Smooth Muscle Drugs
advertisement

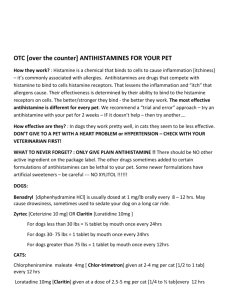
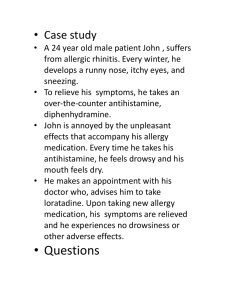
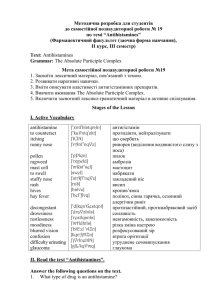
1 Pharmacotherapeutics for Advanced Nursing Practice 433 Drugs that Act on Smooth Muscles: Antihistamines, Decongestants, and Bronchodilators Allergic rhinitis and asthma will be the prototypical disease states used to introduce these agents. Allergic Rhinitis Pathophysiology Sympathetic stimulation causes vasoconstriction, resulting in reduction of tissue size and airway widening. Parasympathetic stimulation causes vasodilation and airway narrowing. The nasal mucosa contains mast cells. o Mast cells release histamine which increases epithelial permeability. o This allows allergens to reach the submucosa where there is a high density of mast cells o Once a patient is susceptible, allergens react with IgE on these mast cells. o The release of cytokines from these cells produces local inflammation. Signs/symptoms commonly seen include: rhinorrhea, sneezing, itching in the nose and throat, watery eyes Complications (most common) Exacerbations of asthma Acute and chronic sinusitis Treatment Antihistamines and decongestants work to alleviate symptoms. Nasal steroids and nasal cromolyn are also very helpful in reducing symptoms in chronic patients. Leukotriene inhibitors used for asthma have also been found to be of benefit for allergy symptoms. Antihistamines Note: There are two types of histamine blockers (“antihistamines”): histamine1) H1 blockers are used for treatment of seasonal allergic rhinitis, anaphylaxis, and insect reactions, whereas histamine2 (H2) blockers are used in the treatment of gastric acid disorders such as ulcers. The following discussion relates to histamine1 blockers. 2 Mechanism of action: antagonize the histamine receptor, preventing the action of histamine. o All antihistamines work best when given before allergen exposure. Oral antihistamines are systemic; use especially if the person is experiencing eye symptoms of allergy along with the nasal symptoms. The use of antihistamines in allergic rhinitis is effective, but side effects and cost can limit their use. o All are equally effective. o Size effects determine the choice of agent. Effects of Various Antihistamines Generic Name brompheniramine Brand Name Anticholinergic Effects* Moderate Sedative Effects Low Moderate High High Low Moderate Low to Moderate Low to Moderate chlorpheniramine clemastine diphenhydramine Dimetane, Codimal-A Chlor-Trimeton Tavist Benadryl dimenhydrinate Dramamine High promethazine hydroxyzine Phenergan Atarax, Vistaril High Moderate High Moderate loratadine desloratadine cetirizine fexofenadine Claritin (OTC) Clarinex Zyrtec (OTC) Allegra (OTC) Low to none Low to none Low to none Low to none Low to none Low to none Low to none Low to none * Comments Cause less drowsiness and more CNS stimulation; suitable for daytime use Substantial anticholinergic effects; commonly cause sedation; with usual doses drowsiness occurs in ~ 50% of patients; diphenhydramine and dimenhydrinate also used as antiemetics; dimenhydrinate also used as antivertigo Also used as antiemetic, antivertigo Also used as a tranquilizer, sedative, antipruritic, and antiemetic Very few adverse effects from anticholinergic or sedative effects; almost exclusively antihistaminic effects; can take during day because no sedative effects. In general they are longer activing and have fewer side effects If anticholinergic effects are “high”, high risk of urinary retention, paradoxical excitation. Antihistamines with “high” anticholinergic effects should be used with caution in patients with angle-closure glaucoma and prostatic hypertrophy……why? The sedating agents are less expensive and generally safe, thus it may be worth beginning therapy with these agents. Caution with elderly and others at risk for falls! With sedating agents such as chlorpheniramine (Chlor-Trimeton), begin with 1 mg twice a day (short-acting) and work up over 2-6 weeks to full dose (8-12 mg/day) to prevent dose limiting side effects such as sedation in patients with significant allergy. 3 Antihistamines: Drug Effects Cardiovascular system (small blood vessels) o Histamine effects: Dilation of blood vessels, increased blood vessel permeability (allows substances to leak into tissues) o Antihistamine effects: Prevent dilation of blood vessels and increased permeability Smooth muscle (on exocrine glands) o Histamine effects: Stimulates salivary, gastric, lacrimal, and bronchial secretions o Antihistamine effects: Prevents salivary, gastric, lacrimal, and bronchial secretions Immune system (release of various substances commonly associated with allergic reactions) o Histamine effects: Mast cells release histamine and several other substances, resulting in allergic reactions o Antihistamine effects: Do not stabilize mast cells nor do they prevent the release of the substances such as histamine, but they bind to histamine receptors and prevent the actions of histamine. Drug Interactions Problem with the early non-sedating antihistamines (terfenadine [Seldane] and astemizole [Hismanal]): Metabolized by the liver Erythromycin, ketoconazole (Nizoral), itraconazole (Sporanox) could inhibit their metabolism. In some patients, this could result in toxic concentrations of terfenadine and astemizole, resulting in arrhythmias from prolongation of the QT interval. These medications were removed from the market. So, what pharmacokinetic process was the basis for the potentially fatal drug interaction described above? Decongestants Decongestants are useful for immediate relief of symptoms while waiting for onset of action of antihistamines and anti-inflammatories. Local vasoconstriction – topical Examples: oxymetazoline (Afrin, Dristan, Sinex) and phenylephrine (Neosynephrine) Duration of therapy: use only when needed for no longer than 3-5 days. 4 o With prolonged therapy, “rhinitis medicamentosa” occurs in virtually all patients. o More of the drug is required to produce the same effects. o Once the drug is stopped, there is rebound congestion (rebound vasodilation) following the extreme vasoconstriction. Patients will want to use the drug again to treat this. o Treatment involves a 2-3 week wean of the topical agent while combining a nasal anti-inflammatory agent such as cromolyn. Systemic vasoconstriction – oral phenylpropanolamine [PPA] (as in Allerest, Contac, Rhinedecon, and Dexatrim): pulled from market in 2000 due to risk of hemorrhagic stroke, particularly in women. pseudoephedrine (as in Pediacare, Sudafed): Still available. o OK for use with hypertensive patients IF HTN is well-controlled, it is used for only a short time, and the dosage used is the 30 mg, rather than 60 mg. o Effective January 15, 2006, the Methamphetamine Precursor Control Act (MPCA) makes pseudoephedrine and ephedrine “schedule V controlled substances,” meaning they must be kept behind pharmacy counters. It requires that all medications that contain any amount of pseudoephedrine or ephedrine in any form be kept behind the pharmacy counter. Customers who want to purchase these products do not need a prescription but they do need to show a governmentissued identification card, be at least 18 years of age, and sign a log. Customers purchasing medications containing pseudoephedrine or ephedrine can purchase no more than two packages, or 6000 milligrams, at a time and no more than 7500 milligrams in a month. (http://www.illinoisattorneygeneral.gov/methnet/news/edition2/story3.html) Phenylephrine (Neosynephrine, Sudafed on the shelf): Avoid in HTN patients o Systemic phenylephrine is an alpha1 agonist…..why would this be a problem in patients with HTN? For those with uncontrolled HTN, there is Coricidin HBP, which does not contain a decongestant….does contains chlorpheniramine (antihistamine) o Can you think of any other option for patients with HTN? Combination decongestant/antihistamine therapy – indications o Useful in patients but usually for a short duration o In most viral URIs patients do not require an antihistamine; therefore combination products are generally not recommended after gaining initial control of symptoms o Works well with patients who have congestion along with an underlying allergy problem o Examples: Claritin-D, Allegra-D, Zyrtec-D) 5 Intranasal Anti-Inflammatories (Steroids) o Examples o cromolyn sodium (Nasalcrom) 1 spray 3-4X/day o beclomethasone (Beconase AQ) 1-2 sprays 2X/day o budesonide (Rhinocort Aqua) 1 spray/day (up to 4 sprays/day) o fluticasone (Flonase, Veramyst) 2 sprays/day (can decrease to 1/day)* Flonase Allergy Relief available OTC in spring 2015) o mometasone (Nasonex) 2 sprays/day (can decrease to 1/day)* o triamcinolone (Nasacort AQ) 2 sprays/day (can decrease to 1/day)* * With control of symptoms, can decrease to 1 spray/day. o Good if patient’s only allergy symptoms are nasal o All of these agents may be more effective than antihistamines for long term control of allergic rhinitis. o They need to be used once the patient is decongested and with clear nasal passages o The steroids work by stabilizing the epithelial mediator cells and decreasing epithelial permeability. o Cromolyn works by stabilizing the mast cells. o They have little additive effect when used in combination with antihistamines o Their onset is within a few days to 2 weeks. o During this time it is useful to use an antihistamine and decongestant if needed. o NOTE: These can be very drying, which can cause nasal bleeding. Warn patients of drying effect. Avoid use in nasal trauma. Intranasal Antihistamine o Antihistamine for allergic and non-allergic rhinitis (including vasomotor rhinitis) o Example: azelastine (Astelin) 2 sprays/nostril twice a day o Good if patient’s only allergy symptoms are nasal If patient’s symptoms also include watery eyes, will need a systemic medication: o Oral antihistamine (discussed above) o Caution with older males: antihistamines can cause urinary retention, especially in patients with BPH o Leukotriene inhibitor (Singulair 10 mg daily) 6 Asthma Types of Asthma o Allergic o May be seasonal or non-seasonal o Most likely cause: allergens (antigens) such as animal dander, dust, and molds o Idiopathic o Most likely cause: poorly defined etiologic factors; may be induced by stress, respiratory infections or strenuous exercise o Mixed o Most likely cause: combination of allergens and some of the idiopathic factors Pharmacologic Treatment Options o Beta-Agonists (=sympathomimetics) o Cause relaxation of the smooth muscle that surrounds the airways o May stimulate alpha and beta receptors, beta1 and beta2 receptors, or just beta1 receptors o Beta2 stimulants are the most specific for the lungs and have the fewest side effects o Examples: Beta2 agonist: albuterol (ProAir HFA, Proventil HFA, Ventolin HFA); levalbuterol (Xopenex HFA) Alpha-beta agonist: epinephrine (Adrenalin, Primatene, Bronkaid) Long-acting: salmeterol (Serevent) – 2 puffs every 12 hours Long-acting: formoterol (Foradil Aerolizer) – 12 mcg inhalation every 12 hours (12 mcg/powder cap) Long-acting: indacaterol (Arcapta Neohaler) 75 mcg/capsule inhaled once daily CAUTION: A 2002 study (Salmeterol Multi-center Asthma Research Trial [SMART] showed a statistically significant greater number of primary events and asthma-related events, including deaths, in patients taking salmeterol compared to those taking placebo. This was seen in African Americans enrolled in the study, but not in Caucasian patients in the study. Recommendations: National Asthma Education and Prevention Program (NAEPP) guidelines recommend patients requiring more than as-needed shortacting beta2 agonists should be prescribed regular and adequate doses of an inhaled anti-inflammatory asthma medication, such as inhaled corticosteroids, for optimal benefit in the management of their asthma. Consistent with these 7 guidelines and reinforced by trends seen in the interim analysis of the SMART data, GlaxoSmithKline recommends that patients receiving salmeterol for asthma should normally also be receiving regular and adequate doses of an effective asthma controller medication, such as inhaled corticosteroids. (Source: Safety information released by GSK in 2003) New as of 2010: The FDA required label changes and other initiatives to promote safe use of long-acting beta agonist (LABA) agents, noting that these agents should never be used alone in children or adults with asthma. This affected the two single-agent LABAs approved for asthma: salmeterol (Serevent) and formoterol (Foradil). The labels were changed to require that the drugs always be used in combination with an asthma controller medication such as an inhaled corticosteroid. (Also applies to newest LABA, Arcapta) o Contraindications to use: history of cardiac disease, dysrhythmias, angina, CAD, HTN, seizure disorders. o Side effects: tremor, insomnia, restlessness, vascular headache o Interactions: o Beta-agonist bronchodilator + nonselective beta-blocker = antagonizes the bronchodilation o For patients with diabetes: epinephrine increases blood glucose levels o Inhaled Corticosteroids o Work by stabilizing the membranes of cells that release harmful bronchoconstricting substances o Not first-line agents; commonly used when conventional short-acting bronchodilators fail o Examples: beclomethasone (Qvar HFA), budesonide (Pulmicort Flexhaler), ciclesonide (Alvesco), flunisolide (Aerospan HFA), fluticasone (Flovent HFA, Flovent Diskus), mometasone (Asmanex HFA, Asmanex Twisthaler) o Inhaled steroids do not suppress HPA axis except at high doses o Combination Products o Examples: fluticasone/salmeterol (Advair Diskus 100/50, 250/50, 500/50), budesonide/formoterol (Symbicort 80/4.5, 160/4.5), mometasone/formoterol (Dulera 100/5, 200/5) o If not currently on a steroid, can start with lower dose (such as Advair 100/50) o If currently on a steroid, start with higher dose (such as Advair 250/50 or 500/50) o Taper to lowest effective dose 8 o Anticholinergics o Work by blocking the bronchoconstrictive effects of acetylcholine o Used for maintenance and not relief of acute bronchospasm associated with COPD (chronic bronchitis and emphysema) (** Not asthma) o Examples of agents o umeclidinium/vilanterol (Anoro Ellipta) o ipratropium bromide (Atrovent HFA) o albuterol/ipratropium (Combivent Respimat) o tiotropium (Spriva HandiHaler, Spiriva Respimat) o aclidinium (Tudorza Pressair) o Indirect-Acting Agents o Work by stabilizing the mast cell wall, thereby preventing potentially harmful vasoconstrictive substances from being released o Only used prophylactically; available in nebulization form o Example: cromolyn sodium o Xanthines o Work by inhibiting phosphodiesterase, which breaks down cAMP, which is needed to relax smooth muscles o Examples: caffeine, theophylline o Theophylline is the most common xanthine used; aminophylline is the parenteral form of theophylline o Contraindications to use: history of GI tract disorders or peptic ulcer disease o Factors affecting theophylline clearance o Decrease clearance: cimetidine, erythromycin, allopurinol, propranolol, OCPs, ciprofloxacin, norfloxacin, ofloxacin, febrile viral illness o Increase clearance: rifampin, carbamazepine, phenobarbital, phenytoin, smoking, high-protein diet, charcoal broiled meat o Theophylline half-life: o Neonates: 20-30 hours o Child 1-12 years old 3-4 hours o Nonsmoking adult 7-8 hours o Smoking adult 4-5 hours o Elderly 9-10 hours o Leukotriene Receptor Antagonists o Used only for long-term control of asthma o Affect the late phase of the asthmatic response 9 o Block binding of leukotriene D4 to its receptor; alters pathophysiology associated with inflammatory process that contributes to signs/symptoms of asthma o Useful alternative if patients are unable to tolerate the side effects of the other medications o May be effective as first-line therapy for patients with mild-to-moderate asthma when used alone or in combination with beta-agonists used PRN o May be especially effective in patients with exercise or aspirin-induced asthma o Oral administration is useful for patients who have difficulty using inhalers o Very low incidence of side effects o Examples montelukast (Singulair) – 10 mg once daily in evening zafirlukast (Accolate) – 20 mg twice daily (take 1 hour before or 2 hours after meals) zileuton (Zyflo, Zyflo CR) – Zyflo 600 mg 4X/day; Zyflo CR 1200 mg twice daily within 1 hour after morning and evening meals. Monitor LFTs o Use of Inhaler o Only 10-15% of the dose actually gets to the lungs; only 30-45% of patients use proper technique o Use of spacer o Use of non-HFA devices: diskus, respimat, twisthaler, etc. o How to check if full-empty – floating in water is NOT adequate; need to count doses, keep a spare! o Demonstrate/return demonstration o If using separate bronchodilator and steroid: Use bronchodilator (beta-agonist) first, wait 2-5 minutes, then use inhaled steroid o Rinse mouth after using steroid