Wistozky, EM Chapter Six v.4 Author
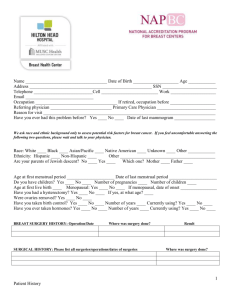
advertisement

Wistozky, EM Chapter Six v.4 Author-1: Eric M. Wistozky, MD Associate Director, Cancer Rehabilitation MedStar National Rehabilitation Hospital Chapter Six Managing Muscle Pain MUSCLE PAIN KEY POINTS May occur in up to 50% of people after breast cancer treatments Common causes include radiation fibrosis, myofascial pain, rotator cuff tendinitis, tennis elbow, and myalgias Exercise is often an effective treatment Psychological interventions can be beneficial Many different over-the-counter and prescription medications can help 1 1 INTRODUCTION 2 Muscle pain can be a serious and debilitating condition for some breast-cancer survivors. This 3 chapter will discuss why breast-cancer patients may develop muscle pain and how it can be 4 managed through conservative rehabilitation interventions. The first section of this chapter will 5 define pain. The different causes of muscle pain in breast cancer will then be explained. Lastly, 6 the multitude of conservative treatment options for muscle pain will be discussed. 7 SECTION I: WHAT IS PAIN? 8 Pain is an unpleasant sensation that is sent to your brain. Pain is something that you perceive. 9 It is a highly personal experience. This is why two people exposed to the exact same injury or 10 surgery may have a very different experience and perceive it in a different way. Have you ever 11 heard someone say that they have a “high pain tolerance”? Well, that person’s brain may just 12 perceive pain differently than someone else. Just like two people may react differently to being 13 pinched, two people may react differently to the exact same breast surgery. That is why it is 14 important to not put too much stock into another person’s experience. Your experience is your 15 own and may be completely different from else’s experience. 16 Keep in mind that there may be minimal pain after breast cancer treatment. You may 17 have a little pain for a short time, or a lot of pain for a long time, or somewhere in between. Up 18 to 50% of people after breast surgery may continue to have pain 2 years after breast surgery. 19 One study showed 17% of women with pain 12 years after breast surgery. This is dependent 20 on many factors, particularly the type of surgery and other treatments such as chemotherapy 21 and radiation. Studies have shown that younger patients have a higher occurrence of persistent 22 pain, as do people who are overweight. Less invasive surgery results in a lower risk of pain, but 2 23 those with less invasive surgery still do develop pain. Up to 80% of patients after less invasive 24 breast surgery may have nerve pain symptoms as some point. Up to 23% of patients may have 25 an uncomfortable feeling that the breast is still there, also called “phantom pain”. 26 Acute pain generally refers to pain in the first month after surgery. The amount of acute 27 pain may depend on the type of surgery, the extent of the cancer, and if you have any surgical 28 complications. Good pain control during this period is very important because it has been shown 29 that people with more severe acute pain have a higher likelihood of having chronic persistent 30 pain. 31 Chronic pain is typically defined as pain which persists for greater than six months. 32 Unfortunately, it is difficult to predict who may develop chronic pain. Pain that can be due to the 33 trauma of surgery, over time can lead to persistent pain due to increased sensitivity of the 34 surgical area. The brain can become overly sensitive as well, so even though the surgical area 35 has healed completely, the brain may still perceive pain. This type of pain becomes very difficult 36 to treat. 37 The identification of pre-operative pain (pain before surgery) is very important. Some 38 types of pain that exist before cancer treatment can be worsened by breast surgery, 39 chemotherapy, and radiation. This is why it is important to discuss these problems with your 40 cancer doctors before treatment. If these problems can be addressed before cancer treatment, 41 there will be a decreased chance of pain after treatment. A physiatrist can manage these 42 problems before cancer treatment, which will decrease the severity of acute and chronic pain. 43 Here is an example: 44 45 A patient was recently diagnosed with right breast cancer. When her surgeon evaluated her, he noticed that her left shoulder motion was severely impaired due to pain. This was a 3 46 major concern considering that she would have great difficulty functioning after surgery if her 47 right arm was recovering from surgery while the left shoulder was already severely impaired. 48 The patient was referred to a physiatrist who diagnosed the patient with rotator cuff (definition. 49 See page 4) and biceps tendinitis (inflammation of the tendon). Given that the patient was 50 having surgery in a few weeks, the physiatrist performed injections of the rotator cuff and biceps 51 tendons which resulted in an immediate decrease in pain and improvement in motion. The 52 patient was also sent for a specific rehabilitation program with a physical therapist. The 53 combination of these treatments improved her left arm function which significantly helped her 54 functional recovery from breast surgery. 55 SECTION II: MUSCLE PAIN IN BREAST CANCER 56 There are many possible causes of muscle pain in breast cancer. Most of these problems occur 57 either due to surgical trauma, changes in body posture, or radiation. This section will discuss 58 these common causes of muscle pain. 59 Radiation Fibrosis 60 Radiation can lead to the chronic production of scar tissue (also called fibrosis) in the area of 61 radiation. This can cause tightness of muscles in the radiation path. Because they are under 62 the breast tissue, the chest muscles are most likely to be affected by this. When these muscles 63 get tight, they change the motion of the shoulder and can lead to other problems like rotator cuff 64 injury, which is discussed below. Because the rib muscles are involved in breathing, if these 65 muscles are overly tight or painful, even deep breaths can be uncomfortable. This can be 66 particularly problematic, as it may decrease the ability to exercise. Women often develop poor 67 posture after breast surgery, which makes this problem worse. 4 68 How is this managed? The first thing to do is “open up” the chest wall. These muscles 69 can be loosened by stretching the chest wall and improving posture. This will decrease pain 70 and prevent other shoulder problems, like rotator cuff tendinitis (huh?). “Myofascial release” is 71 often extremely helpful for this as well. This involves deep hands-on work, typically performed 72 by a physical therapist, to break up the scar tissue from radiation and “loosen up” these 73 muscles. 74 Myofascial Pain 75 This is a fancy term for muscle pain. The hallmark of true myofascial pain is the presence of 76 “trigger points”. These are tight bands of muscle tissue that you can feel. Have you heard 77 someone say they have a “knot” in their muscle? Well that knot may be a trigger point. When 78 pressed, these trigger points often radiate pain to other areas. This problem is also more 79 common after radiation. 80 The management of myofascial pain is very similar to what was discussed above for 81 radiation fibrosis. In addition to stretching and myofascial release, another treatment for this 82 problem is the “trigger point injection”. This involves using a very small needle to break up 83 some of these tight muscle areas. This treatment can be very effective for some patients. It is 84 typically a minimally painful procedure. 85 Rotator Cuff 86 The rotator cuff is a group of tendons that moves and stabilizes the shoulder. Wear and tear of 87 these tendons is common after breast cancer treatment. When the tendons are newly injured or 88 inflamed we call this tendinitis (itis = inflammation). After a while the problem is not really 89 inflammation of the tendon, but actually just wear and tear of the tendon. In that case, it is 5 90 called tendinopathy or tendinosis. Regardless of what you call it – it hurts! It can limit overhead 91 movement of the arm and it may hurt to sleep on the affected shoulder. When chest muscles 92 are too tight due to surgery and radiation, this can put more pressure on the rotator cuff, 93 resulting in pain. After breast surgery and radiation, there can be a tendency to overuse these 94 tendons, or to use them improperly. 95 So how is this managed? After a physiatrist diagnoses a rotator cuff problem, a specific 96 rehabilitation program will be prescribed. Stretching the tight chest wall muscles helps. 97 Strengthening the muscles around the shoulder blade takes the pressure off the rotator cuff 98 tendons, and helps the shoulder move normally. If this doesn’t work, cortisone injections 99 around the rotator cuff may be helpful. 100 Tennis elbow 101 What does tennis have to do with breast cancer? Well, a common problem that occurs in tennis 102 players can occur in breast cancer survivors. Tennis elbow is caused by overuse of tendons 103 that start at the elbow and extend to the wrist. Repetitive movement at the wrist can lead to this 104 elbow pain. Breast cancer survivors may have a tendency to overuse their elbows and wrists, 105 since they are avoiding using their shoulder due to pain. This can result in tennis elbow (also 106 called lateral epicondylitis). 107 Tennis elbow can often be treated successfully with rehabilitation techniques. A special 108 brace called a counterforce brace can be helpful. Physical or occupational therapists can help 109 stretch and slowly strengthen the appropriate muscles to decrease pain. If these techniques 110 don’t work, injections by a physiatrist are also an option. 111 Myalgias 6 112 Myalgias, or achy muscles, are a potential side effect of chemotherapy treatments. They can 113 also be caused by medications that many breast cancer patients are on, such as tamoxifen or 114 aromatase-inhibitors. These medications are extremely important because they may decrease 115 the risk of cancer recurring. However, they can have the side effect of achy joints or muscles 116 anywhere in the body. 117 For most people, these symptoms can be reduced by simple over the counter 118 medications like acetaminophen (Tylenol) or non-steroidal anti-inflammatory drugs (NSAIDs) 119 like ibuprofen or naproxen. Topical pain medications, which are applied to the skin may also be 120 used. If these medications are not effective, nerve stabilizing medications (like gabapentin or 121 pregabalin) can be helpful as well. Nerve stabilizing medications and their side effects are 122 discussed in more detail in the “Managing Nerve Pain” chapter. 123 Exercise may be an important component of managing these symptoms. Specifically, 124 aerobic exercise (such as walking, running, biking, swimming) appears to be the most helpful. 125 A physical therapist can direct a program of slowly progressive stretching and strengthening 126 program which can help these symptoms. A physiatrist’s evaluation can determine what kind of 127 exercise is safe and help to design the appropriate program. 128 SECTION III: EXERCISE FOR PAIN 129 Exercise has not been clearly proven to improve pain in breast cancer survivors, but it certainly 130 helps with fatigue, mood, endurance, body image, and a sense of well being. There are also 131 many indirect effects of exercise which should help with pain. Weight loss may decrease joint 132 pain by decreasing the load on the body’s joints. Exercise helps with mood and sleep, both of 133 which can be correlated with pain. More specific information about exercise will be discussed in 7 134 the exercise chapter in this book (chapter 14). Again, as not all types of exercise are safe from 135 everyone, a physiatrist’s evaluation can help determine what type of exercise is safe. 136 SECTION IV: PSYCHOLOGICAL INTERVENTIONS FOR PAIN 137 The majority of cancer patients experience some form of depression or anxiety. This is 138 generally due to fear of death, anxiety about diagnostic tests, fear of painful and invasive 139 procedures, and the fear of cancer coming back after it is successfully treated. It has been 140 shown that anxiety and depression may contribute to pain. 141 Many different psychological strategies can be helpful and need to be patient specific. 142 Simple education about the cancer itself, cancer treatments, and expectations can often 143 decrease anxiety. A simple lack of understanding of the disease can lead to fear. The cancer 144 patient often feels out of control. Knowledge about the disease is empowering and helps the 145 patient regain control. Coping skills can be learned, which can help during the navigation of the 146 cancer treatment course. Many people feel somewhat depressed or anxious during or after 147 cancer treatments, which is often called an adjustment disorder (adjusting to a difficult life 148 circumstance). If the depression or anxiety is more severe it may require treatment with talk 149 therapy or medications. 150 A pain psychologist can be critical to helping with depression and anxiety’s effects on 151 pain. Many patients who have had chronic pain that were not helped by exercises, physical 152 therapy, medications, or injections have improved significantly by working with a pain 153 psychologist (a PhD psychologist with special training in the treatment of pain). Being sent to a 154 pain psychologist does NOT mean you are crazy. The pain psychologist can implement mental 155 techniques to help you decrease your perception of pain. Remember from the beginning of this 156 chapter – pain is a perception! Hypnosis is one such technique that can help reduce pain. One 8 157 advantage of hypnosis is that one can be taught to do it at home. It has been found to be useful 158 for both acute and chronic pain. Learning imagery skills can help you will your mind into 159 perceiving less pain. These techniques can be helpful even if there is no anxiety or depression. 160 By using the power of the mind, pain can be decreased. 161 If you feel these techniques could be beneficial to you, ask your physiatrist to find you a 162 pain psychologist. A more detailed discussion of psychological ramifications of breast cancer 163 will be discussed in chapter 15. 164 SECTION V: MEDICATIONS FOR MUSCLE PAIN 165 Pain symptoms can often be managed with over-the-counter medications. Please keep in mind 166 that even over-the-counter medications can have side effects and interact with other 167 medications you are taking. Therefore, please talk to your doctor before using any over-the- 168 counter medication regularly. 169 NSAIDs (Non-Steroidal Anti-Inflammatory Drugs) 170 These medications, such as ibuprofen and naproxen can be very effective for pain. They are 171 anti-inflammatories, so they can be helpful if inflammation is part of the cause of pain. Caution 172 is recommended if you have a history of acid reflux, stomach ulcers, heart, or kidney problems. 173 Taking these medications with food can often be helpful to prevent an upset stomach. Again, 174 always discuss the use of these medications with your doctor. 175 Acetaminophen 176 This medication (most commonly known as Tylenol) is another helpful over-the-counter pain 177 medication. It is not an anti-inflammatory like ibuprofen. Acetaminophen has been shown to be 9 178 particularly effective for headaches, which are common in those with cancer. The big concern 179 about this medication, is that it can affect the liver. PLEASE consult your doctor to make sure 180 your liver is healthy and that this medication will not interact with other medications you are 181 taking. 182 Topical Medications (medications applied to the skin) 183 I find these medications particularly helpful for those with breast cancer. These are pain 184 medications that can be rubbed on to the painful area. People love these medications for many 185 reasons. First of all, the “massaging” effect of rubbing a pain medication into the uncomfortable 186 area is comforting. When you are applying the medication to your own body by hand, it really 187 makes you feel like you are in charge of your own pain relief. Secondly, these topical 188 medications rarely cause side effects or interact with other medications. Oral pain medications 189 commonly have side effects and cancer patients are sick of dealing with side effects. In 190 addition, if you are on other medications, you may not want to take yet ANOTHER medication or 191 deal with potential interactions between your medications. 192 Another reason why topical medications are effective, is that most of this pain is caused 193 by very superficial structures that are affected by radiation or surgery. Therefore, the topical 194 medication can penetrate directly to the area causing pain, which can be very effective. Studies 195 have shown that these medications may penetrate 1-2 inches under the skin. Why take a pain 196 medication by mouth that goes throughout the whole body, when you can apply medication 197 directly to the site of pain? 198 There are several options for topical pain medications. Some are over the counter and 199 some require a prescription. Over the counter medications usually contain ingredients like 200 capsaicin, menthol, and aspirin. These have been shown to be effective to some degree. Use 10 201 caution when using an aspirin-containing medication if you already taking aspirin or any other 202 blood thinning medication. A prescription option that is commonly used is a topical anesthetic 203 (lidocaine) which numbs the painful area. This can be given in the form of a cream, gel, or 204 patch, which can often be very effective. Another commonly used prescription topical pain 205 medication is a topical anti-inflammatory. This is like taking an NSAID (discussed above), but 206 topically. These are available as gels, creams, liquids, or patches. 207 Another option is a topical compound. What is great about a compound is that you can 208 combine multiple medications into a cream to treat pain. Pain, especially in breast cancer, often 209 has many causes. There is typically pain due to muscle spasm, inflammation, and nerve 210 irritation. If there are multiple causes of the pain, why treat just one of those causes? A topical 211 compound can combine medications that treat all the causes of your pain with a very low 212 likelihood of any side effects. Many doctors may not have experience prescribing compounds, 213 so you can ask your doctor to refer you to another specialist that is comfortable prescribing 214 these. 215 Opiates 216 Opiates are the “strong” pain medications that most people know of as percocet, vicodin, 217 oxycodone, oxycontin, morphine, etc. These medications are very commonly prescribed to 218 cancer patients, for two reasons. Pain in cancer is thought to be very severe, so doctors often 219 want to pull out the “big guns” to treat pain. Secondly, cancer patients may have a decreased 220 life expectancy, so why not give them the strong stuff? There are a few reasons why these 221 sentiments may be incorrect: 222 223 Cancer doctors are often using less invasive methods for cancer treatment. Surgeries are becoming less extensive and radiation fields are getting smaller. 11 224 Therefore, theoretically, the pain caused by these interventions may be less 225 severe for some people. 226 As mentioned above when talking about topical compounds, the specific cause of 227 pain should be addressed. Opiates are not specific for any certain type of pain. 228 If your pain is from muscle – a muscle pain medication can be used. If your pain 229 is from nerve – a nerve pain medication can be used. Just because the opiates 230 are “strong”, doesn’t mean they will work the best for these specific causes of 231 pain. 232 In many cases, the argument to give cancer patients strong pain medications 233 because they are going to die, is out the window. Many cancer patients are living 234 longer and longer. The death rate from cancer is declining every year as 235 treatments get better and better. The life expectancy, especially for many breast 236 cancer patients, is now quite good. After cancer treatment, patients may live 237 many years or may have a completely normal life expectancy. Therefore, it may 238 be more appropriate to consider other medications that are less addictive for the 239 long-term. 240 These medications can have serious potential side effects. In addition to the 241 potential for addiction mentioned above, they can cause severe constipation, 242 depression, can alter bodily hormone levels, and can even result in overdose and 243 death. 244 As you can see, pain in cancer can often be treated without opioid medications. 245 However, there certainly are cases when opioids may be appropriate. A physiatrist will treat 246 their patient as an individual to determine the best treatment plan for that person. 12 247 SECTION VI: INJECTIONS FOR MUSCLE PAIN 248 When other conservative treatment options fail, injection can be a last resort. There are many 249 minimally invasive injection options available which can be helpful for pain. What’s important to 250 keep in mind, is that the injection should be specific to what your doctor feels is the cause of 251 your pain. This is why it is important for your doctor to send you to a specialist, such as a 252 physiatrist, who can examine you to determine the exact cause of your pain. 253 254 255 One of the most commonly used procedures for muscle pain is the trigger point injection, which was discussed above on page 4. Other options include: Tendon injections: If the cause of the pain is due to a tendon problem, such as in 256 rotator cuff tendinitis or tennis elbow, an injection around the tendon, in conjunction 257 with rehabilitation techniques, can often be very helpful. Most commonly these 258 injections are done with anesthetic and corticosteroid (cortisone-a type of steroid). A 259 few corticosteroid injections are typically safe and effective, but having too many of 260 these injections around the same tendon, can potentially weaken the tendon over 261 time and worsen the problem. There are other newer injection techniques which 262 may help to regenerate wear and tear of a tendon (so called “regenerative 263 procedures” such as platelet-rich plasma and prolotherapy), but these need more 264 research before becoming the standard of care. At this time, most insurance 265 companies do not cover these injections. 266 Botulinum toxin injections: These injections, most commonly known as botox, can 267 be helpful to relax tight muscles or trigger points. If muscle pain continues despite 268 rehabilitation, medications, and trigger point injections, these injections can be an 269 option. More research is needed to recommend these injections as a standard 13 270 treatment, but there are some reports of success in cancer patients. Also, insurance 271 does not always cover these injections. 272 CONCLUSION 273 There are many potential causes of muscle pain in breast cancer patients. Ideally, 274 addressing pain which exists before cancer treatment, will help with long-term outcomes. 275 When your doctor assesses your pain, it is important to have a specific diagnosis of the 276 cause of your pain. The physiatrist can be critical to determining a precise diagnosis. Once 277 a diagnosis has been determined, a specific treatment plan can be designed. Often, 278 successful treatment can take place without invasive interventions, and often without any 279 medications. You don’t have to live with this pain forever, and often there are many things 280 that can be done to help you. 281 Important Points to Remember 282 There are many potential causes of muscle pain in breast cancer patients. 283 Effective treatment of pain begins with a correct diagnosis. 284 A physiatrist is trained to make a precise diagnosis and prescribe a comprehensive 285 treatment plan that often involves a team of knowledgeable health professionals. 286 Good pain control early reduces the likelihood of having chronic persistent pain. 287 Successful treatment can often occur without invasive interventions or medications. 14 288 Glossary 289 Acute - Having a sudden onset, sharp rise, and short course. 290 Aerobic - Exercise which involves increasing oxygen consumption for the body, such as 291 running, walking, swimming, etc. 292 Chronic - Marked by long duration or frequent recurrence. 293 Compound - A cream formed by combining multiple different components. 294 Fibrosis - Collection of scar tissue. 295 Hypnosis - A trance-like state that resembles sleep but is induced by a person whose 296 suggestions are readily accepted by the subject. 297 Inflammation- A response to injury marked by blood vessel dilation, white blood cell infiltration, 298 redness, heat, and pain that serve as a mechanism to eliminate noxious agents and damaged 299 tissue. 300 Myalgias - Pain in one or more muscles. 301 Myofascial - Pain related to muscle and its surrounding tissue. 302 Physiatrist - A physician who specializes in physical medicine and rehabilitation. This physician 303 non-surgically manages functional, neuromuscular, and musculoskeletal impairments with a 304 focus on improving function and quality of life. 305 Tendinitis - Inflammation of a tendon 306 Tendinopathy - Degeneration of a tendon. 15 307 Tendinosis - Degeneration of a tendon. 308 Tendon - A tough band of tissue that connects a muscle with bone. 309 Topical - Designed to be applied on the surface of the body such as an ointment or a cream. 16 310 Symptom Index 311 Tightness 312 Knots 313 Achy 314 Headaches 315 Muscle spasm 17 316 Additional Reading/Resources: Unfortunately, there are not many good articles for the 317 general reader about muscle pain in breast cancer survivors. The web-links below can be 318 helpful. Also, listed are two excellent publications in the scientific literature on this topic. 319 http://www.cancer.net/survivorship/rehabilitation 320 http://www.cancer.net/survivorship/late-effects 321 Ebaugh D, Spinelli B, Schmitz KH. Shoulder impairments and their association with 322 symptomatic rotator cuff disease in breast cancer survivors. Med Hypotheses, 2011 Oct; 77(4): 323 481-7. 324 325 Gartner R, Jensen M, Neilsen J. Prevalence of and factors associated with persistent pain 326 following breast cancer surgery. JAMA 2009;302(18):1985-1992. 18