Thyroid disease in pregnancy
advertisement
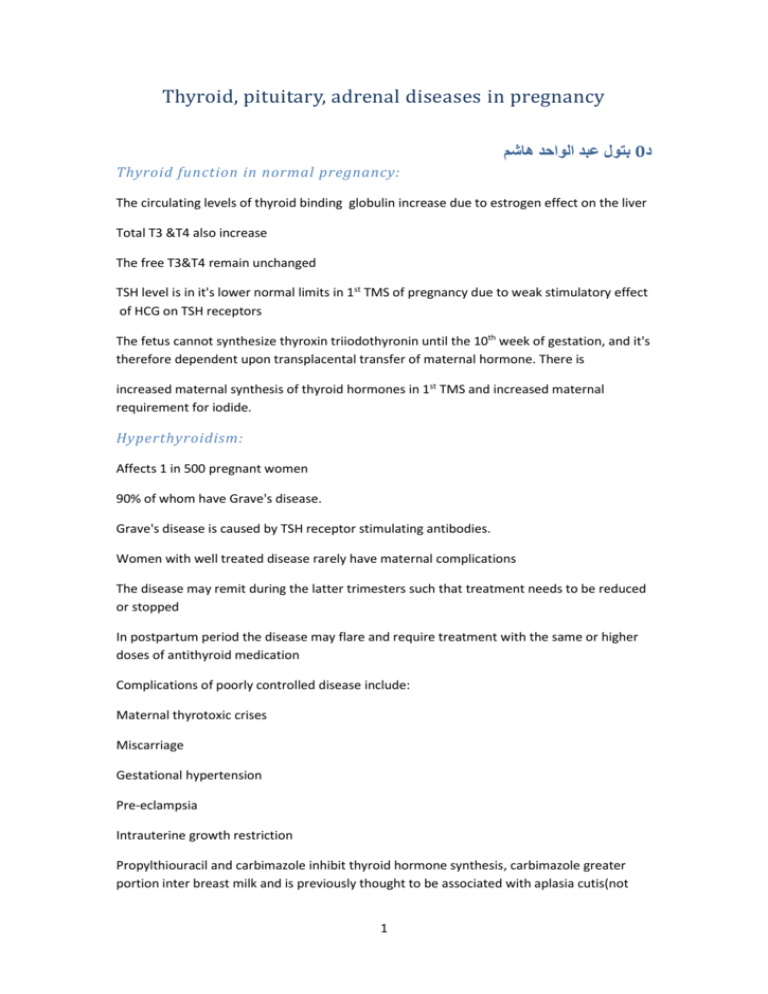
Thyroid, pituitary, adrenal diseases in pregnancy بتول عبد الواحد هاشم0د Thyroid function in normal pregnancy: The circulating levels of thyroid binding globulin increase due to estrogen effect on the liver Total T3 &T4 also increase The free T3&T4 remain unchanged TSH level is in it's lower normal limits in 1st TMS of pregnancy due to weak stimulatory effect of HCG on TSH receptors The fetus cannot synthesize thyroxin triiodothyronin until the 10th week of gestation, and it's therefore dependent upon transplacental transfer of maternal hormone. There is increased maternal synthesis of thyroid hormones in 1st TMS and increased maternal requirement for iodide. Hyperthyroidism: Affects 1 in 500 pregnant women 90% of whom have Grave's disease. Grave's disease is caused by TSH receptor stimulating antibodies. Women with well treated disease rarely have maternal complications The disease may remit during the latter trimesters such that treatment needs to be reduced or stopped In postpartum period the disease may flare and require treatment with the same or higher doses of antithyroid medication Complications of poorly controlled disease include: Maternal thyrotoxic crises Miscarriage Gestational hypertension Pre-eclampsia Intrauterine growth restriction Propylthiouracil and carbimazole inhibit thyroid hormone synthesis, carbimazole greater portion inter breast milk and is previously thought to be associated with aplasia cutis(not 1 proved), and therefore propylthiouracil is the drug of choice. Both drugs may rarely cause neutropenia and agranulocytosis, and patients need to be aware of bone marrow suppression if sore throat developed. Both drugs cross the placenta, however, fetal /or neonatal hypothyroidism is rarely seen Women need to be encouraged to breast feed their babies before taking the medication and to take divided doses, and their infants to be reviewed Thyrotoxic crises (thyroid storm) are a medical emergency present with exaggerated features of hyperthyroidism, hyperpyrexia, congestive HF, dysrhythmias, and an altered mental state. Precipitated by; infection, abrupt cessation of medication, surgery and labour. It must be treated immediately as it can be life threatening. Treatment involves intravenous fluids, hydrocortisone, propranolol, oral iodine and antithyroid drugs. Hypothyroidism: Affect approximately 1% of pregnant women. Complications in pregnancy include Congenital abnormalities, hypertension, placental abruption, premature delivery, fetal growth restriction and postpartum hemorrhage, providing thyroxine replacement therapy is adequate, hypothyroidism is not associated with an adverse pregnancy outcome for the mother or fetus. Severe hypothyroidism affects the subsequent intelligence of the offspring. Treatment: thyroxine replacement, aiming T4 at the upper end of the normal range appropriate for each trimester of pregnancy. Thyroxine absorption is decreased by certain drugs including iron and calcium. Its best taken on an empty stomach 4 hrs before iron or any other supplement. Postpartum thyroiditis: Is associated with the presence of thyroid antiperoxidase antibodies incidence varies between2-16%. It's characterizes by initial hyperthyroidism phase that classically occurs 1-3 mo.postpartum followed by a hypothyroid phase, which usually resolves by 12 mo. After delivery. The hypothyroidism may require treatment with thyroxin, but treatment should be stopped after 1 year as most cases resolve. However, the likelihood of developing subsequent hypothyroidism in women who have had postpartum thyroiditis is up to 5%/year, so affected women should have their thyroid function checked regularly. 2 Pituitary disorders: Hyperprolactinaemia: Is an important cause of infertility and amenorrhea Causes: Mainly due to pituitary microadenoma Drugs(methyldopa, phenothiazines) Diagnosis: Serum prolactine level CT, MRI, scanning of the pituitary fossa. Treatment: 80% of the cases respond to dopamine agonist ( bromocriptine or cabergoline), which cause the tumor to reduce in size. Larger tumors may require surgery or radiotherapy, which is best done before pregnancy. Bromocriptine and cabergoline are usually stopped in pregnancy; it is rare for microadenoma to cause problems. It is important to monitor the visiual field during pregnancy. 1- If there is evidence of tumor growth during pregnancy 2-if there is macroadenoma >1 cm, dopamine ag. Should be recommenced. No evidence of teratogenesis for neither drug. Adrenal disorders : Cushing's syndrome: All adrenal tumors are rare in pregnancy, Cushing syndrome is characterized by increased glucocorticoid production, usually due to hyper secretion of ACTH from pituitary tumor, and however in pregnancy adrenal causes are more common Clinical features include Infertility Preterm labour Stillbirth Diagnosis is difficult because many symptoms mimic normal changes of pregnancy (striae, weight gain, weakness, glucose intolerance and hypertension) Plasma cortisol 3 Adrenal imaging with ultrasound, CT, MRI. Adrenal insufficiency (Addison's disease) Is usually an autoimmune process, Clinical features Exhaustion, nausea, hypotension, hypoglycemia, and weight loss Diagnosis is difficult in pregnancy because the serum cortisol instead of being characteristically decreased may be in the low-normal range due to the physiological increase in cortisol-binding globulin in pregnancy. Occasionally, the disease may present in crises. Treatment is with glucocorticoids and fluid replacement, which need to be increased at times of stress such as hyperemesis and delivery. Pheochromocytoma: Is a rare catecholamine-producing tumor.The tumor arising from the adrenal medulla in 90% of cases. In pregnancy it may present as hypertensive crisis and the symptoms may be similar to those of preeclampsia, a characteristic feature is paroxysmal hypertension, Diagnosis: is by measurement of catecholamines in a 24hr urine collection, and in plasma Treatment is alpha blockage withphentolamine. CS is the preferred mode of delivery as it minimizes the sudden rise in catecholamines associated with vaginal birth. 4