DOCX ENG
advertisement

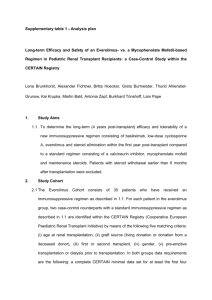
H- 12 : Immunosuppressive regimens H- 14 : acute rejection Alemtuzumab-based induction treatment versus basiliximab-based induction treatment in kidney transplantation (the 3C Study): a randomised trial The 3C Study Collaborative Group Journal :The Lancet Year : 2014 / Month : November Volume : 384 Pages : 1684–1690 ABSTRACT Background Calcineurin inhibitors (CNIs) reduce short-term kidney transplant failure, but might contribute to transplant failure in the long-term. The role of alemtuzumab (a potent lymphocyte-depleting antibody) as an induction treatment followed by an early reduction in CNI and mycophenolate exposure and steroid avoidance, after kidney transplantation is uncertain. We aimed to assess the efficacy and safety of alemtuzumab-based induction treatment compared with basiliximab-based induction treatment in patients receiving kidney transplants. Methods For this randomised trial, we enrolled patients aged 18 years and older who were scheduled to receive a kidney transplant in the next 24 h from 18 transplant centres in the UK. Using minimised randomisation, we randomly assigned patients (1:1; minimised for age, sex, and immunological risk) to either alemtuzumab-based induction treatment (ie, alemtuzumab followed by low-dose tacrolimus and mycophenolate without steroids) or basiliximab-based induction treatment (basiliximab followed by standard-dose tacrolimus, mycophenolate, and prednisolone). Participants were reviewed at discharge from hospital and at 1, 3, 6, 9, and 12 months after transplantation. The primary outcome was biopsy-proven acute rejection at 6 months, analysed by intention to treat. The study is registered at ClinicalTrials.gov, number NCT01120028, and isrctn.org, number ISRCTN88894088. Findings Between Oct 4, 2010, and Jan 21, 2013, we randomly assigned 852 participants to treatment: 426 to alemtuzumab-based treatment and 426 to basiliximab-based treatment. Overall, individuals allocated to alemtuzumab-based treatment had a 58% proportional reduction in biopsy-proven acute rejection compared with those allocated to basiliximab-based treatment (31 [7%] patients in the alemtuzumab group vs 68 [16%] patients in the basiliximab group; hazard ratio (HR) 0·42, 95% CI 0·28–0·64; log- rank p<0·0001). We detected no between-group difference in treatment effect on transplant failure during the first 6 months (16 [4%] patients vs 13 [3%] patients; HR 1·23, 0·59–2·55; p=0·58) or serious infection (135 [32%] patients vs 136 [32%] patients; HR 1·02, 0·80–1·29; p=0·88). During the first 6 months after transplantation, 11 (3%) patients given alemtuzumab-based treatment and six (1%) patients given basiliximab-based treatment died (HR 1·79, 95% CI 0·66–4·83; p=0·25). Interpretation Compared with standard basiliximab-based treatment, alemtuzumab-based induction therapy followed by reduced CNI and mycophenolate exposure and steroid avoidance reduced the risk of biopsy-proven acute rejection in a broad range of patients receiving a kidney transplant. Long-term follow-up of this trial will assess whether these effects translate into differences in long-term transplant function and survival. Funding UK National Health Service Blood and Transplant Research and Development Programme, Pfizer, and Novartis UK. COMMENTS A new drug in renal transplantation which lessen early acute rejection episodes. The introduction of calcineurin inhibitors (CNIs, such as ciclosporin and tacrolimus) as part of immunosuppression protocols in renal transplant recipients made a substantial contribution to the reduction in early transplant failure, but these treatments might also contribute to the subsequent decrease in transplant function and, ultimately, failure. There has therefore been interest in immunosuppression strategies that minimise CNI exposure to reduce the rate of late transplant failure. One such strategy is to use more potent induction treatment at the time of transplantation to allow CNI exposure to be minimised from the time of transplantation without increasing the risk of rejection. Alemtuzumab is a humanised monoclonal antibody directed against CD52 which is expressed almost exclusively on lymphocytes; monoclonal antibodies to CD52 cause profound lymphocyte depletion. 852 participants to treatment were randomly assigned: 426 to alemtuzumab-based treatment and 426 to basiliximab-based treatment . 32 (4%) of enrolled participants did not receive a transplant. Mean age was 52 years (SD 13), 552 (65%) were men, and most patients were white All characteristics were well-balanced . Patients entering the 3C Study were randomised equally either to alemtuzumab-based induction treatment (30 mg immediately after reperfusion and 24 h later, unless the participant was >60 years old, in which case the second dose was omitted) followed by low-dose tacrolimus (target trough concentration 5–7 ng/mL), and mycophenolic acid (360 mg twice daily) without steroids; or to basiliximab-based induction treatment (20 mg on days 0 and 4) followed by standard-dose tacrolimus (target trough concentration 5–12 ng/mL), mycophenolic acid (540–720 mg twice daily), and oral prednisolone. During the first 6 months after transplantation, 31 (7%) of the 426 participants allocated to alemtuzumab-based treatment had an episode of biopsy-proven acute rejection (BPAR) compared with 68 (16%) of patients allocated to basiliximab-based treatment, corresponding to a 58% proportional reduction with alemtuzumab-based treatment There was no statistically significant difference in the occurrence of either steroid-resistant rejection (two [1%] patients in the alemtuzumab group vs five [1%] patients in the basiliximab group; HR 0·40, 95% CI 0·08–2·04; p=0·25) or delayed graft function (defined as any dialysis in the first week after transplant: 127 [30%] vs 102 [24%]; odds ratio 1·35, 95% CI 1·00–1·83; p=0·054). There was no significant difference in graft function at 6 months (mean eGFR 50·1 mL per min per 1·73m2 [SE 1·0] in alemtuzumab-allocated participants vs 49·8 mL per min per 1·73m2 [1·0] in basiliximab-allocated participants). The occurrence of any cytomegalovirus (CMV) infections did not differ between groups. By contrast with CMV infections, BK virus infections were more common in the alemtuzumab-based treatment group compared with in the basiliximab-based treatment group. These findings suggest that alemtuzumab-based induction treatment (ie, alemtuzumab followed by reduced CNI treatment, low dose mycophenolate, and steroid avoidance) roughly halves the risk of acute rejection in the first 6 months after transplantation compared with standard basiliximab-based induction treatment. The hazard ratio of 0·42 for biopsy-proven acute rejection in this study is driven by a large proportional benefit of alemtuzumab-based treatment in the first few weeks after transplantation, All these effects are applicable to the broad range of patients who are candidates to kidney transplanation. Pr. Jacques CHANARD Professor of Nephrology