Biochemistry -Lipoprotein Structure
advertisement

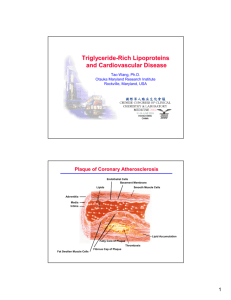
Very Low Density Lipoproteins (VLDL) High Density Lipoproteins (HDL) Lipoprotein Structure Protein part: Apoproteins (may be structural or transferred) or apolipoproteins Lipid part: Each lipoprotein contains different types of lipids in various combinations Type of lipids in a lipoprotein is governed according to the type of lipoprotein Spherical molecules of lipids and proteins (apoproteins) = amphipathic molecules Outer coat: Proteins: Apoproteins Lipids (amphipathic): Phospholipids (PL) &Free Cholesterol Inner core: Lipids (hydrophobic): Triglycerides (TG) & Cholesterol ester (CE) Apolipoproteins (Apoproteins): Five major classes (A-E) divided by structure & function, each has subclasses as Apo A, Apo CII Functions: Structural proteins ♥ Enzyme activators ♥ Recognition sites for cell-surface receptors Types of Lipoproteins: different in lipid & protein composition & therefore, they differ in: Size ♥ density ♥ Electrophoretic mobility Plasma Lipoproteins For triacylglycerol transport (TG-rich): - Chylomicrons: TG of dietary origin - VLDL: TG of endogenous (hepatic) synthesis For cholesterol transport (cholesterol-rich): - LDL: Mainly free cholesterol - HDL: Mainly esterified cholesterol Chylomicrons Synthesis: in intestinal mucosal cells Function: Transport dietary lipids from GIT to tissues (& liver). Responsible for physiological milky appearance of plasma (up to 2 hours after meal) Structure: Lowest density ♥ largest size ♥ highest lipid % ♥ lowest protein % ♥ highest triacylglycerol (dietary origin) Lipoprotein Lipase ♥ Extracellular enzyme anchored by heparan sulphate to the capillary walls of most tissue especially those of adipose tissue, cardiac & skeletal muscles BUT Adult liver does not have this enzyme ♥ its synthesis & transfer to luminal surface of the capillary is stimulated by insulin (in fed state) ♥ Activated by apoC-II Function of lipoprotein lipase ♥ hydrolyses circulating TG in chylomicrons to fatty acids & glycerol ♥ Fatty acids are stored (in adipose) or used for energy (in muscles) ♥ Glycerol is transferred to the liver (to be used for glycolysis, gluconeogenesis or lipid synthesis) Deficiency of lipoprotein lipase (or apo CII): ♥ causes type 1 hyperlipoproteinemia (familial lipoprotein lipase deficiency) ♥ accumulation of chylomicrons in plasma (hypertriglyceridemia) Lipoproteins 1 Tasneem Aldraye Synthesis: in the liver Structure: composed predominantly of triglycerides (TG) Function: To carry lipids (mainly TG) from the liver to tissues. In peripheral tissues, TG are degraded by lipoprotein lipase to FA & glycerol. Fatty liver (hepatic steatosis) Occurs when TG synthesis in liver is more than VLDL secretion As in cases of: Obesity Uncontrolled DM Chronic ethanol ingestion Low Density Lipoproteins (LDL) LDL is produced in the circulation as the end product of VLDLs Compared to VLDLs: It contains only apo B-10 Smaller size & more dense (less lipids) Lipid contents: Less triglycerides (TG) More cholesterol (C) & cholesterol ester (CE) Function of LDL Transport cholesterol from liver to peripheral tissues Uptake at tissue level by LDL receptor-mediated endocytosis recognized by apo B-100 Receptor-Mediated Endocytosis Synthesis: by intestine and liver Nascent HDL: Disk-shaped Contains apo A-I, C-II and E Contains primarily phospholipid (PC) Mature HDL (HDL2): First, the HDL3 collects cholesterol (C) from peripheral tissues & other lipoproteins. Then, Cholesterol is converted to CE (by PCAT) to form HDL2. CE is transported to liver by HDL2. Composition of LDL and HDL Low density lipoprotein (LDL) Mostly free cholesterol High density lipoprotein (HDL) Mostly cholesterol ester More % protein More % phospholipids Functions of HDL Reservoir of apoproteins e.g. Apo C-II and E to VLDL Uptake of cholesterol: From peripheral tissue (& other lipoproteins) Esterification of cholesterol: Enzyme: PCAT/LCAT Activator: Apo A-I Substrate: Cholesterol, Co-substrate: PC Product: Cholesterol ester (& Lyso-PC) Reverse cholesterol transport Transports cholesterol from peripheral tissues to liver Why Is HDL a Good Cholesterol carrier? Inverse relation between plasma HDL levels and atherosclerosis Reverse cholesterol transport involves: Efflux of cholesterol from peripheral tissues and other lipoproteins to HDL3 Esterification of cholesterol & binding of HDL2 to liver (and steroidogenic cells) by scavenger receptor class B (SR-B1) Selective transfer of cholesterol ester into these cells Release of lipid-depleted HDL3 LDL Receptor-Mediated Endocytosis: Regulation Low Density Lipoprotein Cholesterol (LDL-C) LDL-C = Total cholesterol – [HDL-C + TG/2.2 ] in case of mmol/L or 5 in case of mg/dL Lipoproteins 2 Tasneem Aldraye Lipoproteins 3 Tasneem Aldraye Lp (a): Simulates LDL but apo(a) covalently linked to apo B-100 Competes with plasminogen to plasminogen activator Genetical element Estrogen decreases it while trans fats increases it Lipoproteins and Related Clinical Problems Atherosclerosis Hypertension Coronary heart diseases Lipoproteinemias (hypo- and hyper-) Fatty liver Abnormalities in lipoprotein metabolism Hyperlipoprotenemias Type I hyperlipoproteinemia: Type II hyperlipoproteinemia : Familial lipoprotein lipase deficiency Familial hypercholesterolemia Due deficiency of lipoprotein lipase or apo C-II Due to deficiency of functional LDL receptors Slow clearance of TG–rich lipoproteins in plasma Reduced clearance of LDL (chylomicrons & VLDL) Elevation of plasma cholesterol (plasma TG remains Hypertriacylglyceremia (increased TG in blood) normal) Treated by reducing fat in diet Predispose to atherosclerosis & CHD Type III hyperlipoproteinemia Type IV hyperlipoproteinemia Familial dysbetalipoproteinemia Familial hypertriacylglycerolemia or broad B disease Increased production of VLDL Due to abnormal apo E (on chylomicrons) Commonly associated with type II DM & obesity Reduction of clearance of chylomicron remnants by Elevated blood TG & cholesterol liver Predispose to atherosclerosis & CHD. Accumulation of chylomicron remnants in plasma. Hyperchloesterolemia Predispose to atherosclerosis & CHD Hypolipoproteinemia Abetalipoproteinemia Familial hypobetalipoproteinanemia ↓ apo B-100 synthesis Defect in triacylglycerol transfer protein (MTP) responsible for loading of apo-100 with lipids with no ↓ VLDL ↓ blood TG & ↑ TG in liver chylomicrons & no VLDL synthesis ↓ LDL ↓ blood cholesterol No chylomicrons synthesis in intestine ↓ blood TG No VLDL synthesis in liver ↑ TG in liver No VLDL synthesis no LDL ↓ blood cholesterol Lipoproteins 4 Tasneem Aldraye