TG2 Hanlon-Dearman simulation Sept 2011
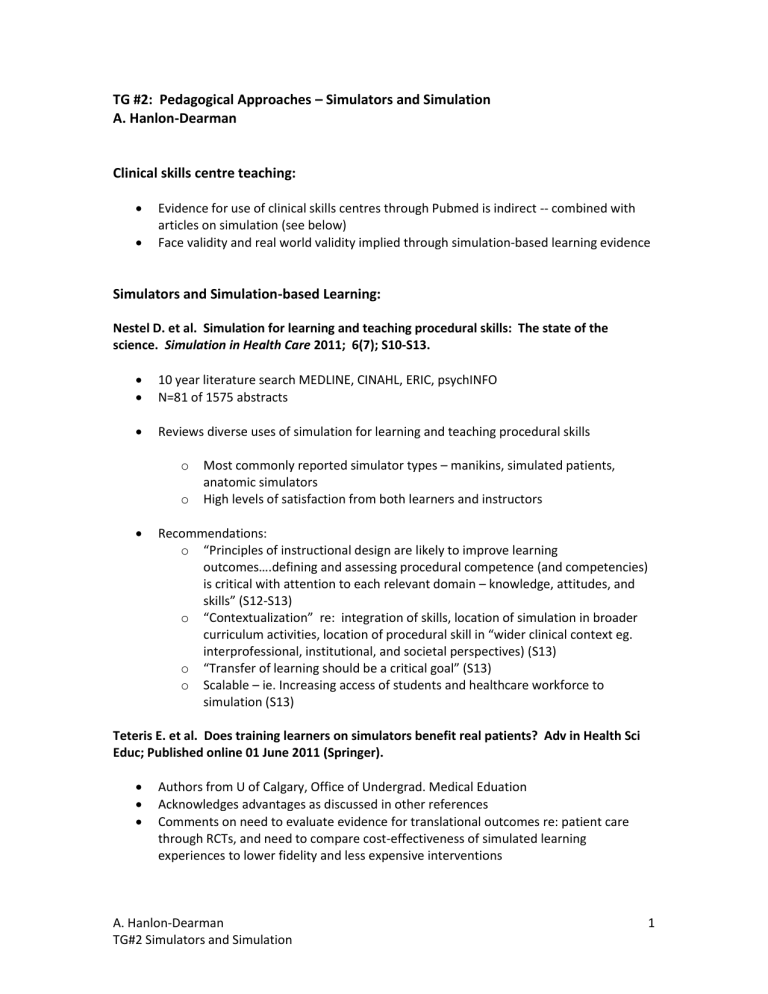
TG #2: Pedagogical Approaches – Simulators and Simulation
A. Hanlon-Dearman
Clinical skills centre teaching:
Evidence for use of clinical skills centres through Pubmed is indirect -- combined with articles on simulation (see below)
Face validity and real world validity implied through simulation-based learning evidence
Simulators and Simulation-based Learning:
Nestel D. et al. Simulation for learning and teaching procedural skills: The state of the
science. Simulation in Health Care 2011; 6(7); S10-S13.
10 year literature search MEDLINE, CINAHL, ERIC, psychINFO
N=81 of 1575 abstracts
Reviews diverse uses of simulation for learning and teaching procedural skills o Most commonly reported simulator types – manikins, simulated patients, anatomic simulators o High levels of satisfaction from both learners and instructors
Recommendations: o “Principles of instructional design are likely to improve learning outcomes….defining and assessing procedural competence (and competencies) is critical with attention to each relevant domain – knowledge, attitudes, and skills” (S12-S13) o “Contextualization” re: integration of skills, location of simulation in broader curriculum activities, location of procedural skill in “wider clinical context eg. interprofessional, institutional, and societal perspectives) (S13) o “Transfer of learning should be a critical goal” (S13) o Scalable – ie. Increasing access of students and healthcare workforce to simulation (S13)
Teteris E. et al. Does training learners on simulators benefit real patients? Adv in Health Sci
Educ; Published online 01 June 2011 (Springer).
Authors from U of Calgary, Office of Undergrad. Medical Eduation
Acknowledges advantages as discussed in other references
Comments on need to evaluate evidence for translational outcomes re: patient care through RCTs, and need to compare cost-effectiveness of simulated learning experiences to lower fidelity and less expensive interventions
A. Hanlon-Dearman
TG#2 Simulators and Simulation
1
Issenberg SB, et al. Features and uses of high-fidelity medical simulations that lead to
effective learning: a BEME systematic review. Medical Teacher 2005; 27(1): 10-28.
34 year systematic review; ERIC, MEDLINE, PsychINFO, Web of Science, Timelit; also hand search, grey lit, internet searches used
N=109 (initial screening pool of 670 articles)
Bottom lines: “The research evidence is clear that high-fidelity medical simulations facilitate learning among trainees when used under the right conditions [see
below]…The evidence also shows that simulation-based medical education complements, but does not duplicate, education involving real patients in genuine
settings [italics mine].” (p.24)
Recommendations for conditions of use of simulators: o “Provide feedback during learning experience… o Learners should repetitively practice skills on the simulator… o Integrate simulators into overall curriculum… o Learners should practice with increasing levels of difficulty… o Adapt simulator to complement multiple learning strategies… o Ensure simulator provides for clinical variation… o Learning on the simulator should occur in a controlled environment…. o Provide individualized (in addition to team) learning on the simulator … o Clearly define outcomes and benchmarks for the learners to achieve using the simulator…. o Sensure the simulator is a valid tool” (p.23,26, and Table 4)
Okuda Y, et al. The utility of simulation in medical education: What is the evidence? Mount
Sinai Journal of Medicine 2009; 76:330-343.
MEDLINE search: “simulation, mannequin simulator, partial task simulator, graduate medical education, undergraduate medical education, and continuing medical education”
N=113 – good list of references
Foundation for use of simulation David Kolb: “medical learning …benefit from experiential learning....4 stages: (1) concrete experience, (2) observation and reflection,
(3) abstract concept formation, and (4) active experimentation in which generalizations are tested and new hypotheses are developed to be tested in future concrete experiences.” (p.333-334)
A. Hanlon-Dearman
TG#2 Simulators and Simulation
2
Okuda et al 2009
“proved to be superior to the traditional problem based learning format” in learning critical care management (p.334) -- references Steadman et al RCT 4 th year med students re: management of acute dyspnea
article reviews evidence for wide variety of use in undergrad (and grad) med education: o basic science: teaching physiology, pharmacology, neurosciences, cardiology, medical reasoning o physical examination o clinical skills training/procedural training o clinical clerkships
strengths of simulation based learning: o Student: opportunity to practice patient care in controlled environment away from bedside, adult learning principles, opportunity for “deliberate practice toward knowledge and skills mastery” (p.339) o Patient: “increases the likelihood of a minimum competency level prior to clinical interaction and medical decision making. Patients are more willing to allow students to perform procedures … after they have undergone simulation training (references Graber et al 2005)
limitations of simulation: faculty time, lack of faculty training, cost of equipment
A. Hanlon-Dearman
TG#2 Simulators and Simulation
3
Selected References: (thorough reference lists described in articles below esp. Issenberg)
Graber MA et al. Does simulator training for medical students change patient opinions and attitudes toward medical student procedures in the emergency department? Acad Emerg Med
2005; 12: 635-639, ix.
Issenberg SB, et al. Features and uses of high-fidelity medical simulations that lead to effective learning: a BEME systematic review. Medical Teacher 2005; 27(1): 10-28.
Nestel D. et al. Simulation for learning and teaching procedural skills: The state of the science.
Simulation in Health Care 2011; 6(7); S10-S13.
Okuda Y, et al. The Utility of Simulation in Medical Education: What is the Evidence? Mount
Sinai Journal of Medicine 2009; 76:330-343.
Steadman, RH, et al. Simulation-based training is superior to problem based learning for the acquisition of critical assessment and management skills. Crit Care Med 2006; 34:151-157.
Teteris E. et al. Does training learners on simulators benefit real patients? Adv in Health Sci
Educ; Published online 01 June 2011 (Springer).
A. Hanlon-Dearman
TG#2 Simulators and Simulation
4