Version of Tox REview
advertisement

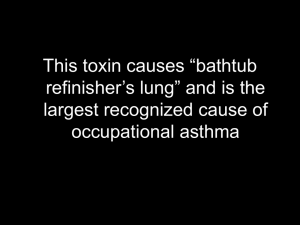
Acetaminophen Peak concentration usually within 4 hours post ingestion Metabolized first by hepatic glucuronidation/sulfation then after saturation, toxicity develops from formation of intermediate N-acetyl-p-benzoquinonimine (NAPQ1) by the CYP450 system NAPQ1 is detoxified by glutathione NAPQ1 is DIRECTLY toxic to kidney and liver Hepatic Zone 3 (centrilobular) is first/most affected by toxicity Toxicity produced at 7.5g in adults or 150 mg/kg in children Phase 1 – Nonspecific symptoms, N/V, malaise, fatigue Phase 2 – Begins at 24 hrs. Increased AST. RUQ pain Phase 3 – Begins at 72 hrs. Hepatic encephalopathy, coag defects, jaundice, renal failure Phase 4 – Begins at day 4. Recovery phase if damage was reversed. If not, death. Rumack Nomogram is applied at 4-24 hours If time unknown, treat if: AST elevated regardless of APAP level or at any elevated APAP >10 If [APAP] <50 at 1-4 hrs, then no risk of toxicity Perform gastric emptying if: <1 hr post ingestion or ER formula or coingestion of GI delaying agents Activated charcoal if: <4 hrs post ingestion 140 mg/kg ORAL loading dose NAC After 4 hours 70 mg/kg ORAL Q4H X17 doses (over 72 hours) Give IV NAC 150 mg/kg loading dose followed by 50 mg/kg over 4 hrs followed by 6.25 mg/kg/hr X 16 hrs or use same dosing schedule as oral Start NAC within 8 hours after ingestion but can start up to 24 hours after ingestion Hydrofluoric Acid Exposure to aluminum brighteners or rust removers (oil refiners, beer brewing, dental labs, sandstone cleaning) Fluoride ion interferes with calcium metabolism and Ca-dependent processes by combining with Ca and Mg Causes liquefactive necrosis of soft tissues (other acids cause coagulative necrosis) Inhibits Na-K ATPase which causes erythrocytes to release K causing HyperK Inhibits acetylcholinesterase causing acetylcholine excess (N/V, diarrhea, ab pain, weakness) Burns: concentrations <20% cause delayed pain, 20-50% pain at 1-8 hrs, >50% immediate pain Ingestion lethal dose: 1.5 g or 20 mg/kg Inhalation: Rarely noncardiogenic pulm edema Monitor Ca levels Q1H Tx: Topical 2.5% Ca gluconate gel for minor burns, Infiltrative Ca gluconate or Bier block technique for >20% [HF] burns, Intra-arterial therapy (radial/ulnar use 10mL of 10% in 40mL NS; brachial use 20mL of 20% in 80mL NS; infuse over 4 hrs; repeat if not pain free for 4 hrs) for burns involving >3 digits, Ca gluconate nebulized for inhalation injuries, Drop solution and irrigation with LR/milk for ocular exposure, Drink water/milk for ingestions is controversial If topical therapy fails (no improvement after 30 minutes), use infiltrative therapy Alkali Ingestions NaHydroxide, NaHypochlorite (bleach), Ammonia (Oven/drain/toilet bowl cleaners, disinfectant, dishwasher detergent, hair dyes, batteries) Each rise in pH of 1 represents a 10-fold increase in [OH] “Strength” refers to willingness of alkali parent compound to dissociate in aqueous solution Titratable Alkaline Reserve (TAR) – measure of resistance of a solution to changes in pH As TAR increases, causticity increases Causes liquefaction necrosis Absence of oral burns does not rule out esophageal injury First and most common site of injury is squamous epithelium of esophagus Incidence of squamous cell carcinoma increases 20-40X Esophageal strictures are common complications Tx: water/milk, endoscopy within 4-24 hrs except in asymptomatic accidental cases (prior to 4 hours underestimates burns and after 24 hrs risks perforation), steroids for second degree burns, prophylactic ampicillin for pts receiving steroids, perform esophageal stricture dilation after week 2, resume enteric feeds ASAP Do not give acid to neutralize as this causes greater thermal heat during neutralization reaction Antipsychotics Block dopamine receptors Low potency (chlorpromazine-thorazine, fluphenazine, hydroxyzine, prochlorperazinecompazine, promethazine-phenergan, thioridazine, mesoridazine) Block D2 receptors in mesolimbic system Most sedating due to anticholinergic effects Most likely to cause tardive dyskinesia/EPS bc blocks D2 in nigrostriatal High potency (Droperidol, haloperidol, thiothixene, trifluoperazine) Atypical (Clozapine, olanzapine-zyprexa, quetiapine-seroquel, risperidone, ziprasidone-geodon, aripiprazole) Block D2 and serotonin 2A Also treat negative symptoms NMS and cardiotoxicity least likely in this group Acute EPS: dystonia, akathisia, parkinsonism (caused by D2 blockade in nigrostriatal and reduced by muscarinic receptor antagonism) Tx: Benadryl, benztropine, benzos (continue Benadryl/benztropine X48hrs) Delayed EPS: tardive dyskinesia, tardive dystonia (caused by upregulation of D2 receptors) NMS caused by neuroregulatory dysfxn 2/2 D2 receptor blockade in substantia nigra/hypothalamus (develops within first 2 weeks of starting drug) Rigidity, fever, diaphoresis, AMS, tachycardia, leukocytosis, rhabdo Tx: Cool, hydrate, benzos, paralytics, bromocriptine/amantadine/dantrolene controversial Phenothiazines (chlorpromazine) possess quinidine-like effects (QT prolongation) – thioridazine, mesoridazine have greatest risk Butyrophenones (Haldol) prolong cardiac repolarization causing Torsades Clozapine – agranulocytosis, seizures, diabetes Olanzapine – diabetes, agranulocytosis Acute OD: sedation, pupils any size, orthostatic hypotension, MC rhythm is sinus tach Ethylene Glycol Antifreeze – sweet taste Peak concentration at 1-4 hrs post ingestion Metabolized to glycoaldehyde via ADH then to glycolic/glyoxilic/oxalic acid via ALDH These require NAD conversion to NADH. Altered ratio causes increased lactate. Liver metabolizes 80% t1/2 – 3 to 9 hrs If EtOH > 100, ADH sites are saturated causing decreased rate of EG metabolism Clinical: inebriation, hypocalcemia, ARF, AG met acidosis (2/2 increased glyColate) Stage 1 Neuro: 0-12 hrs, inebriation, no EtOH odor, N/V, AMS, cereb edema Stage 2 Cardiopulm: 12-24 hrs, tachy, HTN, compens hypervent, ARDS, most deaths Stage 3 Renal: 24-72 hrs, oliguria, flank pain, ARF, BM suppression ARF is generally reversible Indications for tx with antidote: Level >20 mg/dL or h/o drinking EG in combo with osmol gap >10 or clinical suspicion + two: art pH <7.3, bicarb <20, osmol gap >10, urine oxalate crystals Tx: Lavage if <1 hr post exposure Charcoal if mixed ingestion Labs – CBC, BMP, Mg, Ca, Osmol, EtOH, Volatile alcohols, Lactate, UA with microsco Continue antidote until EG nondetectable or <20 AND pt asymptomatic w/ normal pH Fomepizole preferred over EtOH (15 mg/kg then 10 mg/kg Q12HX4 doses then 15 mg/kg Q12H until EG<20 and pt asymptomatic with normal pH) EtOH only if hypersensitive to fomepizole HD if: severe met acidosis (pH <7.3) unresponsive to therapy, ARF, EG >50 mg/dL Bicarb if pH <7.3 If seizing, benzos/phenytoin (consider Ca for hypoCa) Endogenous half life of glycolic acid – 10 hrs Endogenous elimination rate – 1.08 mmol/L/h HD half life of glycolic acid – 2.5 hrs HD elimination rate – 170 ml/min [glycolic acid] correlates with AG but not pH or bicarb Methanol Colorless, Positive alcohol odor Solvent, windshield wiping fluid, gas line antifreeze, moonshine, model airplane fuel, perfumes Ingested, inhaled, dermal Peak concentrations in 30-60 minutes Metabolized to formaldehyde via ADH then to formic acid via ALDH then formic acid to H20/CO2 via folate dependent enzyme Zero order kinetics 10 mg/dL/hr Formic acid binds to cytochrome oxidase in mitochondria (similar to CO, cyanide, H sulfide) FA targets optic disc myelin sheath Damages bilateral basal ganglia/putamen Clinical: blurred/color vision, “snow-field” vision, blindness, central scotoma, inebriation, ab pain, ARF 2/2 myoglobinuria, pancreatitis, AG met acidosis Blindness is generally permanent Ethanol co-ingestion delays symptoms. Has 10X greater affinity for ADH EtOH >100 mg/dL is protective Osm gap present early but decreases. Vice versa for AG. Tx: No GI decontamination Fomepizole (dosing as above) or ethanol if: MeOH >20 or h/o MeOH ingestion and osmol gap >10 or h/o MeOH + 2 (art pH <7.3, bicarb <20, osmol gap >10) Continue fomep/etoh until MeOH <20 HD if: severe met acidosis or ARF/lyte disturbance or coma/seizure or MeOH >50 mg/dL or vision abnormality Bicarb until pH >7.3 Folinic acid – no trials confirming advantage Isopropyl alcohol (Isopropanol) Metabolized to acetone via ADH Rubbing alcohols, nail polish remover, window cleaner Cause twice the CNS depression of EtOH Death is rare First order kinetics Ketosis without acidosis Clinical: inebriation, acetone odor, miosis MC, ab pain, n/v, hypotension rare, tachy, hypotherm “Pseudo-renal failure” – false elevation of creat with normal BUN due to interference of acetone by the colorimetric method of creat determination Tx: Fomepizole/EtOH NOT indicated HD if hypotensive or level >400 mg/dL ASA/NSAIDS ASA peak therapeutic levels at 2 hrs Protein bound Inhibits cytochrome oxidase Causes uncoupling Ingestion of <150 mg/kg usually benign Prehospital care: Activated charcoal. If assisted BVM, hyperventilate MDAC Q4H until ASA <30 mg/dL If intubated, maintain PCO2 of 35mmHg Maintain glucose >90-100 (peripheral demand of glucose increases in OD) Maintain UOP >2ml/kg/hr If seizures, benzos Urine alkalinization: 2 mEq/kg NaHCO3 then infusion (3 amps + D5W at 1.5-2X maintenance) to keep urine pH >7.5 and until ASA <30 mg/dL or arterial blood pH >7.5 Ensure not hypokalemic because hypoK can cause urinary acidification. Keep K>4.0 HD if: severe CNS symptoms or pulm edema or no improvement with GI decontamination/urine alkalinization or ARF or ASA >90-100 mg/dL ASA Clinical: N/V, ab pain, tinnitus, reversible hearing loss, dyspnea, AMS, hyperpyrexia, tachycardic/pnea, hypotensive, flushing, diaphoresis, petechiae, noncardiogenic pulmonary edema, cerebral edema ASA labs: Initial resp alkalosis followed by AG metabolic acidosis, hypoglycemia, Ferric chloride (FeCl3) test of urine (obtained at least 2 hrs post ingestion), Obtain ASA levels Q2-3H Nomogram useless NSAID Clinical: N/V, ab pain, CNS depression, coma, met acidosis, ARF NSAID tx: supportive, AC, benzos for seizures, HD only if ARF but usually worthless Chronic ASA has increased risk of mortality, CNS symptoms and risk of Noncardiogenic pulm edema Pharmacokinetics and Toxicokinetics Pharmacokinetics – study of behavior of drugs including absorption, distribution, metabolism, excretion (ADME) Pharmacodynamics – relationship of drug concentration to clinical effect Toxicokinetics – study of ADME of a xenobiotic under circumstances that produce toxicity/excessive exposure Xenobiotics – foreign, natural, or synthetic chemicals Toxicodynamics – relationship of toxic concentrations of xenobiotics to clinical effect Absorption – process by which a xenobiotic enters the body rate of absorption (ka) extent of absorption (F) aka bioavailability Rate fastest to slowest: inhalation, IV > IM, SC, intranasal, PO > cutaneous, rectal Fick’s law of passive diffusion: Rate of diffusion = (diffusion constant X surface area X partition coefficient X change in concentration of drug)/membrane thickness pH = pKa + log [A-]/[HA] pH = pKa + log [B]/[BH+] Presystemic elimination can decrease or increase the bioavailability of a drug GI tract microbial organisms can metabolize digoxin, OCPs, insulin and can even convert xenobiotics into poisons (amygdalin into cyanide) First pass metabolism – when drug goes from intestine into venous system directly to liver, avoiding systemic circulation Distribution Volume of distribution (Vd) = [% pure drug (S) X F X dose (mg)]/time zero (Co) A large Vd indicates that the xenobiotic resides outside of the plasma compartment and thus it is unlikely that hemodialysis/hemoperfusion/exchange transfusion would be effective High plasma protein binding limits effectiveness of hemodialysis Albumin binds weak acids (ASA, warfarin, phenytoin) Alpha1-acid glycoprotein binds weak bases (lidocaine, propranolol) Elimination – removal of a parent compound from the body Phase 1 metabolic reactions – (preparative metabolism) introduces polar groups onto nonpolar xenobiotics via oxidation, reduction, or hydrolysis Phase 2 metabolic reactions – (synthetic reactions) conjugates polar groups with a glucuronide, sulfate, acetate, etc. which increases hydrophilicity In first order metabolism, regardless of the concentration of the xenobiotic, the rate of decline is constant. –(dC/dt) = (Vmax/Km) X C In first order, the FRACTION of drug eliminated each hour is the same e.g. 15% of the total remaining concenctration is eliminated each hour Half-life - Time necessary for the xenobiotic concentration to be reduced by 50% Half-life calculations can NOT be determined for zero order kinetics The time to achieve 95% of steady state concentration in a first-order process is dependent on the half life and is usually 5 half-lives. Zero order Vmax = -(dC/dt) In zero order, the AMOUNT of drug eliminated each hour is the same e.g. 150 mg is eliminated each hour (Phenytoin, Warfarin, Heparin, Ethanol, Aspirin, Theophylline) t1/2 = 0.693/Ke Ke = [lnC1 - lnC2]/(t1-t2) Co = (S x F x dose)/[Vd (L/kg) x Wt (kg)] 2Na + BUN/2.8 +Gluc/18 + EtOH/4.6 Hematologic Consequences of Poisoning Erythrocytes Oxidant stress (removal of electrons from molecules) – caused by infection/drugs/food Removal from protein portion of Hgb causes Heinz body hemolytic anemia Removal from iron in Hgb causes methemoglobinemia Removal from porphyrin ring by sulfur causes sulfhemoglobinemia Hexose monophosphate shunt Glucose-6-phosphate is converted to 6-phosphogluconate via G6PD with cofactor NADP+ which becomes NADPH (this maintains glutathione stores needed for oxidant stress) Heinz body hemolysis Oxidation of protein portion of Hgb causes denaturation of Hgb and attachment of protein to RBC internal cell membrane Removed by spleen Causes extravascular hemolysis Arsine, stibine, gasoline, naphthalene cause massive hemolysis Methemoglobinemia Reduced Hgb (ferrous, Fe2+) converted to oxidized Hgb (ferric, Fe3+) Normally <2% Produces functional anemia Shifts oxyhemoglobin curve to left (oxygen unloading becomes more difficult) >10-15% causes cyanosis >20% causes CV and CNS signs/symptoms (HA, dyspnea, tachypnea, tachycard) >40-50% causes lethargy, metabolic acidosis, bradycardia, coma, seizures >70% causes death Anemic patients suffers more severe symptoms at lower fractions Cytochrome-b5 Reductase is responsible for most of MetHgb reduction NADPH MetHgb Reductase normally is inactive but cofactor methylene blue accelerates its activity Many causes: nitroglycerin, benzocaine spray, teething ointments, hemorrhoid creams, lidocaine, phenazopyridine (Pyridium), dapsone, well water, aniline dyes Diagnosis: multiple-wave-length co-oximetry, cyanosis with normal arterial oxygen tension, failure of cyanosis resolution with oxygen, chocolate colored blood Pulse ox not reliable (may produce falsely high or low values) Total Hgb concentration is not affected by presence of MetHgb Tx: O2, check CBC for hemolysis (hgb, blood smear, Heinz body stain, haptoglobin) If asymptomatic, observation If symptomatic, IV methylene blue 2mg/kg (if no h/o G6PD deficiency) Side effects of methylene blue: dysuria, SSCP, tachy, HTN, anxiety, green urine, hemolysis in pts with G6PD deficiency Cimetidine in dapsone overdose Riboflavin in congenital MetHgb Blood/exchange transfusion if refractory to methylene blue Sulfhemoglobinemia Sulfur incorporated into porphyrin ring by oxidant stress SulfHgb persists for the life of the RBC (no conversion back to Hgb) 0.5g/dL causes slate-gray discoloration Shifts oxyhemoglobin curve to right (reduces affinity of hgb for oxygen) Diagnose: Co-oximeter, electrophoresis MCC: phenacetin, sulfonamides, metoclopramide, phenazopyridine, dapsone Tx: supportive. Methylene blue does NOT work. Transfusion if needed Leukopenia – colchicine, benzene, metals, podophyllum, valproic acid Thrombocytopenia – colchicine, arsenic, snake bite Aquatic Envenomations Cnidarians (jellyfish, corals, sea anemones) Envenomate via nematocysts Venom is dermatonecrotic, cardiotoxic, myotoxic, hemolytic, neurotoxic, hepatotoxic Most cause dermal effects and very few cause the other systemic effects Chironex fleckeri (box jellyfish) – causes CV collapse and hemolysis by increasing intracellular Calcium Irukandji syndrome – extreme HTN, pulm edema due to Carukia barnesi jellyfish Tx: Avoid rubbing area (causes nematocyst discharge), vinegar/acetic acid for box, antivenom for life-threatening Chironex, baking soda/papain for Chrysaora (Chesapeake Bay) Stingrays 1-4 spines on dorsum of whiplike tail Tx: place area in hot water, inject lidocaine around area, xray, wound tract exploration Scorpionfish (stonefish, lionfish) Heat labile venom contains hyaluronidase, hemolytic activity, and biogenic amines (NE) Cardiotoxicity due to verrucotoxin (inhibits Ca channels) Tx: place area in hot water, inject lidocaine around area, xray, wound tract exploration, stonefish anti-venom Catfish Spines on dorsal and pectoral fins Hemolytic activity Heat labile toxin Tx: place area in hot water, Tdap, Cipro or 1st generation cephalosporin if infection evident, xray for retained spine Sea Snakes Anterior fangs Neurotoxic venom with neuromuscular blockade Nephrotoxic directly and 2/2 rhabdo Tx: admit for 24hrs obs, antivenom for neuro weakness or muscle necrosis Seabather’s eruption/swimmer’s itch Due to cnidarian larvae trapped btw swimsuit and body Tx: topical steroids, antihistamines Dinoflagellates Ptychodiscus brevis causes red tides Destroyed by wind causing airborn toxin Wheezing, rhinorrhea, lacrimation, sneezing Treat prophylactically with quinolones or Bactrim in immunocompromised patients with aquatic wounds in order to avoid Vibrio infections Insecticides/Cholinesterase Inhibitors/Carbamates/Organophosphate Parathion, Sarin, Tabun, VX gas, Physostigmine Cause rise in Ach at muscarinic (heart, lungs) and nicotinic (skeletal muscle) receptors (Cholinergic Crisis) “Aging” occurs if oxime is not supplied early enough. After ‘aging’, bond is irreversible. Diarrhea, diaphoresis Urination Miosis Bradycardia Bronchosecretions Emesis Lacrimation Lethargy Salivation Due to nicotinic activation at NMJ, may see fasciculations followed by weakness “Intermediate Syndrome” – occurs 24-96 hrs post exposure; follows cholinergic crisis; proximal muscle weakness, cranial nerve palsies, and progression to resp failure; first symptom is weakness of neck flexion Chronic OP exposure – peripheral neuropathies; caused by phosphorylation of lysophospholipase in nerves; vague distal muscle weakness and pain; atropine/pralidoxime does not help Diagnosis: Clinical; cholinesterase activity (butyrylcholinesterase, red cell acetylcholinesterase) Tx: Atropine – competitive antagonist at muscarinic receptors; start at 1-3mg IV; double dose Q5 minutes if response to previous dose is inadequate then start gtt; does NOT affect nicotinic receptors If CNS antimuscarinic toxicity develops, may use glycopyrrolate or scopolamine Pralidoxime – need to give within a few hrs so aging of phosphorylated AChE does not occur; usually does not help in carbamate poisoning but should be given anyway; give 30mg/kg up to 2 g IV then 10mg/kg/h up to 650mg/h Crotalids AKA Pit vipers Triangle heads, elliptical pupils, heat-sensing pits Crotalus – rattles on tails, diamondback, sidewinders Sistrurus – rattles on tails, pigmy rattlesnake Agkistrodon – cottonmouths (water moccasins), copperheads Venom contains multiple substances such as metalloproteinases, collagenase, hyaluronidase, etc. Tissue injury Venom Metalloproteinase (VMP) causes release of TNF alpha Edema, ecchymosis, lymphangitis, LAD Myotoxin-a causes increased intracellular Ca causing skeletal muscle necrosis Coagulopathy Defibrination (depletion of fibrinogen/fibrin) without DIC Rarely DIC Definbrination + thrombocytopenia looks like DIC but does not have microangiopathic hemolysis or organ infarction Thrombocytopenia Cardiovascular toxicity Hypotension due to third spacing Neurotoxicity Rarely weakness and paralysis (Mojave) Myokymia (timber rattler) Compartment syndrome if fang penetrates fascia Tx: Immobilize Elevate extremity NO heat, ice, compression, tourniquet, incision, suction, extraction kits, or electric shock Obtain CBC, fibrinogen, PT/PTT/INR, CK Q4H X24H Antivenin (polyvalent from horse) if: rapid progression of swelling, neuromuscular toxicity, coagulopathy/defibrination/thrombocytopenia, or shock Monitor for anaphylaxis and serum sickness; skin test prior to administration CroFab (polyvalent ovine Fab) – replacing Antivenin; no Copperhead venom used in preparation but may be used in copperhead bites Smoke Inhalation Simple asphyxiants – carbon dioxide Irritant toxins – produce acids, alkalis or ROS; acrolein, ammonia, sulfur dioxide, HCl, chlorine, nitric oxide, etc. Chemical asphyxiants – exert effects at extrapulmonary sites; CO, cyanide Obtain: ABG, carboxyHgb, MetHgb, CXR, co-ox, if lactate >10 then assume cyanide poisoning Tx: supportive, O2, consider treating CO/cyanide, beta-agonists, No steroids Cyanide/Hydrogen Sulfide Cyanide Smoke inhalation, photo developing, Cassava root, nitroprusside Apricots, bitter almond, cherry, peach pits contain amygdalin which is converted to cyanide Combines with MetHgb to make CyanoMetHgb which is converted to Thiocyanate via rhodanese The sulfation of cyanide via rhodanese to thiocyanate is irreversible and is the limiting factor in cyanide detoxification Pathophys: Inhibits cytochrome oxidase, carbonic anhydrase, superoxide dismutase causing a cellular hypoxia and thus despite sufficient oxygen supply, O2 can’t be used Hyperlactatemia occurs due to failure of aerogic energy metabolism Acts as potent neurotoxin at most oxygen sensitive areas (basal ganglia, cerebellum) Directly activates NMDA receptors Acute exposure: HA, anxiety, agitation, lethargy, seizures, coma, N/V, cherry red skin Delayed manifestations of acute poisoning: parkinsonism Chronic exposure: tobacco amblyopia – loss of visual fxn in smokers (bc lower cyanocobalamin) tropical ataxia neuropathy – demyelinating disease (cassava consumers) Leber hereditary optic atrophy – due to rhodanese deficiency Hypothyroidism – thiocyanate is competitive inhibitor of iodide entry Tx: Hydroxycobalamin – central cobalt atom complexes cyanide forming Vit B12; 5g IV; may turn skin red Antidote kit (amyl nitrite, sodium nitrite, sodium thiosulfate) Thiosulfate – donates sulfur atom in rhodanese reaction Nitrite – generates MetHgb; cyanide has higher affinity for MetHgb than oxidase; may turn skin blue Hydrogen sulfide Leather, roofing asphalt, rayon, coke, oil/gas production, manure, volcanoes, caves “rotten eggs” odor Inhibits cytochrome oxidase with higher affinity than cyanide Clinical: “knocked down”, enclosed space, multiple victims, bradycardia, HA, seizures, coma, N/V, conjunctivitis, dyspnea, cyanosis, hemoptysis Tx: Nitrite – MOA similar as in cyanide No role for thiosulfate or hydroxycobalamin Cyclic Antidepressants Inhibit presynaptic reuptake of NE and/or serotonin May cause refractory hypotension (depletion of NE/epi); don’t use dopamine for tx Muscarinic competitive antagonists Causes sinus tachycardia “D” agents have least anticholinergic affect (doxepin, etc.) Amitriptyline has most anticholinergic affect Alpha1 antagonists Postural hypotension Cardiac sodium channel blockade Slow the recovery from inactivation of the fast sodium channel Slows phase 0 depolarization Causes prolonged QRS which can lead to wide-complex tachycardia Right bundle is affected more due to longer refractory period; causes RBBB pattern R-R’ in aVR Rarely causes Brugada pattern Histamine antagonists Agitation, delerium Peak concentrations 2-8 hrs post ingestion Rapidly absorbed so get very sick very fast If asymptomatic/mild symptoms and normal EKG, okay to have psych eval after 6 hours Low blood pH increases the amount of free drug (serves as basis for alkalinization therapy) TCAs are weakly basic so when pH low, they become more ionized which is the state that binds to Na channels NaHCO2 also provides Na which acts competitively at Na Channel Site Tx: If QRS > 100 or R-R’ in aVR >3mm, bicarb at 1-2 mEq/kg boluses If pH <7.35, give bicarb until pH 7.45-7.55 Mildly hyperventilate if intubated If refractory to bicarb, give lidocaine Last ditch with ECMO or intralipid Agents causing Na Channel blockade: TCA Carbamazepine Cocaine Cyclobenzaprine Propoxyphene First generation phenothiazine AP (thioridazine causes DELAYED dysrhythmias) Quinidine/quinine/hydroxycholorquine Propafenone Mushrooms/Plants Cyclopeptide-containing groups Amanita phalloides (death cap) pic 1 Amanita virosa (destroying angel) pic 2 Galerina spp. Pic 3 Lepiota helveola pic 4 Phallotoxin – GI symptoms in initial phase Amatoxin – Inhibits RNA polymerase II preventing transcription Phase I – 6-12 hrs PI, gastroenteritis Phase II – 12-24 hrs PI, transient improvement Phase III – 1-6 days PI, hepatic failure Mgmt (controversial): Thioctic acid, high dose PCN?, cimetidine, AC absorbs toxin, silymarin/silybin (inhibits hepatic uptake of amatoxin) Monomethylhydrazine-containing groups Gyromitra esculenta (false morel) – looks like brain Gyromitrin toxin – undergoes hydrolysis to acetylaldehyde and monomethylhydrazine which inhibits conversion of pyridoxine Onset 6-12 hrs N/V, HA, Seizures, hepatorenal failure Mortality 40% Mgmt: pyridoxine 25mg/kg IV Muscarine-containing groups Clitocybe dealbata (the Sweater) pic 1 Clitocybe clavipes pic 2 Clitocybe illudens (Jack O’Lantern) 3 Inocybe spp. Causes peripheral cholinergic syndrome (no CNS symptoms bc doesn’t cross BBB) Onset 0.5-2 hrs Coprine toxins Coprinus spp, includes atramentarius (Inky Cap) Amino acid metabolized to L-aminocyclopropanol which blocks aldehyde dehydrogenase Disulfiram type reaction if ingested with EtOH Muscimol-containing groups Amanita muscaria, pic 1 Amanita pantherina, pic 2 Ibotenic acid decarboxylated to muscimol Inhibitor of GABA receptor Euphoria, hallucinations, ataxia, dream-filled sleep Severe ingestions with fever, confusion, myoclonus, mydriasis, sz, coma Lasts 6 hrs Mgmt: benzos Hallucinogenic groups Psilocybe spp Gymnopilus spectabilis Psathyrella foenisecii Psilocybin/psilocin indoles similar to LSD Hallucinations, ataxia, sz, hyperkinesis Onset 0.5-3 hrs Mgmt: benzos LBM’s Chlorphyllum molybdites (green parasol), esculentum GI distress in 0.5-3 hrs Orelline-containing groups Cortinarius rainierensis, found in Northwest Bipyridal compounds (orelline and orellanine) similar to paraquat/diquat Renal tubular injury Symptoms delayed 24 hrs Initial gastritis, HA, chills, anorexia then oliguric renal failure in days/weeks Allenic norleucine (breaks rule of early vs late symptoms) Amanita smithiana, found in Northwest Renal tubular/interstitial injury similar to Cortinarius Acute GI 30min-12hr Renal failure days Rhabdomyolysis Tricholoma equestre (man on horseback) Unidentified toxin causes myopathy Nutmeg Nut from evergreen tree Myristica fragans Toxin: myristicin located in the SEED MAOI Metabolized to MMDA N/V, hallucination, hyperthermia, HTN, Tachy Morning Glory Seeds – Contain LSD Pennyroyal oil Volatile oil from Mentha pulegium and Hedeoma pulegoides Toxin: pulegone Direct hepatotoxin Bronchial epithelial cell Neurotoxin Mgmt: consider NAC Chamomile tea Tea brewed from chamomile flower Anaphylaxis Jimsom Weed Contain hyocyamine, scopolamine, atropine Anticholinergic poisoning Pyrrolizidine alkaloids Found in herbal teas Heliotropium (pic), Senecio, Crotalaria Hepatic venoocclusive disease, Hepatomegaly, Hepatic Carcinoma Khat Catha edulis Cathine and cathionine Stimulant effect btw caffeine and amphetamine Chew leaves and stems Absinthe Liquor from wormwood (Artemisisa absinthium) Psychosis, hallucinations, intellectual deterioration Dieffenbachia (Dumbcane) Contains Ca oxalate spear-like crystals packaged into raphides Forceful ejection of crystals into mucous membrane Histamine response Poinsettia (Euphorbia pulcherrima) Minimal GI symptoms Not a significant toxin Holly (Ilex spp.) Contains polyphenols, triterpens, saponins Mild GI symptoms Mistletoe (Phoradendron spp.) Phoradendron flavescens (Christmas Mistletoe in US) Viscum album in Europe Viscum is cardiotoxin (bradycardia, neg inotrope) Inhibits protein synthesis at 60S ribosomal unit All parts of plant are poisonous Jequirty pea/Rosary pea (Abrus precatorius) Used in jewelry as bead Contains toxalbumin abrin A&B protein chains with disulfide linkage B chain binds to cell surface glycoproteins allowing entry A chain inhibits ribosomal protein synthesis Bean must be chewed to be toxic Sz, CNS depression, cerebral edema, dysrhythmias Castor bean (Ricinus communis) Contains toxalbumin ricine (similar to abrin) Seeds must be chewed Severe GE, hemorrhagic gastritis Rhubarb (Rheum rhaponticum) Leaves contain oxalates GI symptoms Solanacea (Nightshade) Potatoes (Solanum tuberosum) Nightshade or European bittersweet (Solanum dulcamara) pic 1 Jerusalem cherry (Solanum pseudocapsicam) pic 2 Horse Nettle or wild tomatoe (Solanum carolinense) Solanine – glycoalkaloid removed by boiling; in buds/stems/shoots N/V, diarrhea, HA, hallucinations, blurred vision Pokeweed (Phytolacca Americana) Mistaken for horseradish Phytolacca: GI irritant Mitogens: lymphocytosis N/V, diarrhea, blurred vision, diaphoresis, weak, Sz, dysrrythmias Colchicine containing plants Autumn crocus (Colchium autumnale) pic 1 Glory Lilly (Glorisosa superba) pic 2 Highest concentration in bulb Antimitotic, binds to tubulin GI then multi-system organ failure with NCPE Cyanogenic plants Prunus spp (apricots, bitter almond, peach, apple, wild cherry) – amygdalin in seeds Hydrangea – in leaves/buds Elderberry Cassava – in tubers not properly prepared (pic) Amygdalin and linamarin or lotaustralin Enzymatic breakdown releasing cyanide Peppers (capsicum) Capsaicin Laryngospasm Mucosal irritant Releases neuropeptide substance p Ackee fruit Unripe fruit contains hypoglycine Similar to Reye Syndrome Hypoglycemia, fatty infiltration of liver, n/v, ams Plants cultivated for flowers Foxglove (digitalis) pic 1 Monkshood, wolfbane (aconitum napellus) pic 2 Aconitum toxin Paresthesias of throat Nausea, salivation, hypotension, dysrhythmias Lantana Lantadene toxin Photosensitization Children poisoned from green berries unripe GI, CNS depression; cholestatic jaundice in livestock Rhododendron spp Toxin: diterpenic polyalcohols (grayanotoxin, asebotoxin, rhodojaponin) Acts as cardiac glycoside, hypotensive, bradycardic, n/v, blurred vision Yew Toxicity from leaves or chewed seed; berries nontoxic Christmas decoration Taxine A&B inhibit Na and Ca currents Oleander Toxin cardiac glycoside All plant parts are toxic Mayapple (Podophyllum peltatum) DNA strand uncoupler GI symptoms Peripheral neuropathy Sz, coma, fever, ileus, ARF, BM suppression Tree tobacco (Nicotiana spp) Nicotine SLUDGE symptoms NMB Deadly nightshade (Atropa belladonna) Toxin hyocyamine Anticholinergic syndrome Poison hemlock (Conium maculatum) Toxin conium Similar to nicotine Buckthorn Unidentified neurotoxin Similar to Guillain Barre Water hemlock (wild carrot, false parsley) All parts toxic CNS stimulant, Sz Strychnine Used as rodenticide Competitive inhibition of glycine at post-synaptic motor neuron receptor in spinal cord “Awake seizures” Cardioactive steroids Digoxin (Foxglove, Oleander, Lily of the Valley, Red Squill, Dogbane; Toad Bufo species) Steroid core with attached lactone ring and sugar group Sugar group confers more water solubility enhancing entry into cells Increase contractility, positive inotrope by increasing cytosolic Ca during systole Dig inhibits Na-K ATPase This inhibits Na extrusion and increases intracellular Na thereby decreasing transmembrane gradient. Since Na-Ca antiporter derives power from the gradient, Ca extrusion from the cell is decreased. This enhances the Ca-induced Ca release from the SR during systole Dig decreases rate of depolarization/conduction through the SA/AV nodes Occurs via vagally mediated parasympathetic tone and by depression of myocardium Reflected on EKG by a decrease in ventricular response rate to suprajunctional rhythms and by PR prolongation. EKG shows QT shortening and ST/T forces opposite in direction to major QRS force (scooping of ST segment) Hypokalmeia enhances effects of digoxin by inhibiting Na-K ATPase activity (decreased competitive inhibition between dig and K at the ATPase) Manifestations of toxicity: Acute: N/V, ab pain, lethargy, confusion, weakness Chronic: anhedonia, loss of appetite, weakness, AMS, seizures rarely, amblyopia, scotomata, photophobia, yellow halos around lights Hyperkalemia – better prognosticator than dig level or EKG changes (keep <5.0) First cardiac sign is usually extopic vent rhythm Bidirectional ventricular tachycardia is diagnostic Indications for DSFab Any dig related life threatening dysrhythmia K >5 Serum dig concentration >15ng/mL at any time or >10 6hrs post ingestion Acute ingestion of 10 mg in adults Acute ingestion of 4 mg in children Chronic elevation of serum dig concentration associated with AMS, dysrhythmias, GI Number of vials = (SDC X pt weight)/100 = (mg ingested x bioavail 0.8)/0.5mg per vial Carbon Monoxide Most Serious complication - delayed neurological sequelae occurs in up to 50% Binds to Hgb at affinity 200-250 X oxygen Causes left shift (decrease in 2,3-BPG) Binds to mitochondrial cytochrome oxidase which causes ischemic reperfusion injury in brain Leads to delayed lipid peroxidation of neurons Only 10-15% of total body CO is extravascular, bound to myoglobin Acute exposure: headache, N/V, dizziness, chest pain, dysrhythmias, ataxia, cherry red skin Early resp alkalosis due to compensation of decreased O2 carry capacity then met acidosis due to lactate COHb normal 0-5% COHb smokers 6-10% Measure with co-oximeter COHb is misinterpreted as oxyHb on most pulse oximeters Measure lactate EKG if chest pain MGMT: 100% oxygen with positive pressure mask/ET (decreases half-life from 5 hrs on RA to 1 hr) HBO decreases half life to 20 minutes (but also decreases lipid peroxidation in pts who have lost consciousness) Use HBO in: syncope (LOC), coma, Sz, AMS, COHb >25%, abnl cerebellar fxn, age >36, prolonged >24hr exposure, fetal distress in pregnancy Use HBO within 6-24 hrs post-exposure (within 6 is better) CCB/BB toxicity Inhibit flow of Ca through L-type voltage sensitive channels but via different mechanisms Ca flux is necessary for pacemaker activity, AV conduction, myo contraction, insulin secretion, vasc tone Stimulation of beta1 receptors on myocytes causes increased intracellular cAMP which causes an increase of Ca flow through L-type channel. Increased intracellular Ca causes Ca release from SR causing contraction of muscle. Dihydropyridines (nifedipine) are potent vasodilators with little effect on heart Non-dihydropyridines (verapamil, diltiazem) effect both heart and vascular tone In BB with membrane stabilizing activity (labetalol, carvediolol, acebutolol, propranolol) may see increased QRS and seizures See hyperglycemia, hyperlactatemia Mgmt: Ca – more specific for CCB but give for both; give lots CaCl – 13 mEq Ca; 0.6ml/kg then infuse CaGluconate – 4 mEq Ca; 1.8 ml/kg then infuse Glucagon – Stimulates adenyl cyclase which increases cAMP; 5-10 mg IV then infuse Side effects: N/V, diarrhea PDE inhibitor (milrinone) – used in Europe Epi/NE High dose insulin if poor heart contractility bc helps with glucose utilization by heart (view with U/S) – 1U/kg bolus then 1U/kg/hr up to 10U/kg/hr; Tolerate K to 2.5 bc whole body K is WNL Lithium Element number 3 Mood stabilizer; used in bipolar disorder Eliminated unchanged; no metabolism Renally excreted Li >2 is high Chronic OD: usually due to adding new drug, dehydration; mental slowing, tremor, ataxia, Sz, heart block, serotonin syndrome, Nephrogenic DI Acute OD: Vomiting, clonus, AMS, Decreased anion gap if very elevated Mgmt: normal saline, HD if: AMS, coma, sz, acute level >4, chronic level >2 Lead Element number 82 Used in saudering, fish weights, paint, bullets, cheap jewelry Usually seen as FB ingestion or “ethnic” red food dyes Usually chronic toxicity Acts like Ca and Fe bc it’s divalent Tremor, ab pain, HTN, encephalopathic, constipation, “Saturnine” gout, multiple myelom If >5, then elevated Inteferes with heme synthesis Mgmt: MVT with Ca and Fe for competitive antagonist If FB, consider EGD for retrieval Fiber diet Xray Chelation if: >40 Succimer preferred, 17 day course BAL (made with peanut oil) EDTA (may cause hypoCa)