References: Motion Analysis Testing
advertisement
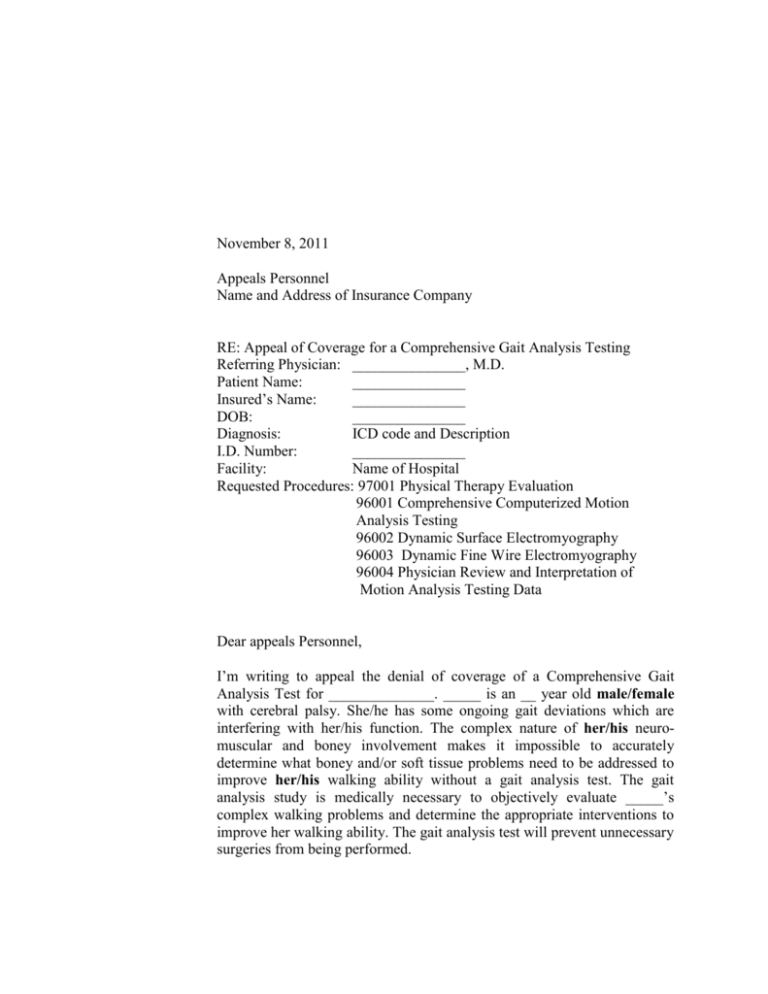
November 8, 2011 Appeals Personnel Name and Address of Insurance Company RE: Appeal of Coverage for a Comprehensive Gait Analysis Testing Referring Physician: _______________, M.D. Patient Name: _______________ Insured’s Name: _______________ DOB: _______________ Diagnosis: ICD code and Description I.D. Number: _______________ Facility: Name of Hospital Requested Procedures: 97001 Physical Therapy Evaluation 96001 Comprehensive Computerized Motion Analysis Testing 96002 Dynamic Surface Electromyography 96003 Dynamic Fine Wire Electromyography 96004 Physician Review and Interpretation of Motion Analysis Testing Data Dear appeals Personnel, I’m writing to appeal the denial of coverage of a Comprehensive Gait Analysis Test for ______________. _____ is an __ year old male/female with cerebral palsy. She/he has some ongoing gait deviations which are interfering with her/his function. The complex nature of her/his neuromuscular and boney involvement makes it impossible to accurately determine what boney and/or soft tissue problems need to be addressed to improve her/his walking ability without a gait analysis test. The gait analysis study is medically necessary to objectively evaluate _____’s complex walking problems and determine the appropriate interventions to improve her walking ability. The gait analysis test will prevent unnecessary surgeries from being performed. The specific reason stated for not covering the comprehensive gait analysis test is that _______________________________________________________(sample: “…the evidence is too limited to draw definitive conclusions regarding the role of gait analysis in the continuum of care”.) This medical policy is outdated and omits the evidence found in the current literature. There are many recent peer-reviewed studies in the literature that document the use of comprehensive gait analysis testing in patients with cerebral palsy improves the outcome of orthopaedic care as well as decreases the cost of care. I urge you to review the more recent literature cited in this letter so that the decision on the needed services is based on the current literature. At the end of this letter you will find an extensive list of research articles published in peer reviewed journals documenting motion analysis testing as the standard of care for individuals with walking problems due to cerebral palsy. Two recent studies not addressed in the denial letter demonstrate the dramatic decrease in costs and the decrease in the need for future surgeries if comprehensive motion analysis testing is done prior to the initial surgery. In 2008 Ounpuu, et al published the results of a study demonstrating the average charges for a single event multilevel surgical approach carried out based on the results of a gait analysis test were close to half of the charges for the same surgeries carried out in a staged approach addressing one problem at a time. In 2009 Wren, et al published the results of a study demonstrating three times more surgeries per person year for ambulatory patients with cerebral palsy who DID NOT have gait analysis testing prior to their initial surgery. In 2011 Wren, et al published a systematic review of the current evidence base related to the efficacy of gait analysis which I strongly urge you to review. Wren, et al also recently completed a 5 year randomized controlled study on the impact of gait analysis on the outcome of care. The findings were presented at NIH in April 2011 and showed that the use of clinical gait analysis prior to orthopaedic surgery in children with cerebral palsy improved their walking ability and their overall health. The alternative to making surgical decisions for _____ based on the gait analysis data is to make surgical decisions based on clinical assessment and visual assessment alone. It is well documented in the literature, that this consistently leads to repeated encounters with surgeries and often recurrence of deformities necessitating repeat surgery (Fabry, Liu, & Molenaers, 1999; J. Gage, 1994). The recent literature also clearly documents better surgical outcomes when gait analysis data is used to determine the surgical plan (Filho, Yoshida, Carvalho, Stein & Novo, 2008). There are also many peer reviewed publications that include long-term patient outcome data that demonstrates its efficacy beyond informal visual analysis of gait abnormalities routinely performed by clinicians. Studies demonstrate long-term patient outcome data at both 5 and 10 years is clearly far superior to the old results (S Õunpuu, DeLuca, Davis, & Romness, 2002; Sylvia Õunpuu, Keggi, Davis, Bell, & DeLuca, 1996). In fact, the need for repeat surgery has been found to be less than 10% in patients followed out over 10 years. Although one could conclude that the delivery of multilevel surgery alone is the cause of these favorable outcomes, this would be incorrect. The ability to evaluate a patient with complex walking problems at multiple levels including pelvis, hip, knee, ankle and foot is made possible only with threedimensional gait assessments. The ability to package surgeries at multiple levels at a single sitting necessitates an appropriate pre operative assessment so that the correct surgical plan can be delivered. The benefits of gait analysis are further emphasized by making comparisons with the “old” literature based on single level surgery in cerebral palsy, which is fraught with over correction, under correction or the need for repeat surgery (Fabry et al., 1999). The overall results of the single staged surgery approach have led to “excessive morbidity and permanent weakness”(J. R. Gage, 2004). As a referral center for complex gait problems we very frequently see unfortunate results of surgeries performed at centers without gait analysis and without an understanding of basic gait principles. As we have had the ability over the past 20 years to evaluate long-term outcomes, we know that our outcomes using gait analysis are far superior. It has also been well established that the informal visual analysis of gait abnormalities, which unfortunately is the standard of care in many locations, is not acceptable. It has been well documented that there is considerable variation in observer agreement for the most common clinical assessment measures (Keenan et al., 2004; Saleh & Murdoch, 1985). As well, evaluations based on clinical assessment of joint range of motion, measure of spasticity, strength, x-rays and visual observation frequently do not correlate with the dynamic findings during a gait analysis (P. DeLuca, Õunpuu, Davis, & Walsh, 1998; McMulkin, Gulliford, Williamson, & Ferguson, 2000; Orendurff, Chung, & Pierce, 1998). This is particularly an issue in those with neuromuscular gait disorders where the impact of abnormal muscle tone increases significantly during functional activities such as gait in comparison to the reclined or sitting positions of the clinical examination. As stated by Lee (E. H. Lee et al., 1992), the “combination of a careful clinical assessment and gait analysis can produce the better results in surgery for children with cerebral palsy”. Several recent studies have demonstrated improved outcomes for individuals with complex walking problems when surgical recommendations, based on findings from threedimensional gait analysis, were followed (F. Chang, 2006; M. Filho, 2008; T. Wren, 2008). Chang, et al evaluated fourteen children with cerebral palsy who had undergone two comprehensive gait analyses spaced at least one year apart. Subjects in the control group were assigned surgical recommendations based on findings from the first gait study, but did not undergo any surgery. The experimental group of children received surgical recommendations based on gait analysis, and then underwent the prescribed surgical procedures. Prior to the surgical procedures for the experimental group, the two groups were matched for identical surgical recommendations based on their initial gait analysis evaluations. The second set of gait analyses were performed one year post-operatively for the experimental group, and one year following the first gait evaluation for the control (no-surgery) group. Findings demonstrated that the control group (those who did not have the prescribed surgical procedures) had only 19.9% positive outcomes, and the experimental group (those who underwent the prescribed surgical procedures) had 46.7% positive outcomes based on post-surgical evaluation criteria. This study illustrates that individuals with complex walking problems have superior outcomes when they undergo the surgical procedures recommended after three-dimensional gait analysis. A more recent study (Filho, et al 2008) demonstrated that the use of three-dimensional gait analysis prior to surgery leads to improved clinical outcomes in children with cerebral palsy. In this study 38 patients with cerebral palsy were divided into four groups according to the agreement between the recommendations from gait analysis and the procedures actually carried out. Fifteen additional patients with cerebral palsy whose surgical intervention was postponed were utilized as the control group. No gait improvement was noted in the control group or in patients whom no procedures recommended by the gait exam were performed. Improvements in walking were observed after treatment in the other three groups with more significant improvements being directly correlated to increased agreement between the motion lab recommendations and the actual treatment carried out. An important positive outcome associated with the use of gait analysis is a reduction in the need for future surgery when comparing patients who underwent three-dimensional gait analysis prior to surgery to those who did not (T. Wren, et al, 2008). This study retrospectively evaluated 756 ambulatory patients with cerebral palsy who underwent lower extremity surgery to improve their walking ability. The need for future surgery was compared between the 578 who had three-dimensional gait analysis testing prior to their initial surgery and the 178 patients who did not have gait analysis testing prior to their initial surgery. After adjusting for GMFCS level, the mean number of additional surgeries per person-year was significantly lower in those who had gait analysis testing prior to their initial surgery. The ability to deliver multilevel surgery and better outcomes is certainly not only a benefit to the patient and their family, but also a benefit to the cost of health care delivery in general. Clearly providing a single hospitalization and recovery period and rehabilitation period is more efficient and cost favorable than the system of 25 years ago. Based on a review of the current literature I am requesting the approval of the Motion Analysis Test for __________. As you can see, the Motion Analysis Test is a critical to determining the most appropriate treatment and surgeries to improve ______’s walking ability and function in the community. Sincerely, ________________, M.D. Name and Address of Referring Physician References: Motion Analysis Testing Articles in bold are recent articles documenting the efficacy of gait analysis testing. Bleck, U. E. (1987). Orthopaedic Management in Cerebral Palsy. Philadelphia: Mac Keith Press. Carollo J.J., Matthews D. (2002). Strategies for clinical motion analysis based on functional decomposition of the gait cycle. Phys Med Rehab Clin N Am, 13:949-977. Chang F., Meininger A.K., Carollo J.J. (2006). Comparison of outcomes in children with cerebral palsy when the recommendations from gait analysis are observed. J Pediatr Ortho, 26(5): 612616. Cook, R. E., Schneider, I., Hazlewood, M. E., Hillman, S. J., & Robb, J. E. (2003). Gait analysis alters decision-making in cerebral palsy. J Pediatr Orthop, 23(3), 292-295. Davids, J. R., Õunpuu, S., DeLuca, P. A., & Davis, R. B. (2004). Optimization of walking ability of children with cerebral palsy. In D. L. Helfet (Ed.), Instructional Course Lectures (Vol. 53, pp. 511-522). Rosemont: American Academy of Orthopaedic Surgeons. DeLuca, P. (1996). The musculoskeletal management of children with cerebral palsy. Pediatric Clinics of North America, 43, 1153-1150. DeLuca, P., Davis, R., Õunpuu, S., Rose, S., & Sirkin, R. (1997). Alterations in surgical decision making in patients with cerebral palsy based on three-dimensional gait analysis. Journal Pediatric Orthopaedics, 17, 608-614. DeLuca, P., Õunpuu, S., Davis, R., & Walsh, J. (1998). Effect of hamstring and psoas lengthening on pelvic tilt in patients with spastic diplegic cerebral palsy. J Ped Orthop, 18, 712-718. DeLuca, P. A. (1991). Gait analysis in the treatment of the ambulatory child with cerebral palsy. Clinical Orthopaedics and Related Research, 264, 5-75. DeLuca, P. A., Õunpuu, S., Rose, S. A., & Sirkin, R. (1993). Surgical decision-making for children with cerebral palsy: conventional versus three-dimensional gait analysis. Paper presented at the Eighth Annual East Coast Clinical Gait Laboratory Conference, Rochester, Minnesota. Esquenazi, A. (1999). Computerized gait analysis for rehabilitation and surgical planning in upper motor neuron syndrome. Europa Medicophysica, 35(3), 111-118. Fabry, G., Liu, X. C., & Molenaers, G. (1999). Gait pattern in patients with spastic diplegic cerebral palsy who underwent staged operations. J Pediatr Orthop B, 8(1), 33-38. Filho M.C., Yoshida R., Carvalho W.S., Stein H.E., Novo, N.F. (2008). Are the recommendations from three-dimensional gait analysis associated with better postoperative outcomes in patients with cerebral palsy? Gait & Posture, 28(2): 31622. Fuller, D. A., Keenan, M. A., Esquenazi, A., Whyte, J., Mayer, N. H., & Fidler-Sheppard, R. (2002). The impact of instrumented gait analysis on surgical planning: treatment of spastic equinovarus deformity of the foot and ankle. Foot Ankle Int, 23(8), 738-743. Gage J.R. (1993). Gait analysis: an essential tool in the treatment of cerebral palsy. Clin Orthop, 288:126-34. Gage, J. (1994). The role of gait analysis in the treatment of cerebral palsy. Journal of Pediatric Orthopaedics, 14, 701-702. Gage, J. R. (1992). Gait Analysis: an essential tool in the treatment of cerebral palsy. Clinical Orthopaedics and Related Research, 288, 126-134. Gage, J. R. (2004). An overview of treatment. In J. R. Gage (Ed.), The treatment of gait problems in cerebral palsy (pp. 238-244). London: Mac Keith Press. Gage, J. R., DeLuca, P. A., & Renshaw, T. S. (1996). Gait analysis: principle and applications with emphasis on its use in cerebral palsy. Instr Course Lect, 45, 491-507. Gage, J. R., & Novacheck, T. F. (2001). An update on the treatment of gait problems in cerebral palsy. J Pediatr Orthop B, 10(4), 265-274. Kay, R. M., Dennis, S., Rethlefsen, S., Reynolds, R. A., Skaggs, D. L., & Tolo, V. T. (2000). The effect of preoperative gait analysis on orthopaedic decision making. Clin Orthop(372), 217-222. Kay, R. M., Dennis, S., Rethlefsen, S., Skaggs, D. L., & Tolo, V. T. (2000). Impact of postoperative gait analysis on orthopaedic care. Clin Orthop(374), 259-264. Kay, R. M., Rethlefsen, S. A., Ryan, J. A., & Wren, T. A. (2004). Outcome of gastrocnemius recession and tendo-achilles lengthening in ambulatory children with cerebral palsy. J Pediatr Orthop B, 13(2), 92-98. Keenan, W. N., Rodda, J., Wolfe, R., Roberts, S., Borton, D. C., & Graham, H. K. (2004). The static examination of children and young adults with cerebral palsy in the gait analysis laboratory: technique and observer agreement. J Pediatr Orthop B, 13(1), 1-8. Kerrigan, D. C., & Glenn, M. B. (1994). An illustration of clinical gait laboratory use to improve rehabilitation management. Am J Phys Med Rehabil, 73(6), 421-427. Kerrigan, D. C., Karvosky, M. E., & Riley, P. O. (2001). Spastic paretic stiff-legged gait: joint kinetics. Am J Phys Med Rehabil, 80(4), 244-249. Krebs, D. E., Edelstein, J. E., & Fishman, S. (1985). Reliability of observational kinematic gait analysis. Phys Ther, 65(7), 1027-1033. Lee, E. H., Goh, J. C., & Bose, K. (1992). Value of gait analysis in the assessment of surgery in cerebral palsy. Arch Phys Med Rehabil, 73(7), 642-646. Lee, E. H., Nather, A., Goh, J. C., Teng, B., & Bose, K. (1985). Gait analysis in cerebral palsy. Annals Academy of Medicine, 14(1), 37-43. Lee, L. W., Kerrigan, D. C., & Della Croce, U. (1997). Dynamic implications of hip flexion contractures. Am J Phys Med Rehabil, 76(6), 502-508. McMulkin, M. L., Gulliford, J. J., Williamson, R. V., & Ferguson, R. L. (2000). Correlation of static to dynamic measures of lower extremity range of motion in cerebral palsy and control populations. J Pediatr Orthop, 20(3), 366-369. Nene, A., Evans, G., & Patrick, J. (1993). Simultaneous multiple operations for spastic diplegia. Journal of Bone and Joint Surgery, 75-B, 488-494. Novacheck, T. F. (1996). Surgical intervention in ambulatory cerebral palsy. In G. F. Harris & P. A. Smith (Eds.), Human motion analysis: Current applications and future directions (pp. 231-254). Piscataway: IEEE Press. Orendurff, M. S., Chung, J. S., & Pierce, R. A. (1998). Limits to passive range of joint motion and the effect on crouch gait in children wth cerebral palsy. Gait & Posture, 7(2), 165. Õunpuu, S. (2002). Gait Analysis in Orthopaedics. In R. Fitzgerald, H. Kaufer & A. Malkani (Eds.), Orthopaedics (pp. 86-107). St. Louis: Mosby. Õunpuu, S. (2003). Gait analysis in documenting and understanding hip function. In J. V. Banta & D. Scrutton (Eds.), Hip disorders in childhood (pp. 146-162). London: Mac Keith Press. Ounpuu S, Bell K, DeLuca P. (2008). The “Birthday Syndrome” vs. the single event multilevel surgical approach: a comparison of financial costs. Preceedings of the 13th Annual Gait and Clinical Movement Analysis Society, 2008, 160-161. Õunpuu, S., DeLuca, P., Davis, R., & Romness, M. (2002). Long-term effects of femoral derotation osteotomies: an evaluation using three-dimensional gait analysis. Journal of Pediatric Orthopaedics, 22, 139-145. Õunpuu, S., Keggi, J. M., Davis, R. B., Bell, K. J., & DeLuca, P. A. (1996). A long-term followup of the effects of heel cord surgery on the ankle in persons with cerebral palsy. Patrick, J. H. (2003). Case for gait analysis as part of the management of incomplete spinal cord injury. Spinal Cord, 41(9), 479-482. Perry, J. (1999). The use of gait analysis for surgical recommendations in traumatic brain injury. J Head Trauma Rehabil, 14(2), 116-135. Rang, M. (1990). Cerebral Palsy. In R. Morrissy (Ed.), Lovell and Winter's Pediatric Orthopedics (Vol. 1, pp. 465-506). Philadelphia, PA: JB Lippincott. Rethlefsen, S., Dennis, S., Kay, R., (2008). Impact of gait analysis on treatment planning for intoeing and out-toeing in able bodied subjects. Proceedings of the 13th GCMAS Meeting, 310-311. Saleh, M., & Murdoch, G. (1985). In defence of gait analysis. Observation and measurement in gait assessment. J Bone Joint Surg Br, 67(2), 237-241. Saraph, V., Zwick, E. B., Zwick, G., Steinwender, C., Steinwender, G., & Linhart, W. (2002). Multilevel surgery in spastic diplegia: evaluation by physical examination and gait analysis in 25 children. J Pediatr Orthop, 22(2), 150-157. Schwartz, M. H., Viehweger, E., Stout, J., Novacheck, T. F., & Gage, J. R. (2004). Comprehensive treatment of ambulatory children with cerebral palsy: an outcome assessment. J Pediatr Orthop, 24(1), 45-53. Wren T.A.L., Gorton G.E., Ounpuu S., Tucker, C.A. (2011). Efficacy of clinical gait analysis: a systematic review. Gait and Posture, 34(2), 149-153. Wren T.A.L., Kalisvaart M, Ghatan C, Rethlefsen S.A., Hara R., Sheng M., Chan L.S., Kay R.M. (2009). Effect of pre-operative gait analysis on costs and amount of surgery. J Pedriatr Orthop. 29, 558-563, 2009. Wren T.A.L., Otsuka N.Y., Bowen R.E., Scaduto A.A., Chan L.S., Rethelefsen s S.A., Healy B.S., Dennis S.W., Kay R.M. (2011). Impact of gait analysis on surgical outcomes: preliminary results from a randomized controlled study. Proceedings of the 16th GCMAS Meeeting. Zwick, E. B., Saraph, V., Strobl, W., & Steinwender, G. (2001). [Single event multilevel surgery to improve gait in diplegic cerebral palsy - a prospective controlled trial]. Z Orthop Ihre Grenzgeb, 139(6), 485-489.