some of liver flukes diseases are:
1075) Colonrchis Sinensis and Opisthorchis symptoms differs by their severity: what are the symptoms?
1076) Symptoms of Fasciola spp. are:
Clonorchis sinensis and Opisthorchis viverrini.
Fasciola spp.
Light infections are asymptomatic.
Heavy infections cause fever, abdominal pain, and jaundice.
Severe infections may cause biliary obstruction.
Light infections may cause fever, abdominal pain, diarrhea, jaundice, and liver tenderness.
Larvae may migrate to intestinal walls, lungs, heart, or brain.
71
PPT Flashcards
1077) What is morphology of Clonorchis
Sinensis?
1078) What are the common species of Lung
Flukes?
1079) Worms live in the lungs and produce eggs in lungs, where does we find them?
1080) What are the hosts of lung flukes?
Adult worms
Narrow and transparent reddish-yellow color
Eggs
Shouldered opercula
Small knob at opposite end of operculum
Yellow-brown
Embryonated
Paragonimus westermani (most common)
Paragonimus mexicanus
We found them in sputum or feces.
1081)
1082)
1084)
The disease of Paragonimus spp. are:
What are the diagnosis of Paragonimus spp.?
Chapter 58
1083) What are the types of blood trematodes
What are some general characteristics of blood trematodes?
Intermediate host—Freshwater snail
Second intermediate host—Crab or crayfish
Reservoir hosts
P. westermani—Dogs and cats
P. mexicanus—Pigs
Light infections are asymptomatic.
Metacercariae migration may cause tissue damage.
Worms encapsulate in a granuloma and cause chronic cough.
Eggs are isolated in sputum.
Eosinophil count is elevated.
Lesions in lungs are visualized on x-ray images.
Primarily in humans
Schistosoma haematobium
S. japonicum (Oriental blood fluke)
S. mekongi
S. mansoni
Primarily in animals
S. intercalatum
Adult schistosomes are not flattened.
Oral sucker surrounds the mouth.
Ventral sucker is below the oral sucker.
Adults
Male—1.5 cm in length and wider than the female
Female—2 cm in length and very thin
Adult worms live in veins that supply the intestines or bladder.
Eggs are passed in feces or urine via the spine.
72
PPT Flashcards
1085)
1086)
What are some epidemiologic factors?
What are some symptoms and results of parasitic disease?
Schistosoma haematobium
Africa and Arabian peninsula
S. mansoni
Africa, Arabian peninsula, and Brazil
Reservoir hosts—Rodents and marsupials
S. japonicum
China, Indonesia, and the Philippines
Reservoir hosts—Domestic animals
S. mekongi
Lower Mekong River basin (Laos)
Reservoir hosts—Dogs and pigs
S. intercalatum
Central and western Africa
Reservoir hosts—Rodents, marsupials, and nonhuman primates
Cercariae cause localized swelling and itching.
Larval migration may cause fever and malaise.
Severe tissue damage may occur when eggs penetrate tissue to reach the intestine or bladder.
Blood flukes that commonly infect other mammals may cause “swimmer’s itch” in humans.
1087) How are infectious parasites diagnosed? Eggs are detected in feces or biopsy.
Rectal biopsy (all schistosomes)
Urine or bladder biopsy (S. haematobium)
Wet mounts with or without iodine can be used.
Optimal time for recovery of S. haematobium in urine is between noon and
2 pm.
Some antibody-based assays are available.
Mycology Chapter 59
1088) What is the study of fungi?
1089) What do you call fungi that live on dead organic matter?
1090) What are fungi that are moist called?
1091) What are fungi that are filamentous called?
1092) What do you call an organism that displays both yeast and mold?
Saprophytic
Yeast
Mold
Dimorphic
73
PPT Flashcards
1093) What do you call an organism that displays both yeast and mold that are dependant on temperature?
1094) What do you call fungi that have more than one form or stage?
1095) What are the four types of phyla?
Thermally dimorphic
Polymorphic
Zygomycota, Ascomycota, Basidiomycota,
Deuteromycota
1096) How do zygomycota asexually By sporangiospores reproduce?
1097) How do zygomycota sexually reproduce? By zygospores
1098) How do ascomycota asexually reproduce? By conidia
1099) How do zygomycota sexually reproduce? By ascospores
1100) How do basidiomycota sexually reproduce?
Via basidiospores (on basidia)
By conidia 1101) How do deuteromycota asexually reproduce?
1102) What are three reproductive forms? Teleomorph, Anamorph, Synanomorph
Teleomorph 1103) What reproductive form is sexual?
1104) What reproductive form is asexual?
1105) What reproductive form has different
Anamorph
Synanomorph asexual forms in the same fungus?
1106) What fungal infections involve the hair, skin, or nails without direct invasion of deep tissue?
1107) What fungal infections are confined to subcutaneous tissue without dissemination?
1108) What fungal infections often involve the lungs but can disseminate to any organ?
Superficial cutaneous mycoses
Subcutaneous mycoses
Systemic mycoses
1109) What fungal infections occur in patients who are immunocompromised and can become systemic?
Opportunistic mycoses
1110) What type of pathogens do you find in fungal diseases?
Primary and opportunistic
1111) What are four common virulence factors? 1) Size of the organism
2) Ability to grow @ 37̊ C@ neutral pH
3) Conversion from mycelial form to yeast or spherule form
4) Toxin production
Antibiotic and antifungal should be in culture media.
1112) How should clinical specimens for respiratory secretions be collected?
1113) How should clinical specimens for cerebrospinal fluid be collected?
1114) How should clinical specimens for hair, skin, and nail scrapings be collected?
1115) How should clinical specimens for vaginal be collected?
Should be filtered before culturing.
Mycosel agar should be used.
Selective and inhibitory plates should be used
74
PPT Flashcards
1116) How should clinical specimens for tissue, bone marrow, and sterile body fluids be collected?
All tissues should be minced before culturing
1117) What are two other types of clinical specimens?
Blood and urine
1118) mycosel culture?
1120)
What is the recommended media for
What is the correct temperature to incubate a mycosel culture?
1) With and without cycloheximide
2) With and without an antibacterial agent
1119) Why are agar plates preferred over screw1) Better aeration capped agar for mycosel culture? 2) Larger surface area
3) Greater ease of handling
Room temperature (30̊ C)
1121) How many days do you incubate a mycosel culture?
1122) What is the humidity range to incubate a mycosel culture?
1123) How often should you examine a mycosel culture during incubation?
Minimum of 21 – 30 days
Humidity range of 40% - 50%
Examine at least three (3) times a week
1124) What are 6 direct detection methods used 1) Potassium hydroxide (KOH) preparation to observe mycoses? 2) Calcofluor white stain (superior to KOH)
3) India ink stain
4) Lactophenol cotton blue mounts
5)
Grocott’s methenamine silver (GMS) stain
6) Periodic acid-Schiff (PAS) stain
1125) What colonial morphologic characteristics of mold should be noted on the front and reverse surfaces?
Color
1126) What are 3 types of topography when 1) Verrucose studying colonial morphologic characteristics 2) Umbonate of mold?
1127) What is verrucose topography?
3) Rugose
Furrowed or convoluted
1128) What is umbonate topography?
1129) What is rugose topography?
Slightly raised in the center
Furrows radiate out from the center
1130) What are 3 types of texture when studying Cottony colonial morphologic characteristics of mold? 2) Granular
3) Wooly
Loose, high aerial mycelium 1131) What is cottony texture?
1132) What is granular texture?
1133) What is wooly texture?
Dense and powdery
High aerial mycelium that is slightly matted down
1134) What are four types of microscopic preparation?
1)
2)
3) Tease mount
4) Microslide culture
Adhesive-tape mount
Wet mount
75
PPT Flashcards
1135) What type of mold produces morphologic characteristics that are: freely branching
“antlerlike” appearance; racquet hyphae; spiral hyphae?
1136) What structure of mold, used in sporulation, is a large structure containing sexual spores (asci)?
1137) What structure of mold, used in sporulation, are spores contained in the asci?
1138) What structure of mold, used in sporulation, is used in asexual reproductive cycle?
1139) What structure of mold, used in sporulation, that contain the conidia?
1140) What is a single conidiophore strand called?
1141) What is a conidiophore that is small and unicellular called?
1142) What is a conidiophore that is large and multiseptate called?
1143) What structure of mold, used in sporulation, is a fragment of hyphae the forms spores (square)?
1144) What structure of mold, used in sporulation, is formed directly from hyphae but is round?
1145) If the chamydoconidia form within the hyphae, what is it called?
1146) If the chamydoconidia form on the end of the hyphae, what is it called?
1147) What structure of mold, used in sporulation, is a saclike structure containing sporangiospores only in zygomycetes
(asexual phase)?
1148) What structure of mold, used in sporulation, sexual phase of zygomycetes?
Chapter 60
1149) Rhizopus, Mucor, Lichtheimia,
Syncephalastrum, Cunninghamella are categorized under
1150) Are large, ribbonlike hyphae
Occasional septa
Sporangiospores—Internally spherical spores
Sporangiophore—Supporting structure for sporangium
Dermatophytes
Asocarp
Ascospores
Conidia
Conidiophores
Phialide
Micoconidia
Macroconidia
Arthroconidia
Chamydoconidia
Intercalary
Terminal
Sporangium
Zygospores
Zygomycetes
Zygomycetes
76
PPT Flashcards
1151) Saclike fruiting structures
1152) Supporting structure for sporangium
1153) Is found on decaying organic matter, bread, or in the soil.
1154) Infection is acquired through inhalation, percutaneous routes, or the ingestion of spores.
1155) Appear fluffy.
Are white-gray to brown.
Hyphae are grayish and dotted with dark sporangia.
1156) Patients who are immunocompromised are at risk zygomycosis.
1157) Uncontrolled diabetes and those with prolonged drug therapy are prone to
1158) Vascular invasion, particularly rhinocerebral
Tissue thrombosis and/or necrosis
Perineural invasion
Lung infections
1159) Gastrointestinal (GI) infections are examples diseases of
1160) Infected hairs do not fluoresce under
Wood’s lamp (ultraviolet [UV]).
1161) Two types of invasion by trichophyton are
1162) Hair shaft is filled with arthroconidia.
1163) Spores are found around the hair shaft.
1164) Hair shaft is filled with arthroconidia
1165) is an example of an invasion by
1166) Spores are found around the hair shaft is an example of invasion by
1167) Macroconidia—Smooth, club-shaped, and thin-walled is a description of
1168) Microconidia—Spherical, pyriform
(teardrop), or clavate (clublike) is a description of
1169) Does not perforate hair.
Is slow growing.
Has a cherry-red reverse surface.
Colonies are fluffy or granular.
1170) Perforates hair, Is rapid growing, has an orange-red reverse surface.
Colonies are downy or granular.
Sporangia found in zygomycetes
Sporangiophore
Zygomycetes
Zygomycetes
Morphologic Characteristics of zygomycosis
Uncontrolled diabetes
Zygomycosis
Zygomycosis
Zygomycosis
Trichophyton
Endothrix and Ectothrix—
Endothrix caused by invasion Trichophyton
Ectothrix caused by invasion of
Trichophyton
Trichophyton
Trichophyton
Trichophyton
Trichophyton
Key features of T. rubrum
Key features of T. mentagrophytes
77
PPT Flashcards
1171) Thin-walled, Smooth-walled, Multicelled
Cigar-shaped (three to eight septa) are key features of
1172) Thin-walled, Smooth-walled, Cigarshaped (two to five septa), Narrow attachment to base
1173) Large, spindle-shaped, rough-walled macroconidia
1174) Thick walls with four or more septa
Macroconidia of T rubrum
Macrocinidia of T. mentagrophytes
Microsporum
1175) Small and club-shaped microconidia are charateristics of
1176) Cultures that produce aerial hyphae
1177) Texture—Velvety, powdery, glabrous, or
Microsporum
Microsporum
1179) Causes Tinea capitis among schoolchildren.
Microsporum cottony
1178) Color—Whitish, buff to cinnamon brown Microsporum
M. audouinii
Is spread by infected hair.
Infected hair shafts fluoresce yellow-green.
1180) Causes ringworm in children and adults. M. canis
Is spread by infected animals.
1181) Infected hair shafts fluoresce yellowgreen.
1182) Cause tissue invasion in individuals who are immunocompromised.
1183) Organisms are saprophytic and therefore difficult to diagnose.
M. canis
Opportunistic Mycoses
Opportunistic Mycoses
1184) All fungi should be identified in these patients.
1185) Are acquired through:Construction,
Demolition, Remodeling, Hospital visits
1186) Usually green to blue-green colonies
1187) Velvety surface, Hyaline septate hyphae
Brushlike conidiophores are characteristics of
1188) Is found in the Ohio and Mississippi River
Valley regions.
1189) occurs in dogs and humans.
Opportunistic Mycoses
Opportunistic Mycoses
Penicillium
Penicillium
Blastomyces dermatitidis
1190) Produces acute or chronic suppurative and granulomatous infections.
1191) Large, spherical, thick-walled yeast (8 to
15 μm)
Single bud connected to the parent cell
1192) Is found in the desert southwest of the
United States.
Blastomyces dermatitidis
Blastomyces dermatitidis
Blastomyces dermatitidis
Coccidioides immitis
1193) Is acquired by inhalation of arthroconidia. Coccidioides immitis
78
PPT Flashcards
1194) Causes respiratory tract infections.
Is considered a “select agent.”
1195) Nonbudding, thick-walled spherule (20 to
200 μm)
1196) Spherules containing nonbudding endospores
1197) Is associated with the inhalation of aerosolized conidia:
1198) Chicken houses
Roosting places for birds (e.g., starlings)
Bat guano (in caves) are examples of
1199) Produces chronic, granulomatous infection.
1200) May be detected in bone marrow or blood using Wright stain.
Is intracellularly found in cells as small, round-to-oval yeast cells (2 to 5 μm).
1201) Demonstrates tuberculate macroconidia
(mycelial form).
1202)
Is referred to as the “rose gardener’s” disease.
1203) Is acquired through trauma (thorns).
1204) Appears as round-to-oval cigar-shaped yeast cells.
1205) Demonstrates ovoid microconidia in mycelial form.
Chapter 61
1206) What are the accidental hosts of
Dematicaceious Molds?
1207) What is involved?
1208) What are the two classifications of
Dematicaceious Molds?
1209) What is a slow growing Dematicaceious
Mold?
1210) What is rapid growing Dematicaceious
Mold?
1211) What are the agents of superificial and subcutaneous mycoses?
1212) What are the slow growers?
Coccidioides immitis
Identification of Coccidioides immitis
Coccidioides immitis
Histoplasma capsulatum aerosolized conidia found in Histoplasma capsulatum
Histoplasma capsulatum
Histoplasma capsulatum
Histoplasma capsulatum
Sporothrix schenckii
Sporothrix schenckii
Sporothrix schenckii
Sporothrix schenckii
Humans and animals
Skin and subcutaneous tissue
They are slow growing and rapid growing
Slow growing in 7 to 10 days
Rapid growing in less than 7 days
Dematicaceious Mold
Cladosporium spp., Ochroconis gallopava,
Exophiala dermatidis, Hortaea jeanselmei ,
H. werneckii , Fonsecaea spp., Phialophora spp., Piedraia hortae , Madurella mycetomatis
79
PPT Flashcards
1213) Which are the rapid growers? Alternaria spp., Bipolaris spp., Curvularia spp.,
Drechslera spp., Exserohilum spp.,
Pseudallescheria boydii , Cladophialophora bantiana
Tinea nigra and Black piedra 1214) What are the superficial infections?
1215) What is Tinea nigra?
1216) What is the hair and scalp infection caused by Piedraia hortae ?
1217) What is the chronic granulomatous infection involving lower extremities?
1218) What are the two types of Mycetoma?
Skin infection caused by
Black piedra
Mycetoma
Horaea werneckii
Bacterial (actinomycotic) or fungal
(eumycotic)
1219) What is the chronic infection acquired by traumatic inoculation into skin?
1221) What are the infections from brownish
Chromoblastomycosis
1220) How is chromoblastomycosis identified? By lesions revealing sclerotic bodies and resembling copper pennies
Phaehyphomycosis yeastlike cells, pseudohyphae or hyphae?
1222) What does Hortaea werneckii infect? Skin
1223) What does Horatea werneckii look like? Tissue contains hyphal fragments and budding yeast
1224) What does Piedraia hortae infect?
1225) What does Piedraia hortae look like?
Hair
Tissue contains asci-containing nodules cemented to hair shafts.
Mostly in tropical and subtropical regions 1226) Where can agents of Mycetomas be found?
1227) Who are most affected?
1228) What are the two fungal mycetomas?
1229) What are the white grain mycetomas?
Infections occur in those who have outdoor occupations
White and black grain
1230) What are the black grain mycetomas?
Pseudallescheria boydii , Acremonium ,
Fusarium spp.
Madurella mycetomatis , Exophiala jeanselmei , Curvularia
In 5 to 10 days 1231) How fast can Pseudallescheeria boydii grow?
1232) What does Pseudallescheria boydii look like?
It is initially white and fluffy but becomes brownish-gray.
1233) What is the reverse surface of
Pseudallescheria boydii ?
1234) What is the reproduction of
Pseudallescheria boydii?
1235) What are the two anamorph morphologies of asexual reproduction?
1236) What is Scedosporium apiosermum ?
1237) What are the agents of chromobastomycosis?
Tan to dark brown
Asexual and sexual.
Culture-based and Graphium stage
Asexual reproduction
Cladosporium, Cladophialophora,
Phialophora and Fonsecaea
80
PPT Flashcards
1238) What are the sclerotic bodies and septate hyphae are observed in subcutaneous tissue?
1239) What is the septate hyphae that occurs in tissue?
1240) What is Phialophora ?
Cladosporium
Cladophialophora
1241)
1242)
1243)
Where can hyphae be found?
Where is Fonsecaea
What are the agents of
Phaeohyphomycosis?
found?
Sclerotic bodies and septate hyphae are found in subcutaneous tissue
Joints
Sclerotic bodies are observed in subcutaneous tissue and septate hyphae are observed in brain and lung tissue
Alternaria, Bipolaris, Drechslera,
Curvularia, Exophiala jeanselmei,
Exophiala dermatitidis and Exserohilum
Alternaria and Curvularia 1244) Which agents of Phaeohyphomycosis are fluffy and gray to gray-brown or gray-green?
1245) Which agent of Phaeohyphomycosis is gray-green to dark-brown colonies?
1246) Which agents of Phaeohyphomycosis are gray-green to dark brown?
1247) What color is the hyphae of Alternaria ?
1248) What does the conidia of Alternaria look like?
1249) What is the septa shape of Alternaria ?
1250) Where are the germ tubes of Bipolaris ?
1251) How does the hilum of Bipolaris protrude?
1252) How are the oblong conidia arranged?
1253) What is the conidiophores shape of
Bipolaris ?
1254) What is the conidiophores shape of
Curvularia ?
1255) What does the conidia of Curvularia look like?
1256) What are the similarities of E. jeanselmei and E. dermatitidis ?
1257) What differentiates E. jeanselmei from E. dermatitidis ?
1258) What differentiates
E. jeanselmei ?
E. dermatitidis
Chapter 62
1259) True/False:
Pneumocystis jirovenci is not an opportunistic, atypical fungus from
Bipolaris
Drechslera and Exserohilum
Golden-brown
Large brown conidia resembling a drumstick
Horizontal and longitudinal
At one or both ends
Slightly
Sympodially
Bent
Geniculate
Golden-brown, multicelled, curved with a swollen central cell
Slow growers, shiny colonies, velvety with age, elongated and grows at 37 ⁰ C
It has shiny brown colonies with elongated conidiophores with tapered tip. It uses potassium nitrate and only grows at 37 ⁰ C.
It has shiny black colonies with elongated tubular annellophores. It does not use potassium nitrate. It grows at 37 ⁰ C and 40 to 42 ⁰ C.
False
81
PPT Flashcards
1260) What organism infects individuals that are immunocompromised?
1261) What is another way that pneumocystis pneumonia is expressed?
1262) What is the lifecycle of Pneumocystis jirovenci?
1263) What are major characteristics that differ from other fungi?
Pneumocystis jirovenci
PCP
Trophozoite,
Precyst (sporocyte),
Cyst (diagnostic form)
Cell membrane contains cholesterol.
Trophozoite form is susceptible to osmotic disturbances.
Has one to two copies of the ribosomal subunit gene
Transmission is unknown; it may be person to person
Pneumocystis jirovenci
1264) How can Pneumocystis jirovenci be transmitted?
1265) What is the most common opportunistic infection in patients with human immunodeficiency virus or acquired immunodeficiency syndrome (HIV/AIDS)?
1266) What infection is species specific to rodents?
1267) What infection is species specific to humans?
1268) Where do the inhaled organism that adheres to pneumocytes replicate?
1269) Where does the inflammatory response occur?
1270) What are symptoms of Pneumocystis jirovenci?
P. carinii
P. jiroveci
Extracellularly
Interstitial mononuclear
1271) diagnosis?
1272) Name 3 stains that aid in the diagnosis of
Pneumocystis jirovenci?
1273) for
1274)
What kind of specimen is needed for a
What are other methods for identification
Pneumocystis jirovenci ?
What are the morphologic characteristics of trophoozoites of Pneumocystis jirovenci?
Nonproductive cough,
Low-grade fever,
Dyspnea,
Chest tightness,
Night sweats
Bronchoalveolar lavage fluid (BAL) or induced sputum,
Biopsy material
Calcofluor white,
Methenamine silver,
Immunofluorescent staining
Commercial kits using monoclonal antibodies,
Nucleic acid amplification
Are the predominant form but difficult to visualize,
Have flexible walls (pleomorphic),
Outnumber cysts, 10 to 1
82
PPT Flashcards
1275)
1277)
1278)
1279)
1280)
What are the morphologic characteristics of cysts of Pneumocystis jirovenci
Chapter 63
1276) What is an example of a
Eukaryotic/Unicellular organism?
?
What is the shape and size of yeast?
How does yeast reproduce?
What morphologic characteristics does yeast express?
What are the Three genera of yeast?
1281) Which genera of yeast is the most common opportunistic fungal infection?
1282) Which genera of yeast is associated with avian excreta, infection are acquired from aerosolization, and Telemorphic form is
Filobasidiella neoformans?
1283) What yeast species causes these types of disease?
Oroesophageal candidiasis
Intertriginous candidiasis
Paronychia—Infection of nails
Onychomycosis—Infection of nails and nail beds
Perlèche respiratory infections
Vulvovaginitis
Thrush
Pulmonary infection
Eye infection
Endocarditis
Meningitis
Disseminated infection
1284) What yeast species causes these types of disease?
Infections emerge in certain populations of patients:
Older adults
Patients with malignancies
Patients in oncology care settings
Patients in neonatal intensive care units
Round to oval (2 to 60 μm)
Asexually by budding and Sexually by ascospores or basidiospores
A.
Germ tube – Tubular outpouch of cell wall
B.
Pseudohyphae – Elongated buds that form subsequent buds.
1.
Candida spp.
2.
Cryptococcus
3.
Trichosporan and Malassezia
Candida spp.
Are spherical to concave,
Are uniform in size (4 to 7 μm),
Do not bud,
Contain intracystic bodies.
Yeast
Cryptococcus
Candida albicans
Non-albicans candida
83
PPT Flashcards
1285) Which of the yeast genera can manifests as an acute, subacute, or chronic infection?
1286) What are some examples of certain
Cryptococcus neoformans
Initial presentation is a pulmonary conditions that can be cause by Cryptococcus neoformans? infection.
May migrate to the central nervous system
(CNS), especially in individuals who are immunocompromised.
Disseminated cryptococcosis:
Painless papular skin lesions
Endocarditis
Hepatitis
Renal infection
1287) How does yeast protect themselves from environmental stress and protect themselves
Contains a polysaccharide capsule from phagocytes?
1288) What are some examples of diseases that is caused by Trichosporon?
Causes trichosporonosis.
Disseminated trichosporonosis (most common)
Skin lesions
Endocarditis
Endophthalmitis
Brain abscess
Respiratory infections
May cause white piedra in patients who are immunocompetent.
1289) What are two species of Malassezia?
Malassezia furfur
Malassezia pachydermatis
1290) What disease does Malassezia furfur cause?
Causes tinea versicolor.
Brownish scaly lesions on light-skinned
1291) What disease does Malassezia pachydermatis cause?
1292) How to diagnose Candida? persons
Light lesions on dark-skinned persons
Is a disseminated infection in young children.
Malassezia pachydermatis
Is recovered from skin lesions.
May cause fungemia in patients who are immunocompromised.
Stains
Cultivation
Identification
1293) How would Blastoconidia or
Pseudohyphae stain?
Strongly gram positive
1294) What would the cultivation of candida look like?
Smooth, Creamy white colonies
84
PPT Flashcards
1295) How to identify Candida?
Germ tubes or chlamydoconidia on cornmeal agar
C. albicans— Production of both betagalactose-aminidase and
1296) neoformans?
1297) stain?
1298)
How to diagnose Cryptococcus
How would Cryptococcus neoforms
What would the cultivation of
Cryptococcus neoformans expresss?
1-proline aminopeptidase
Use of specific substrates
Fermentation of carbohydrates
CHROMagar Candida culture medium
Peptide nucleic acid fluorescent in situ hybridization (PNA-FISH)
Stains
Cultivation
Identification
India ink delineates the large capsule.
Organisms appear as spherical, budding, thick-walled yeast with a capsule.
Grows on routine fungal media without cycloheximide.
Colonies appear smooth white to tan and
1299) How to identify Cryptococcus neoformans?
1300)
1301)
How to diagnose Trichosporon
How would Cryptococcus neoforms stain?
are mucoid and creamy.
Presumptive identification is based on rapid urease.
Substrate utilization patterns are identified.
Pigment is produced on niger seed agar.
Antigen is detected (latex agglutination).
Stains
Cultivation
Identification
Hyaline hyphae
Numerous arthroconidia
Few blastoconidia
Cream-colored, heaped, and dry-to-moist 1302) What would the cultivation of
Trichosporon expresss?
1303) How to identify Trichosporon? wrinkled colonies
Presence of rectangular arthroconidia with
1304) How to diagnose Malassezia? round ends
Presence of septate hyaline hyphae
Urease positive
Substrate utilization profile
Stains
Cultivation
Identification
1305) What would the cultivation of Malassezia
Infrequently cultured expresss?
Positive blood cultures on agar overlaid with olive oil
85
PPT Flashcards
1306) How to identify Malassezia?
Growth on overlaid agar
“Bowling pin” or “pop bottle” morphologic
1307) What are some examples of Yeast identification systems? feature
API-20C AUX Yeast System
Uni-Yeast Tek System
MicroScan Yeast Identification Panel
Vitek Biochemical Cards
CHROMagar
RapID Yeast Plus System
1308) Conventional identification Methods can identify up to what percentage of yeast?
1309) Cornmeal agar determines if the yeast produces what?
75% of yeasts
Blastoconidia
Arthroconidia
Pseudohyphae
True hyphae
Chlamydoconidia
1310) Carbohydrate utilization works by? Uses carbohydrate-containing filter paper disks.
1311) agar?
Phenoloxidase is detected using what
Chapter 64
1312) Standards for antifungal susceptibility testing have been developed by: niger seed agar.
Clinical Laboratory Standards Institute
(CLSI)
1313) Guidelines for what are provided in three documents (M27-AS, M38-A, and M44-A)?
1314) Document M27-AS provides specific guidelines with what aspect of antifungal susceptibility testing?
1315) Document M38-A provides specific guidelines with what aspect of antifungal susceptibility testing?
1316) Document M44-A provides specific guidelines with what aspect of antifungal susceptibility testing?
1317) What is one disadvantage of antifungal susceptibility testing?
1318) To determine antibiograms for isolates in an institution, to aid in the management of patients with refractory oropharyngeal candidiasis, and to aid in the management of patients who have invasive candidiasis when the use of the azoles is questioned in infections caused by non– Candida albicans are all reasons why this form of testing may be of value: antifungal susceptibility testing
Reference method for broth dilution susceptibility testing of yeasts
Reference method for broth dilution susceptibility testing of filamentous fungi
Method for antifungal disk diffusion of yeasts
Tests are costly and time-consuming antifungal susceptibility testing
86
PPT Flashcards
1319) Problems that complicate interpretive guidelines in antifungal susceptibility testing include:
Physical condition of the patient, type of infection and ability of the drug to penetrate a closed space, dose of the drug and its pharmacokinetics, and susceptibility testing method used and serum level of drug administered
Agents contain multiple conjugated double bonds and one to three ring structures
1320) Polyene macrolide antifungal agents are noted for what unique structure and bond configuration?
1321) Amphotericin B, nystatin, griseofulvin, and 5-fluorocytosine (flucytosine) are all examples of what?
1322) Which polyene macrolide antifungal agent is produced from Streptomyces noursei and is used to treat oral or vulvovaginal candidiasis?
1323) Which polyene macrolide antifungal agent is produced from Penicillium and is the oral agent for dermatophytoses?
1324) Which polyene macrolide antifungal agent inhibits protein and deoxyribonucleic acid (DNA) synthesis and acts synergistically with amphotericin B?
1325) Amphotericin B agents are produced by what organism?
1326) Which class of polyene macrolide antifungal agents is intravenously infused to treat: Invasive aspergillosis, Candida spp,.
Cryptococcus, and Zygomycetes members?
1327) Amphotericin B agents bind to ereosterol in which structure of the cell?
1328) Amphotericin B agents may cause insufficient function in which organ of the human body?
1329) Pseudallescheria boydii , Aspergillus terreus , Trichosporon spp, and Fusarium spp are all fungi resistant to which antifungal agent?
1330) Which type of antifungal agent disrupt the integrity of the cell membrane and inhibit synthesis of ergosterol?
1331) Clotrimazole, miconazole, fluconazole, ketoconazole, itraconazole, and vorivonazole are all examples of which class of antifungal agent?
Polyene macrolide antifungal agents nystatin griseofulvin
5-fluorocytosine (flucytosine)
Streptomyces nodosus
Amphotericin B agents cell membrane kidneys
Amphotericin B agents
Azole antifungal agents
Azole antifungal agents
87
PPT Flashcards
1332) Which azole antifungal agents are used for mild cases of dermatophytosis and tinea versicolor?
1333) Which azole antifungal agent provides excellent activity toward Candida spp. and
Cryptococcus neoformans ?
1334) Which azole antifungal agent is used for mild cases of paracoccidioidomycosis?
1335) Which azole antifungal agent provides a broader spectrum than ketoconazole?
1336) Which azole antifungal agent is active against Fusarium and fluconazole-resistant yeasts?
1337) Which antifungal agent main mechanism of action is to inhibit glucan synthesis (1,3 beta-glucan synthase)?
1338) Caspofungin, micafungin, and anidulafungin, are all examples of what type of antifungal agent?
1339) Which type of echinocandin agent Is used for Candida spp., including fluconazoleresistant yeasts; has fungistatic properties against Aspergillus spp; but is ineffective against Candida neoformans ?
Chapter 65
1340) The characteristics of being microscopic, obligate parasites, and displaying tropism describe what agent?
1341) What agent is capable of infecting animals, plants, and bacteria?
1342) Virion structure generally include what 3 components?
1343) Which virion component protects the viral genome?
1344) Which virion component aid viral entry into a host cell?
1345) What organization determines the classification of viruses?
1346)
1347)
Virus classification is based on what 3 properties?
The viral infectious cycle consists of what
6 steps?
Clotrimazole and miconazole fluconazole ketoconazole
Itraconazole vorivonazole
Echinocandin Agents
Echinocandin Agents
Caspofungin
Viruses
Viruses
Viral genome, capsid, lipid envelope
Capsid
Lipid envelope
International Committee on Taxonomy of
Viruses (ICTV) of the Virology Division of the International Union of Microbiology
Societies
Viral morphology, genome type, and envelope presence/absence
Attachment, penetration, uncoating, macromolecular synthesis, viral assembly, and viral release
88
PPT Flashcards
1348) What 3 clinical presentations can manifest from a viral infection?
1349) Following a viral infection, what 5 outcomes can result?
Acute, latent, or chronic infection
Viremia, dissemination to other body tissues, symptomatic disease, antibody or cell-mediated immunity, or tissue damage
1350) Clinical Viral Services have increased in demand due to what?
Introduction of virus-specific drugs, development of rapid diagnostic tests, available cell lines for culture, RT-PCR detection of viral genomes, and appearance of emerging pathogens
1351) Virology laboratory can include what? BSC, fluorescent microscopes, inverted bright-field microscope, refridgerated centrifuge, incubator, and roller drum
1352) Virology lab scientists must be familiar in what 4 types of tests?
1353) Specimen collection for viral testing include what sample types?
1354) Enteroviruses, influenza, and adenoviruses are tested in what specimen type?
1355) Measles, mumps, rubella are tested in what specimen type?
1356) Which body fluid is collected for CMV testing?
1357) How are enteroviruses tested?
1358) How is HSV tested?
1359) How are influenzas A and B tested?
Cell culture, EIA, Immunofluorescence, molecular methods
Throat/Nasopharyngeal swab, urine, lesion, blood, bone marrow, stool
Throat/nasopharyngeal swab
Urine
Blood
Cell culture and PCR
Cell Culture
Cell culture, shell vial culture, EIA, direct staining using FA, and RT-PCR
1360)
1361)
How are noroviruses tested?
How is RSV tested?
RT-PCR
Direct fluorescent staining, R-mix cells, cell culture, rapid nonculture tests
Tzanck test 1362) What test is used to detect VZV and HSV, and uses a stained smear of cells from the base of a skin vesicle?
1363) What procedure is used to detect influenza
A/B/C-infected cells by adsorption of guinea pig RBCs to the outer membrane of infected cells?
Hemadsorption
1364) Conventional culture terms include what? Monolayer, primary cells, semicontinuous
(diploid) cells, and continuous cells
1365) Growth Cell culture media includes what? Serum rich growth medium to support rapid cell growth
1366) How is a maintenance media different Less serum, to keep cells in a steady state from a growth media?
1367) Under what conditions are cell cultures incubated? of metabolism
1-4 weeks at 35-37 deg C.
89
PPT Flashcards
1368) Dead or dying culture cells due to viral infection are called what?
1369) What are common cell lines used in clinical laboratories?
Cytopathic effect
1370) What cell line is best for influenza testing? PMK
1371) What cell line is best for VZV testing?
1372) What cell line is best for HSV testing?
HDF
HDF, HEp-2
1373) What cell line is best for CMV testing?
1374) Which culture type allows for early virus detection, contains a stainable cover slip, and
Rhesus, MRC-5, lung fibroblasts, HEp-2,
A-549, human dermal fibroblasts (HDF)
HDF
Shell vial culture involves viruses grown in shell vials?
1375) What disease conditions are causes by
VZV?
1376) What virus causes the patient to initially exhibit varicella and establishes latency in the dorsal nerve root ganglion?
Chicken pox and shingles
VZV
Deoxyribonucleic Acid (DNA),
Ribonucleic Acid (RNA)
Chapter 66
1377) Name two virus families?
1378) Is Adenoviridae in DNA or RNA virus classification?
1379) Is Hepadnaviridae in DNA or RNA virus classification?
1380) Is Herpesviridae in DNA or RNA virus classification?
1381) Is Papillomaviridae in DNA or RNA virus classification?
1382) Is Parvoviridae in DNA or RNA virus classification?
1383) Is Polyomaviridae in DNA or RNA virus classification?
1384) Is Poxviridae in DNA or RNA virus classification?
1385) Is Arenaviridae in DNA or RNA virus classification?
1386) Is Astroviridae in DNA or RNA virus classification?
1387) Is Bunyaviridae in DNA or RNA virus classification?
1388) Is Caliciviridae in DNA or RNA virus classification?
1389) Is Coronaviridae in DNA or RNA virus classification?
1390) Is Filoviridae in DNA or RNA virus classification?
1391) Is Orthomyxoviridae in DNA or RNA virus classification?
DNA virus
DNA virus
DNA virus
DNA virus
DNA virus
DNA virus
DNA virus
RNA virus
RNA virus
RNA virus
RNA virus
RNA virus
RNA virus
RNA virus
90
PPT Flashcards
1392) Is Paramyxoviridae in DNA or RNA virus classification?
1393) Is Picornaviridae in DNA or RNA virus classification?
1394) Is Reoviridae in DNA or RNA virus classification?
1395) Is Retroviridae in DNA or RNA virus classification?
1396) Is Rhabdoviridae in DNA or RNA virus classification?
1397) Is Togaviridae in DNA or RNA virus classification?
1398) How many serotype have been described in Adenoviruses?
1399) How many species Adenoviruses are divided into?
1400) Name the virus that causes Respiratory and gastrointestinal diseases
Severe and acute respiratory disease in new military recruits
1401) What Adenoviruses serotype vaccines were developed for 1971 through 1996?
1402) What type of Adenovirus occurs in individuals of all ages?
1403) Name human respiratory viruses?
1404) What viruses cause colds, tonsillitis, pharyngitis, and croup?
1405) What viruses are acquired through contact with contaminated respiratory secretions, stool, and fomites?
1406) What viruses Cause influenza?
1407) What virus is acquired through the inoculation of mucous membranes with secretions from fomites or aerosolized droplets?
1408) What are the three types of influenza?
1409) How three types of influenza are distinguished?
1410) What Influenza causes subclinical infections?
1411) Name two subdivision of Influenza A
RNA virus
RNA virus
RNA virus
RNA virus
RNA virus
RNA virus
Fifty-two (52) seven species—A through G
Adenoviruses serotypes 4 and 7
Adenovirus type 14
Adenoviruses
Orthomyxoviruses
Paramyxoviruses
Picornaviruses (rhinovirus)
Adenoviruses
Adenoviruses
Orthomyxoviruses
Parainfuenza
A, B, and C on the basis of matrix protein and nucleoprotein
Influenza C hemagglutinin (HA) neuraminidase (NA).
91
PPT Flashcards
1412) What type of Influenza A circulate in humans?
1413) What are the current strains of Influenza
A?
1414) What antigenic occurs when genome gradually changes?
1415) What antigenic occurs when Influenza A acquires a new HA or NA gene?
1416) Name two viral genome
1417) What does make the formulation of a vaccine challenging?
1418) In what animal avian and human viruses can be replicated?
1419) What type of Influenza occurs when a global outbreak of illness causes serious illness against which little immunity exists?
1420) Following are historic example of what type of influenza?
Spanish 50 million deaths
Mexico, 2009 (H1N1)—18flu of 1918
(H1N1)—25 to ,449 deaths
Avian “bird flu” (H5N1)—309 deaths
1421)
What viral infection causes the “common cold”?
1422) What virus is transmitted by Selfinoculation through the eyes or nose, and
Direct contact of aerosols?
1423) Name the viral infection when these
Symptoms are seen: watery nasal discharge, headache, malaise, sneezing, nasal congestion, sore throat, and cough.
1424) How many serotypes do Rhinoviruses have?
1425) What medium and what temperature is required to grow Rhinovirus?
1426) Is Rhinovirus test often required?
1427) How does Cytopathic effect (CPE) appear in Rhinovirus test?
1428) What animal transmits Arboviruses?
1429) Name the three taxonomic families which
Arbovirus occurs.
1430) virus) belongs to what family virus?
1431)
California encephalitis group (La Crosse
How Bunyavirus is transmitted?
Only H1, H2, H3, and N1 or N2
H1N1, H3N2 (highly pathogenic), and
H1N2.
Antigenic drift
Antigenic shift
Antigenic shift and Antigenic drift
Continual change in the viral genome
Swine
Pandemic Influenza
Pandemic Influenza
Rhinovirus
Rhinovirus
Rhinovirus viral infection
Over 100 serotype
Virus grows in MRC-5 cell lines at a reduced temperature (30ºC).
It is not often required
Cytopathic effect (CPE) appears as large and small round refractile cells.
Arthropod
Bunyaviruses
Flaviviruses
Alphaviruses (Togaviridae family)
Bunyaviruses
Transmitted by mosquitoes, ticks, and sandflies
92
PPT Flashcards
1432) Following are the main pathogenic of what type of viruses?
Yellow fever, dengue fever, West Nile virus,
Flavivirus
Japanese encephalitis, and St. Louis encephalitis virus
1433) What are the main vectors for Flavivirus? Mosquitoes
1434) Following are the main pathogenic of what family viruses?
Alphaviruses Family
Eastern, Western, and Venezuelan equine encephalitis
1435) What are the main vectors for mosquitoes
Alphaviruses?
1436) What type of viral encephalitis are St.
Louis and West Nile viral encephalitis
Arbovirus
(Flavivirus)?
1437) What type of viral encephalitis is La
Crosse virus (Bunyavirus)?
1438) What type of virus is Herpes simplex virus–type 1 (HSV-1)
1439) What type of virus causes Subacute sclerosing panencephalitis disease?
1440) Equine encephalitis (alphavirus) is an example of what type of disease?
1441) Following viruses cause what type of disease?
Rabies
Enteroviruses
Human immunodeficiency virus (HIV)
John Cunningham (JC) virus
Arbovirus
Viral encephalitis
Measles virus
Viral encephalitis
Viral encephalitis
1442) This virus can be transmitted sexually
1443) This virus can be transmitted sexually
1444) This virus can be transmitted sexually
1445) This virus can be transmitted sexually
1446) This virus can be transmitted sexually
1447) This virus can be transmitted sexually
1448) This hepatitis virus can causes acute or chronic disease
1449) Hepatitis C causes what type of cancer?
1450) Name a test is used to diagnose Hepatitis
C
1451) What is a predictor of Hepatitis C?
1452) Name a treatment for Hepatitis C
1453) What family of viruses does HPV belong to?
1454) How many genotypes do HPVs have?
Hepatitis B
Hepatitis C
HSV
HPV
HIV
Human T-lymphotropic virus (HTLV)
Hepatitis C
Hepatocellular carcinoma
Serology test
Viral genotyping
Interferon
Papillomaviridae
More than 200 genotypes
93
PPT Flashcards
1455) How many sexually transmitted do HPVs have?
1456) Name a virus which exhibit tropism for cutaneous or mucosal tissue.
1457) What type of HPV causes planter wart?
1458) What type of HPVs cause genital wart?
1459) What types of HPV are most responsible for cervical cancer?
1460) Are Human Retroviruses in DNA or RNA classification?
1461) This virus Contain reverse transcriptase
(RT) enzyme, which converts RNA to DNA.
1462) Name the two human exogenous
Retroviruses.
1463) What type of virus Infects cluster of differentiation 4 (CD4) T lymphocytes, monocytes, and cells of the central nervous system (CNS)?
1464) What type of virus causes acute influenzalike disease, acquired immunodeficiency syndrome (AIDS), and malignancies?
1465) How is HIV treated?
1466) What type of Retrovirus causes T-cell leukemia and lymphoma and tropical spastic paraparesis?
1467) What symptom of disease defines as skin or rash eruption?
1468) Measles disease is most common in adult or children?
1469) What symptom is seen in Measles disease?
1470) What symptom is seen in Scarlet fever disease?
1471) Scarlet fever disease is most common in adult or children?
1472) What symptom is seen in Rubella
(German measles)?
1473) Rubella (German measles) is most common in adult or children?
1474) Erythema infectiosum is most common in adult or children?
1475) This symptom is seen in Erythema infectiosum (fifth disease caused by parvovirus B19)
1476) What symptom is seen in Roseola viral infection (HSV-6)?
More than 30
HPV
HPV-1
HPV-6, HPV-11
HPV-16 and HPV-18 cause 60% of cervical cancers.
RNA
Retroviruses
HIV and HTLVs
HIV type 1 or 2
HIV type 1 or 2
It is treated with multiple-drug therapy.
HTLV–type 1
Exanthema children
Exanthema
Exanthema children
Exanthema children children
Exanthema
Exanthema
94
PPT Flashcards
1477) Roseola viral infection (HSV-6) is most common in adult or children?
1478) What human virus HSV1 and HSV2 are belong to?
1479) What human virus Varicella-zoster virus
(VZV) belong to?
1480) What human virus Epstein-Barr virus
(EBV) belong to?
1481) What human virus Cytomegalovirus
(CMV) belong to?
1482) What human virus Human herpesvirus
(HHV) belong to?
1483) How HSVs are transmitted? children
Herpesviridae
Herpesviridae
Herpesviridae
Herpesviridae
Herpesviridae
Through infected secretions (e.g., through sexual contact).
1484) What illnesses does VZV cause?
1485) What illness does EBV cause?
1486) What congenital disease of the newborn is associated with?
1487) What type of HHVs cause respiratory infection?
1488) What type of HHV causes Kaposi sarcoma tumor?
1489) What type of virus is Rotavirus? Does it most common in adult or children?
1490) What type of virus is Adenovirus 40 through 41? Does it most common in adult or children?
1491) What type of viruses are Caliciviruses
(Norovirus, Sapovirus)? Does it most common in adult or children?
1492) What type of virus is Astrovirus? Does it most common in adult or children?
1493) What type of virus is Noroviruses? Does it most common in adult or children?
1494) What type of viral infection causes the following symptoms? chickenpox and shingles infectious mononucleosis
CMV
HHV-6 and HHV-7
HHV-8
Gastrointestinal Virus- children
Gastrointestinal Virus- children
Gastrointestinal Virus- children
Gastrointestinal Virus- children
Gastrointestinal Virus-adult
Noroviruses nausea, abdominal cramps, vomiting, and watery diarrhea
1495) What virus causes Rodent-born disease? Hantavirus
1496) How Hantavirus is transmitted? Transmitted through inhalation of rodent excreta
95
PPT Flashcards
1497) Which disease the following symptoms are related to?
After 11 to 32 days, symptoms are headache, fever, and body aches.
Symptoms progress to hemorrhagic fever, kidney disease, and acute respiratory failure.
1498) Sin Nomber virus is strain of what type of virus?
1499) How Sin Nomber is transmitted?
1500) Bayoy virus is strain of what type of virus and how it is transmitted?
1501) How Bayoy virus is transmitted?
1502) Black Creek Canal virus is strain of what type of virus?
1503) How Black Creek Canal virus is transmitted?
1504) New York–type 1 virus is strain of what type of virus?
1505) How New York–type 1 virus is transmitted?
Chapter 67
1506) What occurs when small changes or mutations in a virus reduce the effectiveness of a drug?
1507) What occurs when an infection fails to respond to therapy
1508) What organization developed laboratory standards?
1509) What are the two general methods of susceptibility testing?
1510) What method of testing measures viral replication in the presence of viral agents and measures the inhibitory effect of an antiviral agent on an entire virus population.
1511) What method of testing uses polymerase chain reaction (PCR) to detect genes known to cause resistance and uses nucleic acid of the virus to determine whether a virus possesses mutations that can cause drug resistance
1512) Who should get susceptibility testing before the initiation of therapy, when changing antiretroviral regimens and in cases of suboptimal viral load reduction
1513) Why should vaccines for influenza be reformulated each year?
Hanta pulmonary syndrome
Hantavirus
Transmitted by deer mice
Hantavirus
Transmitted by the rice rat
Hantavirus
Transmitted by the cotton rat
Hantavirus
Transmitted by the white-footed mouse
Drug resistance
Clinical resistance
Clinical and Laboratory Standards Institute
(CLSI)
Phenotypic and genotypic
Phenotypic testing
Genotypic testing
Patients with HIV because of antigenic drifts
96
PPT Flashcards
1514) What provides data to determine and predict what influenza strains will be circulating in the upcoming winter
1515) What are the two types of influenza vaccines?
1516) What are the two classes of antiviral drugs?
1517) Which class of antiviral drug prevents viral uncoating and is effective of influenza A
1518) Which class of antiviral drug inhibits NA, preventing viral release and is effective for influenzas A and B
Chapter 68
1519) What is the suffix derived from the Greek meaning blood?
1520) What is the word for an infection with bacteria in the bloodstream?
1521) What is the word for an infection with fungi in the bloodstream?
1522) What is the word for an infection by bacteria or their toxins that cause harm in the bloodstream?
1523) Shock, multiple organ failure, disseminated intravascular coagulation (DIC), and death are consequences of:
1524) What bacteria cause the most common bacterial infection?
1525) What usually colonizes the skin, oropharynx, and gastrointestinal (GI) tract?
1526) What fungi cause the most common fungal infections?
1527) The presence of fungemia usually represents?
1528) What may be transiently found in the bloodstream?
1529) What invades both blood cells and hepatic cells?
1530) Epstein-Barr virus (EBV), cytomegalovirus (CMV), and HIV are viruses that preferentially infect:
1531) Transient, continuous, and intermittent are types of:
Global surveillance
Trivalent inactivated influenza vaccine
(TIV) and Live attenuated influenza virus vaccine (LAIV)
Adamantane inhibitors and neuraminidase inhibitors
Adamantane inhibitors
Neuraminidase inhibitors
-emia
Bacteremia
Fungemia
Septicemia
Microbial invasion
Gram-positive cocci
Bacteria
Candida spp.
Infection elsewhere
Eukaryotic parasites
Malarial parasites
Red blood cells (RBCs)
Bacteremia
97
PPT Flashcards
1532) Flora are usually introduced into the bloodstream as a result of the manipulation of infected tissue or surgery involving nonsterile sites in this type of bacteremia?
1533) The immune system clears bacteria from the bloodstream in this type of bacteremia?
1534) Organisms are released into the bloodstream at a constant rate in this type of bacteremia?
1535) Bacteria are found intermittently in the bloodstream in this type of bacteremia?
1536) Organisms may be found in the bloodstream early in patients with meningitis, pneumonia, pyogenic arthritis, and osteomyelitis in this type of bacteremia?
Transient
Transient
Continuous
Intermittent
Intermittent
Intravascular Infections
Intravascular Infections
1537) What type of bloodstream infections originate in the cardiovascular system?
1538) Infective endocarditis, mycotic aneurysm, suppurative thrombophlebitis, and intravenous catheter–associated bacteremia are examples of what type of bloodstream infection?
1539) What are the two major categories of bloodstream infections?
1540) Which category of bloodstream infections enters circulation through the lymphatic system?
1541) Genitourinary tract, respiratory tract, abscesses, surgical wound infections, and biliary tract are common portals of entry for:
1542) What is initiated by damage to the cardiac endothelium?
1543) What gets deposited in the damaged cardiac endothelium?
1544) What transiently enter the bloodstream and attach to the damaged surface?
1545) What is the web of cells, fibrin, and organism is referred as?
1546) Infection causes inflammatory damage and weakens the arterial wall leading to:
1547) What is it called when the arterial wall bulges and ruptures?
1548) What has causative agents that are similar to those that cause endocarditis?
Intravascular and extravascular
Extravascular Infections
Extravascular Infections
Infective endocarditis
Platelets
Bacteria vegetation mycotic aneurysm mycotic aneurysm mycotic aneurysm
98
PPT Flashcards
1549) What is an inflammation of a vein wall?
1550)
What involves an alteration in the vein’s endothelial lining, followed by clot formation?
1551) What is a frequent complication of using intravenous (IV) catheters?
1552) Short-term, triple-lumen central venous catheters can easily become colonized with bacteria or fungi leading to:
1553) Organisms move from the catheter entry site through skin to the catheter tip in:
1554) Organisms migrate along the inside of catheter-to-catheter tips leading to:
1555) What has the following symptoms fever or hypothermia, chills, hyperventilation, respiratory alkalosis, skin lesions, hypotension or shock, and Disseminated intravascular coagulation (DIC)?
1556) What can be initiated by either exotoxins or endotoxins (e.g., lipopolysaccharide
[LPS])?
1557) What mediates hypotension or shock?
1558) What is the condition where numerous small blood vessels become clogged with blood clots, and bleeding occurs as a result of the depletion of coagulation factors?
1559) Patients who have undergone an organ transplant, older adults, individuals with malignancies, and individuals with acquired immunodeficiency syndrome (AIDS) all are:
1560) Patients with what disease have the greatest diversity of pathogens recovered from blood?
1561) What are the common causes of infections in those who are immunocompromised?
1562) What is an important step in specimen collection?
1563) Blood culture media will enhance the growth of?
1564) For adults, how much blood is in a culture bottle?
1565) How many blood culture bottles for adults?
1566) What type of environment is contained in each blood culture bottle? suppurative thrombophlebitis suppurative thrombophlebitis suppurative thrombophlebitis
IV catheter–associated bacteremia
IV catheter–associated bacteremia
IV catheter–associated bacteremia septicemia
Hypotension or shock
Cytokines
Disseminated intravascular coagulation
(DIC) immunocompromised
AIDS
Gram-positive aerobic bacteria and
Gram-negative aerobic bacteria
Careful skin preparation
Contaminants
10 to 20 mL
2
One aerobic and one anaerobic bottle or two aerobic bottles
99
PPT Flashcards
1567) For infants and children, how much blood in pediatric culture bottles?
1568) What contains a nutrient broth and an anticoagulant?
1569) What is the best anticoagulant?
1570) Ethylenediaminetetraacetic (EDTA) acid and sodium citrate are also examples of?
1571) Additives may be added to support the growth of what kind of bacteria?
1572) What culture technique has an incubation that requires a low oxidation-reduction potential?
1573) What culture technique consists of a blood culture bottle with an attached chamber containing a slide coated with agar(s)?
1574) What is the culture technique where the specimen is treated with a lysing agent and anticoagulant to ensure that the organism will be concentrated during centrifugation?
1575) In lysis centrifugation what is plated on to solid media?
1576) What culture technique is capable of rapid and accurate detection of organisms in blood specimens?
1577) BACTEC blood culture system,
BacT/ALERT microbial detection system, and ESP 80A system are examples of what?
1578) Which blood culture system uses blood or sterile body fluids that are inoculated into bottle?
1579) BACTEC blood culture system measures the production of what by metabolizing the organisms?
1580) Which blood culture system is fully automated with incubator, shaker, and detector?
1581) Which blood culture system measures
CO
2
-derived pH changes using a sensor in the bottom of each bottle?
1582) Microbial growth is detected by the consumption and/or production of gases as organisms metabolize nutrients in culture medium in which blood culture system?
1 to 5 mL
Basic medium
Sodium polyanethol sulfonate (SPS)
Anticoagulants
Bacteria with no cell wall
Conventional blood cultures
Self-contained subculture system
Lysis centrifugation
The sediment
Instrument-based systems
Instrument-based systems
BACTEC blood culture system carbon dioxide (CO
2
)
BACTEC blood culture system
BacT/ALERT microbial detection system
ESP 80A system
100
PPT Flashcards
1583) Diagnosis of a/an what is difficult, because there are often no signs of infection at the catheter insertion site and the typical signs and symptoms of sepsis can overlap with other clinical manifestations.
1584) Various methods, such as semiquantitative cultures, Gram stains of the skin entry site, and culture of IV catheter tips following catheter removal to detect what?
1585) How may different major approaches when the catheter remains are there?
1586) Drawing two blood cultures (one from a peripheral site and one from an infected line) is an example of which approach?
1587) Comparison of the differential time to positivity of blood specimens obtained from a peripheral and intravascular site is an approach used when?
1588) Which blood culture bottles are examined daily?
1589) Hemolysis of RBCs, bubbles in medium, turbidity, small aggregates of bacterial or fungal growth in broth indicate what?
1590) If the instrument flags the specimen as positive what is done next?
1591) What stain is used on a positive specimen?
1592) What is performed on cultures suspected of being positive?
1593) Rapid tests and susceptibility testing are performed if what is suspected?
1594) Bacillus spp., Corynebacterium spp.,
Propionibacterium acnes , or coagulasenegative Staphylococcus has grown are examples of?
1595) A result is contaminated when?
1596) Clinical presentation is not consistent with sepsis then the result is from?
1597) Organism from the primary site is not the same as the organism from the blood culture is the result of a/an?
1598) When the same organism has grown in repeated cultures the result is a/an?
1599) Certain organisms from patients with suspected pathogens have grown then the result is a/an?
IV catheter–related bacteremia (or fungemia)
IV catheter–related bacteremia
2
Differential quantitative cultures when the catheter remains
Positive Blood Cultures
Growth
It is stained
Gram stain or Acridine orange stain
Subcultures monomicrobic infection
Contaminants
Multiple organisms have grown
A contaminant contaminant pathogen pathogen
101
PPT Flashcards
1600) When certain organisms (e.g., Group A streptococci [GAS]) have grown then the result is interpreted as a/an?
1601) Commensal flora is isolated from patients with suspected bacteremia the result is a/an?
1602) What is Haemophilus aphrophilus ,
Actinobacillus actinomycetemcomitans ,
Cardiobacterium hominis , Eikenella corrodens , and Kingella kingae acronym?
1603) The HACEK organisms are associated with what disease?
1604) Capnocytophaga spp., Rothia dentocariosa , Flavobacterium spp., and
Chromobacterium spp. are all examples of what kind of organisms?
1605) Campylobacter and Helicobacter grow within the how many day protocol?
1606) What is difficult to visualize without the use of acridine orange stain?
1607) Because of the fastidious nature of these organisms, appropriate media and atmospheric conditions for subculture from blood culture bottles must be employed. To facilitate the growth of which organisms?
1608) What kind of fungi can be recovered from standard media?
1609) Agitated incubation or lysis centrifugation achieves optimal isolation of what?
1610) Nontuberculous mycobacteria (NTM) tend to occur in what kind of patients?
1611) Newer methods have been developed
(e.g., automated systems) with increased sensitivity to what organism?
1612) This organism plates must be incubated at least 3 weeks and handled in a biologic safety cabinet (BSC). What is it?
1613) Brucella is incubated for how many days on an automated instrument?
1614) What organism uses direct preparations to diagnose?
1615)
What organism requires that it’s cultures are incubated for up to 13 weeks and examined using dark-field microscopy?
1616) What organisms are associated with bacteremia and endocarditis? pathogen pathogen
HACEK infective endocarditis fastidious
5-day
Campylobacter and Helicobacter
Campylobacter and Helicobacter
Yeast
Fungi
HIV positive
Mycobacteria
Brucella
7
Borrelia
Leptospira
Vitamin B6–dependent streptococci
102
PPT Flashcards
1617) What organism can be recovered during postabortal or postpartum fever?
1618) Use of the isolator system is recommended before subculture of what organism?
Chapter 69
1619) One of the diseases of the Lower
Respiratory Tract is:
1620) An inflammation of the tracheobronchial tree that may be preceded by an upper respiratory tract infection (influenza) is called:
1621) In the first 2 years of life, an acute viral infection usually occurs which is called:
1622) What are the two major categories of
Pneumonia?
1623) In the case Community-Acquired
Pneumonia, what are more common causes of bacterial pneumonia in school-age children (5 to 14 years of age)?
1624) Hospitalized children are often caused of nosocomial pneumonia by ________ .
1625) Any patient who is hospitalized is in a high risk of _________ pneumonia:
1626) One of the most likely cause of chronic lower respiratory tract infections is :
1627) What types of patients are considered at high risk for P. jiroveci; Mycobacterium tuberculosis and M. avium complex; S. pneumonia; and H. influenza?
1628) In visual examination, how much potassium hydroxide (KOH) preparation with phase contrast is needed/ used for fungi?
1629) For Gram stain, acceptable specimens yield less than _________ squamous cells per low-power field (LPF):
1630) Specimens collected from percutaneous aspiration and bronchial brush are suitable for__________:
1631) Specimens from patients with cystic fibrosis are inoculated to selective media for:
1632) Few epithelial cells and fewer than
_______ white blood cells (WBCs) indicate an excellent specimen
Mycoplasma hominis
Bartonella
Bronchitis/ Bronchiolitis/ Pneumonia/
Pleural Infections
Bronchitis
Bronchiolitis
Community-acquired; and Hospitalacquired
Mycoplasma pneumonia and Chlamydia pneumonia
Viruses
Nosocomial
Mycobacterium tuberculosis
Patients who are infected with HIV
10%
10 anaerobic culture
Staphylococcus aureus , Haemophilus influenzae , and Burkholderia cepacia
25
103
PPT Flashcards
Chapter 70
1633) Laryngitis causes hoarseness and is _____
Benign
1634) Acute laryngitis is associated with what? Viral infection
1635) ______ is an infection of the _____ and soft tissues avove the vocal cords.
Epiglottitis, epiglottis
1636) Epiglottitis affects children of what ages? 2 through 6 years of age
1637) Epiglottitis is associated with what Haemophilus influenzae type b, Streptococcus , organisms?
1638) ____ is inflammation of the salivary glands located under the cheeks. and Staphylococcus
Parotitis
1639) What is the major pathogen of parotitis? S. aureus
1640) What virus can cause parotits, but has Mumps virus declined since childhood vaccination?
1641) _____ is infection of the pharynx and causes ______
Pharyngitis sore throat
1642) The pathogenesis of pharyngitis may be due to organisms that invade the what?
1643) The organisms that cause pharyngitis may produce toxins. True or False?
1644) Viruses that tend to cause pharygitis occur when?
1645) What bacteria is a primary cause of pharyngits?
1646) Pharyngitis infection caused by S . pyogenes may lead to what?
1647) S. pyogenes has virulence factors that include
A.
M proteins
B.
streptolysin
C.
superantigen genes
D.
all of the above
1648) Pharyngitis can be caused by groups C and G streptococci and Arcanobacterium
Pharyngeal mucosa
True
During the colder months
Streptococcus pyogenes
D. all of the above
True
Poststreptoccocal sequelae haemolyticum. True or false?
1649) Streptococci in group A grow well in what media?
1650) Fusobacterium is associate with
A.
Vincent's angina
B.
Peritonsillar abscess
C.
All of the above
1651) Acute necrotizing ulcerative gingivitis is associated with _____?
1652) Peritonsillar abscess is usually a complication of _____ and is common in children older than _____
Sheep blood agar
C. all of the above
Fusobacterium
Tonsilitis, 5
104
PPT Flashcards
1653) Corynebacterium diptheriae is a _____ cause of bacterial pharyngits and it's symptoms include______?
1654) What is the hallmark sign of diptheria?
1655) _____ forms on the tonsils or pharyngeal wall and a _______ membrane results from a diptheria toxin on the epithelium.
1656) pertussis (whooping cough) symptoms include
A.
dry cough
B.
fever
C.
runny nose
D.
paroxysmal cough (after two weeks)
E.
all of the above
1657) Nasopharyngeal secretions from aspiration or washings ____ recovery and specimens are incoulated directly to culture
_______?
1658) Inflammation of the oral mucous membranes is called _____ and caused by______
1659) An infection where white patches of exudate are observed on the cheek, muosa, tongue, and oropharynx is called ___ and caused by____
1660) Root canal infections and orofacial odontogenic infections involve _____ and
_______
1661) Perimandibular space infections may involve _______ and _______
1662) Oral flora are responsible for _____
1663) Infections of the neck can spread to _____ or _____
1664) In neck infections, what organism may also be present?
Chapter 71
1665) What does the Central Nervous System consists of?
1666) What are the two coverings?
1667) What is the order of the meninges layers from outermost to innermost?
1668) What fluid is found in the subarachnoid space and surrounds the brain and spinal cord?
1669) What are the functions of cerebrospinal fluid? less common, febrile, sore throat, malaise
Pseudomembranous membrane
Exudate
Gray-white
E. all of the above improve at the patient's bedside
Stomatitis herpes symplex virus
Thrush, Candida species anaerobes streptococci staphylococci, Eikenella corrodens neck infections major vessels, mediastinum
Viridans streptococci
Brain and spinal cord
Inner (meninges) and outer (bone)
Dura mater, arachnoid, and pia mater
Cerebrospinal Fluid
Provides cushion, carries metabolites, and removes wastes
105
PPT Flashcards
1670) What is the route of infection that is followed by entry into the subarachnoid space?
1671) What is the most common route of infection?
1672) What is the route of infection that is the extension of an infection close to or contiguous with the CNS?
1673) What is the route of infection when there are anatomic defects resulting from surgery, trauma, or abnormalities?
1674) What is the least common route of infection?
1675) What is the purpose of the blood-brain barrier?
1676) How can organisms enter the blood-brain barrier?
Hematogenous spread
Hematogenous spread
Direct spread from infected site
Anatomic defects in CNS structures
Along nerves leading to the brain
Minimizes the passage of infectious agents into the CSF
Through the loss of capillary integrity of the blood-brain barrier, through the transport of circulating phagocytic cells, and by crossing the endothelial cell lining within endothelial cell vacuoles
Meningitis 1677) What disease is described as an infection in the subarachnoid space or through the leptomeninges?
1678) What are the two major categories of
Meningitis?
1679) What type of meningitis has significant, acute inflammatory exudative CSF with many polymorphonuclear (PMN) leukocytes (or neutrophils)?
1680) What type of meningitis is usually viral and characterized by an increase in lymphocytes?
1681) Why do neonates have the highest infection rate of meningitis?
1682) What are common pathogens in newborns?
1683) Before the Hib vaccine, what was the most common cause of meningitis in children?
1684) What are the symptoms of acute meningitis?
1685) What are the laboratory results of bacterial meningitis?
Purulent and aseptic
Purulent meningitis
Asceptic meningitis
Immature immune system, increased permeability of the blood-brain barrier, and presence of colonizing bacteria in the vaginal tract
Group B streptococci, Escherichia coli, and
Listeria monocytogenes
Haemophilus influenza- type b
Fever, stiff neck, change in mental status
Increased PMN leukocytes, decreased glucose in CSF, increased protein in CSF
106
PPT Flashcards
1686) When does chronic meningitis often occur?
1687) What are the typical laboratory results of chronic meningitis?
1688) What is encephalitis?
1689) What is meningoencephalitis?
1690) What are the common causes of viral encephalitis?
In patients who are immunocompromised
Increase in lymphocytes, elevated protein, and decreased glucose
An acute inflammation of the brain parenchyma (usually viral).
Concomitant meningitis with encephalitis
Enteroviruses (coxsackie and echoviruses),
Mumps,
Herpes simplex virus, Arboviruses (West
Nile, togavirus, bunyavirus)
Parasites 1691) What may cause meningoencephalitis and brain abscess via two routes?
1692) By what route are parasites acquired during swimming in natural, stagnate freshwater lakes or ponds?
1693) What is the route of infection of
Toxoplasma, Entamoeba histolytica,
1694) Strongyloides stercoralis, Taenia solium
(pork tapeworm)?
1695) How is CSF collected?
1696) What are each of the 4 CSF tubes used for?
Direct extension from the nasal mucosa
Hematogenous spread
Lumbar puncture
Tube 1- For chemistry
Tube 2- For culture
Tube 3 or 4- For cell count and differential
1697) (T or F) CSF is immediately sent to the laboratory.
1698) How should CSF specimens be stored?
True
1699) How is CSF sediment examined for cells and organisms?
1700)
1701)
How are bacterial cultures incubated?
What plates are used for fungi cultures?
1702) How are fungal cultures incubated?
1703) What is the specimen collection, transport, and processing for brain abscesses and biopsies?
Specimens for microbiology should not be refrigerated (unless viral studies are required) and should be incubated (37ºC) or left at room temperature if testing will be delayed.
Gram stain, acridine orange, wet preparation, and India ink (Cryptococcus neoformans)
At 37ºC in 5% to 10% carbon dioxide
(CO
2
) for at least 72 hours.
Sabouraud dextrose agar and brain-heart infusion with 5% sheep blood.
In air at 30ºC for 4 weeks
Specimens are homogenized in sterile saline before plating and routine bacteriologic or fungal media are used.
Chapter 72
1704) What is the external anatomy of the eye?
Eyelids, conjunctiva, sclera and cornea
1705) What is the internal anatomy of the eye? Anterior and posterior
107
PPT Flashcards
1706) What does the anterior anatomy consist of?
1707)
1708)
What does the posterior contain?
What are the normal floras of the eye?
Aqueous humor
Vitreous humor
Staphylococcus epidermidis,
Staphylococcus aureus, Lactobacillus spp.,
Propionibacterium acnes, and Haemophilus influenza
1709) How often is Haemophilus influenza encountered?
1710) How often is Staphylococcus aureus encountered?
0.4 to 25% of individuals
Less than 30% of individuals
1711) How often is Staphylococcus epidermidis encountered?
Frequently
1712) What are the rarely encountered organisms? Streptococci
1713) What are the eye’s defense mechanisms? Eyelashes and lids
1714) What prevents the entry of foreign
Moraxella catarrhalis
Eyelashes
, Enterobacteriaceae, material into the eye?
1715) What serves as a mechanism to distribute Blinking secretions that help wash away bacteria and foreign matter?
1716)
What serves as the lids’ natural defense mechanisms?
1717) What can be a pathway for infections?
1718) What can extend to periocular orbital structures?
Lysozyme and immunoglobulin A (IgA)
Bloodstreams
Sinus infections
1719) What is the inflammation of the margins of the eyelids?
1720) What causes blepharitis?
1721) What is the inflammation of the conjunctiva?
1722) What are the causes of conjunctivitis?
1723) What are the bacterial causes of conjunctivitis?
Blepharitis
Staphylococcus aureus
Conjunctivitis
Bacteria and viruses
Streptococcus pneumoniae , Haemophilus spp., S. aureus , Chlamydia trachomatis ,
Neisseria gonorrhoeae , Streptococcus
1724) What are the viral causes of conjunctivitis?
1725)
1726)
What is the inflammation of the cornea?
What are the causes of keratitis? pyogenes , and Moraxella spp.
Adenoviruses, herpes simplex virus (HSV), and varicella-zoster virus
Keratitis
Bacteria, viruses, fungi and parasites
1727) What are the bacterial causes of keratitis? Staphylococcus aureus, Streptococcus pneumoniae, Pseudomonas aeruginosa,
1728) What are the viral causes of keratitis?
Moraxella spp., and Bacillus spp.
HSV, adenoviruses, and varicella-zoster virus
108
PPT Flashcards
1729) What are the fungal causes of keratitis?
1730) What parasites cause keratitis?
1731) What is the infection of conjunctiva and cornea as a result of trauma?
1732) What are the causes of ophthalmia neonatorum?
1733) What is the inflammation of retina and underlying choroid or the uvea?
1734) What are the type of causes of chorioretinitis and uveitis?
1735) What are the bacterial agents of chorioretinitis and uveitis?
Fusarium , Aspergillus , Candida ,
Acremonium , and Curvularia
Acanthamoeba spp.
Keratoconjunctivitis
Neisseria gonorrhoeae trachomatis or Chlamydia
Chorioretinitis and uveitis
Bacterial, viral and etiological agents
1736) What are the viral agents of chorioretinitis and uveitis?
1737) What are the etiological agents of chorioretinitis and uveitis?
1738) When does endophthalmitis occur?
1739) What is the infection of the aqueous or vitreous humor?
1740) How does endophthalmitis lead to blindness?
1741) What are the etiologic origins of endophthalmitis?
1742) What are the rare, chronic inflammation of the lacrimal canals?
1743) What are the causes of lacrimal infections and canaliculitis?
1744) What is the inflammation of the lacrimal sac?
1745) What are the etiologic origins of dacryocystitis?
1746) What are the bacteria that cause dacryocystitis?
1747) What are the fungi that cause dacryocystitis?
1748) What is the acute inflammation of the lacrimal gland?
1749) What are the usual etiologic agents of dacryodenitis?
1750) How often is the normal flora of the external ear canal encountered?
Mycobacterium tuberculosis, Treponema pallidum , and Borrelia burgdorferi
Cytomegalovirus (CMV) and HSV
Candida spp., Toxoplasma gondii , and
Toxocara
—Etiologic
After surgery or trauma
Endophthalmitis
Its rapid progression
Bacterial and fungal
Lacrimal infections and canaliculitis
Actinomyces , Propionibacterium , and
Propionicum
Dacryocystitis
Bacterial and fungal
Streptococcus pneumoniae , Staphylococcus aureus , Streptococcus pyogenes , and
Haemophilus influenzae
Candida albicans and Aspergillus spp.
Dacryoadenitis
S. pneumoniae , S. aureus , or S. pyogenes
Sparsely
109
PPT Flashcards
1751) What are the encountered organisms? Pneumococci, Propionibacterium acnes ,
Staphylococcus aureus , Enterobacteriaceae,
Pseudomonas aeruginosa, Candida spp.
External ear infections 1752) What is Otitis externa ?
1753) What is Otitis media ?
1754) Where is Otitis externa found?
1755) What is the result of drainage from the middle ear in patients with chronic suppurative Otitis media or perforated eardrum?
1756) What is Otitis media?
Middle ear infections
Localized
Chronic otitis externa
Result of abnormalities of the auditory tubes
1757) What is the usual cause of chronic infections of Otitis media ?
1758) What is a complication of Otitis media ?
1759) What are the common causes of acute
Otitis externa ?
1760) What are the common causes of chronic
Otitis externa ?
1761) What are the common causes of acute
Otitis media ?
Anaerobes
Mastoiditis
S. aureus, S. pyogenes, Pseudomonas aeruginosa and other gram-negative bacilli
P. aeruginosa and anaerobes
S. pneumonia, H. influenza, Moraxella catarrhalis, S. pyogenes , respiratory synctial virus and influenza virus
Anaerobes 1762) What is the common cause of chronic
Otitis media ?
1763)
1764)
1765)
What are the sinuses?
Is the sinus sterile?
What can be found in the sinus?
1773) What may be required to treat chronic sinusitis?
1774) What are the common causes of acute sinusitis for young adults?
1775) What are the common causes of acute sinusitis for children?
Air-filled cavities in the head
Normally, yes.
Ciliary activity and mucous clear secretions and contaminants
1766) What causes sinusitis? Same pathogens associated with otitis media
1767) What are the two types of sinusitis? sinusitis?
Acute and chronic
1768) When does acute sinusitis develop? Usually during a cold or influenza illness
1769) How long is the acute sinusitis limited to? 1 to 3 weeks
1770) What are some symptoms of acute Purulent nasal and postnasal discharge and pressure over the sinus areas of the face
Bacterial colonization 1771) What does chronic sinusitis result in?
1772) Does chronic sinusitis respond to antibiotics?
No
Surgery or drainage
Haemophilus influenza S. pneumonia, S. pyogenes and Moraxella catarrhalis
Haemophilus influenza S. pneumonia,
Moraxella catarrhalis and rhinovirus
110
PPT Flashcards
Chapter 73
1776) What does the upper urinary tract consists of?
1777) What does the Lower urinary tract consists of?
1778) What are some resident microflora of the urethra?
- Kidneys and ureters
- Ureters, bladder, urethra
- Coagulase-negative staphylococci
(excluding S. saprophyticus), Viridans and nonhemolytic streptococci, Lactobacilli,
Diphteroids ( Corynebacterium spp.),
Nonpathogenic (saprobic) Neisseria spp,
Anaerobic cocci, Propionibacterium spp.
Anaerobic gram-negative bacilli,
Commensal Mycobacterium spp.,
Commensal Mycoplasma spp.
1779) What is UTI?`
1780) Which women have a higher incidence of
UTIs?
- Urinary Tract Infection
- women who are sexual active
- women who have anatomic and hormonal changes that favor the development of
UTIs.
1781) How many percent of patients with catheters will develop UTI?
1782) UTIs are caused commonly by?
- 20%
1783) What are routes of transmission?
1784) What is an Ascending route of transmission?
- Echerichia coli, Klebsiella spp., Proteus spp.,
Pseudomonas spp.
- Ascending, Hematogenous, Lympathic
- organisms multiply in the bladder and pass to the ureters and kidneys
1785) What is Hematogenous route of transmission?
1786) What is Lympathic route of transmission? - increased pressure on the bladder causes lympathic flow into the kidneys.
1787) What are physical properties that act as - normal voiding of urine (urinating), defense mechanisms preventing UTIs?
- bloodborne that usually results of bacteremia. valvelike mechanism that prevents backward flow, Urothelial cells that initiate an immune response.
1788) What are chemical properties that act as defense mechanisms preventing UTIs?
1789) What is UPEC?
- low pH, high or low osmolality, high urea content, high organic acid content.
- Uropathogenic Escherichia coli , a pathogen that possess virulence factors such as adhesins facilitate bacterial adhesion, produce alpha-hemolysin, exhibits resistance to serum-killing activity.
1790) Which pathogens possess virulence factors?
1791) Which pathogen that possess virulence factors is associated with the kidneys?
- Uropathogenic Escherichia coli, Proteus spp., S. saprophyticus.
- Proteus spp.
111
PPT Flashcards
1792)
1805)
What are some risk factors that are associated with complicated Urinary Tract
Infections?
1793) What is Urethritis?
1794) What is Ureteritis?
1795) What is Asymptomatic bacteriuria?
1796) What is cystitis?
1797) What is Pyelonephritis?
1798) What are different types of sample collecting?
1799) What screenings procedures are involved for UTIs?
1800) Which agar is used for identifying gramnegative organisms?
1801) Which agar can be used to detect grampositive enteric organisms when overgrowth occurs?
1802) Which loop is usually used to inoculate samples?
1803) What is the process of inoculating urine sample onto an agar?
1804) to make for an interpretation of Bacteriuria? acute, uncomplicated UTI in women?
1806)
How many CFUs must there be in order
What is the clinical classification of an
What are the laboratory findings of an acute, uncomplicated UTI in women?
1807) What is the clinical classification of an acute, uncomplicated pyelonephritis?
1808) What are the laboratory findings of an acute, uncomplicated pyelonephritis?
- Underlying diseases that predispose the kidney to infection (e.g., diabetes, sickle cell anemia), kidney stones, structural or functional abnormalities of the urinary tract
(e.g., a tipped bladder), indwelling urinary catheters.
- Infection of the urethra
- inflammation of the ureters
- Isolation of bacteria without signs of infection
- infection of the bladder
- inflammation of the kidney parenchyma, calices, and pelvis.
- Clean catch midstream urine, straight catheterized urine, suprapubic bladder aspiration, indwelling catheter collection.
- gram stain, pyuria (>400,000 PMNs per hour), Nitrate reductase, Leukocyte esterase, catalase.
- MacConkey agar
- Columbia colistin-nalidixic acid (CNA) or phenylethyl alcohol (PEA) agar
- .01 or .001- mL loop
- Urine is thoroughly mixed before inoculation, loop is touched to the center of the plate , then it is streaked with calibrated loop, plates are incubated for 24 hours for
35 degrees C.
- 10 5 CFUs/mL
- Dysuria, urgency, frequency, suprapubic pain, no urinary symptoms in last 4 weeks before current episode, no fever or flank pain.
- greater than or equal to 10 WBC/mm
3
, greater than or equal to 10
3
CFU/mL uropathogens in CCMS urine.
- Fever, chills, flank pain on examination, other diagnoses excluded, no history or clinical evidence of urologic abnormalities.
- greater than or equal to 10 WBC/mm
3
, greater than or equal to 10 4 CFU/mL uropathogens in CCMS urine.
112
PPT Flashcards
1809) complicated UTI and UTI in men?
1810)
What is the clinical classification of a
What are the laboratory findings of a complicated UTI and UTI in men?
- any combination of symptoms listed above, one or more factors associated with complicated UTI
- greater than or equal to 10 WBC/mm 3 , greater than or equal to 10
5
CFU/mL uropathogens in CCMS urine.
- No urinary symptoms 1811) What is the clinical classification of an asymptomatic bacteriuria?
1812) asymptomatic bacteriuria?
1813)
What are the laboratory findings of an
What are some characteristics of uncomplicated UTI?
1814) What are some characteristics of complicated UTIs:
Chapter 74
1815) Referring to normal flora, what kind of organism are located in the urethral flora?
1816) Normal flora consists of what organisms in the vulva and penis?
1817) In regards to normal flora, pH and estrogen in female tract can varies. EXCEPT?
Lactobacilli are predominant.
Prepubescent and postmenopausal women harbor staphylococci and corynebacteria.
Women of reproductive age harbor facultative bacteria and anaerobes.
Some women carry group B streptococci, which can be transmitted to the neonate.
Thick and cheesy discharge
1818) STDs are the major cause of genital tract infection? True or False
1819) Herpes simplex, Haemophilus ducreyi,
Treponema pallidum can infect the____
____?
1820) What sexual habits dictate the site of infection?
1821) Chlamydia trachomatis, Neisseria gonorrhoeae, Trichomonas vaginalis , Human immunodeficiency virus (HIV), Ureaplasma urealyticum,
Mycoplasma hominis, Adenovirus,
Coxsackievirus, Molluscum contagiosum,
Human papillomaviruses (HPVs) are ______
______?
- plus or minus greater 10 WBC/mm
3
, greater than or equal to 10 5 CFU/mL in two
CCMS cultures > 24 hours apart.
- occur in both healthy women and men, respond well to antibiotics
- occur in both sexes, individual often have certain risk factors, are more difficult to treat, have greater morbidity and mortality
Coagulase-negative staphylococci
Corynebacteria
Anaerobes
Mycobacterium smegmatis
Gram-positive bacteria
E. Thick and cheesy discharge
True
Surface epithellium
Anal genital, Oral genital
STD agents
113
PPT Flashcards
1822) None sexual routes can be associated with?
A.
Instruments
B.
Foreign body
C.
Irritation
D.
Mother to infant (in vivo or during delivery)
E.
All the above
1823) Referring to Dysuria, what is the clinical manifestation?
1824) Urethral discharge can indicate what
_____infection? (Urethritis)
1825) Lesion of skin and mucous membranes can cause?
1826) Vaginitis is inflammation of the vaginal mucosa. True or False?
1827) Cervicitis is inflammation of the vaginal?
True or False?
1828) Proctitis is caused by anorectic lesions?
True or False?
1829) Bartholin gland infection is caused by bartholinitis? Trur or False
1830) Vaginitis symptoms are?
A.
Itching
B.
Offensive odor
C.
Abnormal discharge
D.
All the above
1831) Thick and cheesy discharge is what causative agents?
A.
Trichomonas vaginalis
B.
Gardnerella vaginalis
C.
Candida albicans
D.
All the above
1832) Slightly offensive, yellow-green discharge?
A.
Trichomonas vaginalis
B.
Gardnerella vaginalis
C.
Candida albicans
D.
All the above
1833) Bacterial vaginosis, Polymicrobic, possibly the result of the loss of lactobacilli?
A.
Trichomonas vaginalis
B.
Gardnerella vaginalis
C.
Candida albicans
D.
All the above
1834) Increased polymorphonuclear neutrophils
(PMNs) in the endocervix, Purulent discharge are symptoms of Cervicitis? True of False
E. All the above
Painful urination gonococcal
Genital warts, Neoplasia (e.g., tumor)
True
False
Cervix
True
True
D. All the above
C. Candida albicans
E. Trichomonas vaginalis
B. Gardnerella vaginalis
True
114
PPT Flashcards
1835) Referring to cervicitis, causative agents are?
A.
Neisseria gonorrhoeae
B.
Chlamydia trachomatis
C.
Herpes simplex virus (HSV) Friable cervix (bleeds easily)
D.
HPV
E.
All the above
1836) Cervical microorganisms travel to the endometrium, fallopian tubes, and other pelvic structures.
A.
Dysuria
B.
Anorectic
C.
PID
D.
All the above
1837) PID may produce endometritis, salpingitis, peritonitis, or abscesses. True or
False?
1838) Scarring of fallopian tubes or infertility may occur if left untreated because ____?
1839) Referring to women tract infections,
Common agents include Neisseria gonorrhoeae, Chlamydia trachomatis, anaerobes, gram-negative rods, streptococci, and mycoplasmas.
True of False?
1840) Upper tract infections for women are more susceptible in gynecologic surgery.
True or False?
1841) Prenatal, Postpartum infection are associated with _____?
1842) Epididymitis is associated with inflammation epididymis and sexually active men. True or False?
1843) Adult male patients who have perineal, lower back, or lower abdominal pain, urinary discomfort, or ejaculatory complaints are associated with ____?
1844) Inflammation of the testicles, Uncommon and acquired by bloodborne dissemination of viruses are associated with ______?
1845) Neisseria gonorrhoeae cause______?
1846) _____ is spread by direct contact in the mouth, vagina, penis, or perianal region?
E. All the above
C. PID
True
PID
True
True
Pregnancy
True
Prostatitis
Orchitis
Gonorrhea
Gonorrhea
115
PPT Flashcards
1847) Symptoms occur 2 to 5 days after infection in men and up to 1 month in men.
True or False?
1848) Gonorrhea diagnosis
A.
Intracellular gram-negative diplococcus is observed in secretions
Intracellular gram-negative diplococcus is observed in secretions.
B.
Definitive diagnosis requires culture.
C.
Extracellular gram-negative diplococci in women are normal flora.
D.
All the above
1849) Referring to specimen collection,
Urogenital swabs are true. EXCEPT?
A.
One swab is placed in sterile saline (for
Trichomonas vaginalis).
B.
Separate swabs are required for gonococci, chlamydiae, and ureaplasma.
C.
Specimens for group B streptococci are inoculated to selective broth and then subcultured to agar the next day.
1850) In regards to sexual abuse cases, extreme care is taken for specimen collection. True or
False?
1851) Swabs from the Bartholin gland exudate are not recommended; aspiration with a syringe is suggested. True or False?
1852) What organism is used for this culture:
MTM medium, NYC medium, JEMBEC plates?
A.
gonococci
B.
streptococci
C.
Trichomonas vaginalis
D.
None
1853) What organism is used for this culture:
Both grow on standard blood agar, Yeast grow well on Columbia agar with 5% sheep blood and Columbia CNA.
A.
gonococci
B.
Trichomonas vaginalis
C.
streptococci
D.
A and B
False
2 to 5 days for women
Up to 1 month for men
D. All the above
C. Specimens for group B streptococci are inoculated to selective broth and then subcultured to agar the next day.
True
True
A. gonococci
C. streptococci
116
PPT Flashcards
1854) Specimens for group B ________ are inoculated to selective broth and then subcultured to agar the next day.
A.
Trichomonas vaginalis
B.
streptococci
C.
gonococci
D.
None
1855) _________ may be cultured in Diamond’s medium or plastic envelopes inoculated with discharge material.
A.
gonococci
B.
streptococci
C.
Trichomonas vaginalis
D.
Cocci
1856) Referring to nonculture method, these tests are true. EXCEPT?
Serologic examination
A.
Latex agglutination
B.
Nucleic acid hybridization and amplification assays
B. streptococci
C. Trichomonas vaginalis
E. Organism separation assay
C.
Enzyme immunoassays
D.
Organism separation assay
1857) PH measurement and sialidase test
(Genzyme Diagnostics) are associated with
True bacterial vaginosis diagnosis?
True or False?
1858)
Chapter 75
Describe the numbers of resident flora in the
GI tract?
1859)
What's the ratio of anaerobes to aerobes in
The upper small intestine contains 10 to
10 2 /mL sparse flora, the distal ileum counts are higher (10 6 to 10 7 /mL.
1000 to 1. the adult large bowel?
1860)
Which flora are found in the distal ileum? Enterics, Bacteroides spp.
1861) Which flora are found in the adult large bowel?
1862) What are the 2 nd leading cause of death?
Clostridium, Enterococci, Streptococci
Diarrheal diseases
1863)
What are the host factors of
Gastroenteritis?
Acidity of stomach, normal peristalsis, mucous layer coating the epithelium, normal flora preventing colonization by potential pathogens
1864) What are the microbial factors of gastroenteritis?
1865)
What are examples of microorganisms that cause GI infection for enterotoxin production?
Primary pathogenic mechanisms, toxins: enterotoxins, cytotoxins, and neurotoxins, attachment mechanisms, invasion of the host's intracellular environment
Vibrio cholera, Shigella dysenteriae type 1,
Salmonella spp, aeromonas
117
PPT Flashcards
1866) cytotoxin production?
1867) production?
1868) within or close to mucosal cells/adherence?
1869)
1870)
What are some microorganisms for
What are microorganisms for neurotoxin
What are microorganisms for attachment
What are microorganisms for invasion?
What are the types of Enteric infections by pathogenic mechanism?
Shigella spp, Clostridium difficile (toxin
B), enterohemorrhagic E. Coli
Clostridium botulinum, Staphylococcus aureus, Bacillus cereus
Rotavirus, Hepatitis A, B, C, Norwalk virus, Isospora belli
Enteroinvasive E. coli, Campylobacter jejuni, Shigella spp.
Upsetting of fluid & electrolyte balance/noninflammatory, invasion & possible cytotoxin production/inflammatory
(dysentery), penetration with subsequent access to the bloodstream (enteric fever)
1871)
What are the major symptoms of fluid upset and electrolyte balance?
1872)
What are examples of etiologic agents of fluid upset and electrolyte balance?
1873)
What are the symptoms of invasion & cytotoxin production?
1874)
What are etiologic agents of invasion & cytotoxin production?
1875)
What are symptoms of penetration with access to the bloodstream?
1876) What are etiologic agents of enteric fever? Salmonella typhi, Yersinia enterocolitica
1877)
Which microorganisms in pathogenic Bacillus cereus, Aeromonas, Vibrio bacterial infections that cause watery diarrhea?
Cholerae, Enteropathogenic E. Coli
1878)
Which microorganisms cause bloody diarrhea (dysentery)?
1879)
What are the bacterial agents that cause food poisoning?
Shigella spp, Salmonella spp,
Enteroinvasive E. Coli, Aeromonas
Staphylococcus Aureus, Bacillus Cereus,
Type A Clostridium perfringens,
Clostridium botulinu
1880)
What are the non bacterial agents of infection?
Watery diarrhea, no fecal leukocytes, no fever
Vibrio cholerae, rotavirus, norwalk virus,
Bacillus cereus
Dysenteric like diarrhea (mucus, blood, white cells) fever, fecal leukocytes
Shigella spp, Enteroinvasive E. coli,
Salmonella enteritidis
Signs of systemic infection: headache, malaise, sore throat, fever
1881)
1882)
1883)
What are the clinical manifestations of watery diarrhea?
What are the clinical manifestations of dysentery?
What are the clinical manifestations of disseminated infections?
1884)
Where are etiologic agents found?
Giardia lamblia, Cryptosporidium parvum,
Entamoeba histolytica, rotavirus, norwalk virus
Fluid and electrolyte balance is upset, no fecal leukocytes are present
Cell destruction and inflammation occur, fecal leukocytes are present, mucus and blood are present
Spreads to other sites
Institutional settings, day care centers
(viruses, Shigella spp, Campylobacter jejuni), hospitals (Clostridium difificile), nursing homes
118
PPT Flashcards
1885)
Where is traveler's diarrhea found? Developing countries, enterotoxigenic E.
Coli (Asia, Africa and Latin America)
1886)
Describe food and water borne outbreaks Usually traced to poor hygienic practices of food handlers, Hepatitis A, Norwalk virus and Salmonella
1887)
What is Esophagitis?
1888)
1889)
1890)
What is Gastritis?
What is Proctitis?
What is the lab diagnosis?
Painful, difficulty in swallowing, most patients have underlying illnesses (HIV), most common agents are Candida spp, herpes simplex virus (HSV) & cytomegalovirus (CMV)
Inflammation of the gastric mucosa is present, is often associated with
Helicobacter pylori
Inflammation of the rectum, most infections are sexually transmitted
Direct wet mount, clostridium difficile toxin assay, immunoelectron microscopy for viruses, enzyme linked immunosorbent assay (ELISA) or latex test for rotavirus
1891)
What are the stains used in direct detection?
1892)
How are antigens detected?
Gram stain will detect Campylobacter & polymorphonuclear(PMN) leukocytes, Acid fast stain is used for Cryptosporidium & mycobacteria. Trichrome stain for parasites
Indirect fluorescent stain for giardiasis and cryptosporidiosis, enzyme immunoassay(EIA) or latex test for E. Coli, shiga toxins & Clostridium difficile toxins
A or A and B.
1893) Which types of agar are used in routine culture?
1894) What's the diagnosis of Campylobacter difficile diarrhea?
Blood agar supports the growth of most yeasts & bacteria. MacConkey agar: enterics & vibrios growth, MacConkey with sorbitol for E. Coli, Campy agar selective for C.coli & C.jejuni.
Based on clinical criteria combined with lab testing: culture, detection of cytotoxin by tissue culture, antigen detection assays for
C. difficile toxin
Chapter 76
1895) What is the role of skin?
Skin forms a protective boundary between the body’s internal environment and the external environment
1896) How does skin help to prevent colonization by pathogenic bacteria?
1897) Name some resident microbial flora on the skin
Normal microbial flora, pH, Chemical defense
Diphtheroids, Staphylococcus epidermidis,
Propionibacterium acnes, other coagulase negative staphylococci
119
PPT Flashcards
1898)
1899)
1900)
1901)
1902)
1903)
1904)
1905)
1906)
What is Macule?
What agents cause macule?
What is papule?
What agents cause papule?
What is nodule?
What agents cause nodule?
What is pustule?
What agents cause pustule?
What is vesicule?
Flat discoloration of the skin
Dermatophytes, Treponema pallidum , and enteroviruses
Elevated, solid lesions (less than 5 mm in diameter)
Human papillomavirus (HPV), pox virus, scabies,
Staphylococcus aureus , and Pseudomonas aeruginosa
Raised, solid lesion (greater than 5 mm in diameter)
Corynebacterium diphtheriae , Sporothrix schenckii , fungi, Mycobacterium marinum , and Nocardia
Raised, pus-filled lesion containing leukocytes and fluid
Candida spp., dermatophytes, herpes simplex virus (HSV), Neisseria gonorrhoeae , S. aureus , Group A streptococci, and varicella-zoster virus.
Raised, fluid-filled (blisterlike) lesions (less than 5 mm in diameter)
Varicella-zoster virus 1907) What agent causes vesicule?
1908) What is Bulla? Raised, fluid-filled lesion (greater than 5 mm in diameter)
1909) What agents cause Bulla?
1910) What are scales?
1911) What agents cause scales?
1912) What is an ulcer?
Clostridium spp., HSV, gram-negative rods,
S. aureus , and vibrios
Dry, horny, and platelike lesions
Dermatophytes
Lesion with the loss of epidermis and dermis
1913)
1914)
1920)
What agents cause an ulcer?
What is folliculitis?
What etiological agents cause cellulitis?
Bacillus anthracis , bowel flora, Haemophilus ducreyi , and Treponema pallidum
Papules or pustules that are pierced by a hair and surrounded with redness
1915) What is furuncle? Abscess that begins as a red nodule in a hair follicle that ultimately becomes painful
1916) What is carbuncle? and full of pus
Furuncles that coalesce and spread more deeply to the dermis and subcutaneous tissues
1917) What is erysipelas? Painful, red, and swollen indurated lesions
1918) What etiological agents cause erysipelas? Group A, B, C or sometimes G streptococci
1919) What is cellulitis? Diffuse spreading infection involving deep layers of the dermis
Group A streptococci, Staphylococcus aureus
120
PPT Flashcards
1921) What is erythrasma?
1922) What agent causes erythrasma?
1923) What is erysipeloid?
1924) What agent causes erysipeloid?
1925) What is impetigo?
1926) What agents cause impetigo?
1927) What is dermatophytosis?
1928) What is necrotizing fasciitis?
1929) What agent causes necrotizing fasciitis?
1930) What is Progressive bacterial synergistic gangrene?
1931) What agents cause progressive bacterial synergistic gangrene?
1932) What is myositis?
1933) What agent causes myositis?
1934) What agent most commonly causes postoperative infections?
1935) What infectious agents are most commonly involved in animal bites?
1936) What are the four types of burns?
1937) What agents are commonly associated with burns?
1938) What is a sinus-tract infection?
1939) What agents are usually involved in a sinus-tract infection?
1940) What agents are involved with actinomycosis?
1941) Where is anaerobic cellulitis often identified?
1942) What vascular and neurologic problems are often seen in anaerobic cellulitis?
Chronic infection of the keratinized layer of the epidermis
Corynebacterium minutissimum
Purplish, nonvesiculated skin lesion with an irregular, raised border
Erysipelothrix rhusiopathiae
Erythematous lesion that may be bullous or nonbullous
Group A streptococci (nonbullous) and
Staphylococcus aureus (bullous)
Fungal infection of the skin
Muscle fascia and soft tissues become infected.
Large areas of the body may become infected in a short amount of time group A streptococci or Staphylococcus aureus
Chronic necrotic condition of the skin is a result of surgery usually polymicrobic with microaerophilic streptococci and S. aureus . inflammation of the muscle
Staphylococcus aureus
Staphylococcus aureus
Pasteurella and Fusobacterium impetigo, surgical, cellulitis, and invasive
S. aureus , Pseudomonas aeruginosa , enterococci, Enterobacter spp., and
Escherichia coli a deep-seated inflammation that develops a channel to the skin surface
Staphylococcus aureus , Enteric pathogens
Pseudomonas aeruginosa, Anaerobic gramnegative bacilli, and anaerobic grampositive cocci
Actinomyces spp., Actinobacillus, actinomycetemcomitans ,
Propionibacterium propionicum , Prevotella spp., Porphyromonas spp.
In the extremities
Impaired circulation, peripheral motor neurophathy
121
PPT Flashcards
1943) What agents are associated with diabetic foot infections?
1944) What type of culture should be performed on bullous lesions?
1945) What type of transport media is required for bite wound infections?
Chapter 77
1946) What are the five main body cavities?
1947) What is found between the membranes and organs to reduce friction?
1948) What fluid lubricates the pleura?
Staphylococcus aureus , Group B streptococci, Enteric pathogens, Anaerobes
Blood culture
Anaerobic transport media
Cranial, spinal, thoracic, abdominal, pelvic
Sterile fluid
Pleural fluid
1949) What is the condition in which excess fluid is produced around the pleura?
1950) When inflammation of the peritoneum occurs, what is often contained in the ascetic fluid?
Pleural effusion inflammatory cells and elevated protein
1951) What condition is attributed to most cases of peritonitis?
1952) How is peritonitis diagnosed?
Liver disease
Cloudy dialysate, abdominal pain, positive blood culture from dialysate
1953) What are the usual agents of pericarditis? viruses
1954) What fluid does the diagnosis of septic arthritis require to be aspirated for
Synovial fluid examination?
1955) How are most fluid specimens collected? By aspiration
1956) What may be necessary to diagnose Bone marrow aspiration or biopsy brucellosis, histoplasmosis, blastomycosis, tuberculosis, and leishmaniasis
1957) What is often collected when osteomyelitis is suspected
1958) What is is the most common organism associated with osteomyelitis.
1959) From where is bone marrow aspirated?
1960) What may be necessary to examine bone biopsies?
1961) What kind of specimen may need mincing before culturing
Bone biopsy
Staphylococcus aureus from the interstitium of the iliac crest
Grinding the bone with mortar and pestle
Solid tissue
Chapter 78
1962) An activity designed to improve patient care by having the laboratory monitor work to detect and correct deficiencies is…
1963) What is Continuous quality improvement
(CQI) and performance improvement (PI) for?
Total quality management (TQM)
To place the emphasis on preventing mistakes.
122
PPT Flashcards
1964) What quality control method is associated with the internal activities that ensure diagnostic test accuracy?
1965) What methodology does concentrate on eliminating redundant motion, recognizing waste, and identifying what creates value from the clients’ perspective?
1966) What does help reduce operational costs by focusing on defect reduction, turnaround time, and cost savings?
1967) What testing phases are important for each laboratory to maintain policies and procedures for QC?
1968) Who is responsible for the QC and QA programs?
1969) What private certifying agencies do supersede federal guidelines?
1970) What criterias are important in written instruction for specimen collection?
1971) What agency the Standard Operating
Procedure Manual should be written by?
1972) What are elements of QC Program?
Quality assurance (QA)
LEAN methodology
Six Sigma
Preanalytic, Analytic, Postanalytic.
The laboratory director
College of American Pathologists (CAP) and The Joint Commission (TJC)
Patient selection, appropriate transportation, and storage.
Clinical and Laboratory Standards Institute
(CLSI)
Personnel, Reference Laboratory, Patient reports
1973) How often should personnel be qualified? Twice during the first year and annually thereafter
1974) What must be done in case of getting critical value?
Clinician should be notified immediately
1975) What is a Quality assurance (QA) measure that monitors a laboratory’s analytical performance in comparison with
Proficiency Testing (PT) peers and reference standards?
1976) How do Private accrediting agencies provide PT?
1977) Some important following information that should be contain equipment logs are…
They send out “blind unknowns” that are to be treated exactly the same as a patient specimen.
Procedure and periodicity of function tests
Acceptable performance ranges
Corrective action when problems occur
Genetic Stability 1978) What is the reason to select Minimum inhibitory concentration (MIC) reference strains?
1979) How long each antimicrobial susceptibility test system should be tested?
1980) What kits should be appropriately labeled
(e.g., opened date, expiration date) and tested with controls?
For 20 days
Stains, reagents, and antisera
123
PPT Flashcards
1981) What is the appropriate way to save nonfastidious organisms?
1982) What is the appropriate way to save molds?
1983) What is the appropriate way to keep
AFB?
1984) What is the appropriate way to store viruses?
1985) Collection of specimen by the health care provider would refer to which step in the quality assurance process?
1986) Interpretation of specimen results by the microbiologist would refer to which step in the quality assurance process?
1987) Formulation of a written or printed report by the microbiologist would refer to which step in the quality assurance process?
1988) What type of audit compares data from one laboratory with data from other facilities of similar size?
1989) What is the goal of daily monitoring?
Chapter 79
1990) An infection, which was not present or in the prodromal stage when a patient entered the health care setting, is contracted after admission
1991) An infection is contracted outside of a health care setting
1992) Infection present on admission(to hospital)
1993) The majority of______ involve the patient’s own flora
1994) Susceptibility of the patient to the infection, Virulence of the infecting organism, Nature of the patient’s exposure to the infecting organism
1995) UTI(35%), Pneumonia(15%), surgical site infections(15%), bloodstream infections(13%) are all types of:
1996) Prolonged hospitalization and prior treatment with antibiotic are risk factors for the acquisition of
1997) The use of ____________has played a role in the emergence of many antibiotic-resistant organisms.
Save for 1 year on trypticase soy agar (TSA) slants.
Are stored on phenylalanine deaminase
(PDA) slants at 4ºC for 1 year
Keep on Löwenstein-Jenson agar at 4ºC for
1 year
Store indefinitely at –70ºC in a cryoprotectant substance.
Preanalytic
Analytic
Postanalytic
Q-Probes program
Patients get the best quality care. health care–associated infections (HAIs)
Community-acquired infections
Community-acquired infections health care–associated infections (HAIs) factors that determine whether a patient will acquire an infection are: health care–associated infections (HAIs)
Resistant organisms cephalosporin antibiotics
124
PPT Flashcards
1998) Patients colonized ________ can transfer organisms to other patients in nursing homes and in the community
1999) Microbiologist, infection control practitioner, hospital epidemiologists, and pharmacist all serve on an:
2000) Collecting and analyzing surveillance data, Monitoring patient care practices,
Participating in epidemiologic investigations,
Educating health care providers in techniques that minimize the spread of infections are the responsibilities of: antibiotic-resistant organisms
Infection control committee infection control practitioner
2001) Direct, indirect, droplet, airborne, vectorborne
2002) The lab: saves all isolates, cultures possible reservoirs, typing strains to establish relatedness among isolates of same species.
Modes of transmission
During a suspected out break
2003) Labs are required by law to report certain Isolates or syndromes to public health officials
2004) biotyping, antibiograms, serotyping
2005) Two major ways to type strains
2006) These two methods occur in:
2007) Plasmid analysis is often used to explain
Phenotyping techniques
Phenotyping techniques, genotypic methods
Genotypic methods the occurrence of unusual or multidrugresistance patterns, Restriction endonuclease technique has been modified to reduce the number of bands to ensure that the gels are easy to interpret.
2008) Washing hands, segregating, PPE, bagging contaminated articles, cleaning isolation rooms, place cards on patient doors with type of isolation and instructions for visitors are all:
2009) Microbiologist, infection control practitioner, and hospital epidemiologist can make the decision to __________
2010) Certain surveillance cultures are still performed as a method of
2011) Cooling towers, hot water sources(for
Legionella spp .), water, dialysis fluids, blood bank products, VRE, MRSA, VRSA are all
_____&_______ to help limit outbreak
Techniques for isolation precautions
Perform cultures
Limiting outbreaks
Cultured and checked
Chapter 80
2012) What is biocrime?
A biocrime, or bioterrorism event, is an intentional assault on a person or group of people using a pathogen or toxin. Assaults are either overt or covert.
125
2013) What are select agents?
2014) What does a laboratory biosecurity plan entail?
2015) What is the LRN?
PPT Flashcards
2016) What does a Sentinel Laboratory need to detect and recognize a possible bioterrorism event?
Select agents are specific pathogens or toxins that pose a risk to public health and national security.
Select agents are defined by the United
States Department of Health and Human
Services (DHHS) and the United States
Department of Agriculture (USDA).
Category A—Present the highest risk to the public
Category B—Agents that are moderately easy to disseminate
Category C—Emerging pathogens that could be engineered for mass spreading
The plan must include physical security and data system security policies as well written procedures for Assessing select agents
Specimen accountability
Receipt of select agents in the laboratory
Transfer and shipping of select agents from the laboratory
Reporting incidents
Emergency response plan
The Laboratory Response Network is a three-tier system:
Sentinel laboratories
Recognize, rule out, and refer.
Reference laboratories
Perform confirmation testing.
National laboratories
Definitively characterize agents.
A laboratory must have an active microbial surveillance program, rule out possible bioterrorism agents, vigilant technologists looking for a disease that does not occur naturally in a particular geographic region, transmitted by an aerosol route of infection, caused by an unusual agent, good communication with infection control practitioners, infectious disease physicians, and local and regional public health laboratories 24 hours a day.
126
PPT Flashcards
2017) What government agencies are responsible for managing bioterrorism and consequence management?
Federal Bureau of Investigation (FBI)
Federal Emergency Management Agency (FEMA)
FEMA receives assistance from the following agencies:
Department of Defense (DOD)
Department of Energy (DOE)
USDA
Department of Transportation (DOT)
DHHS
Environmental Protection Agency (EPA)
127