CNA Medical Form - Manchester Community College
advertisement

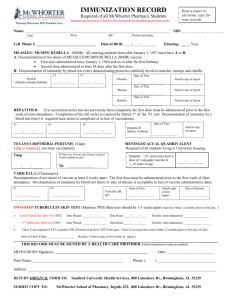
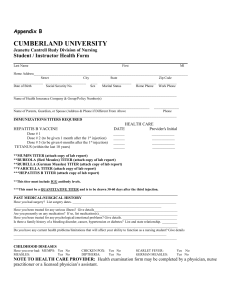
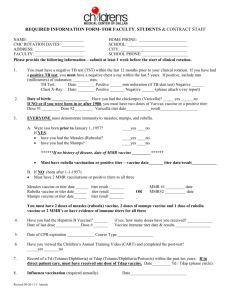
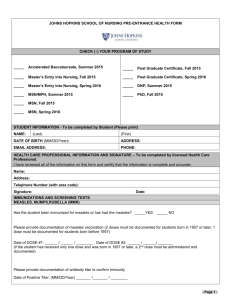
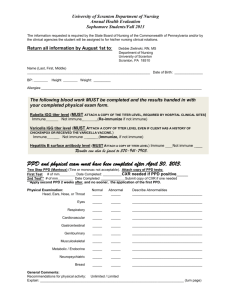
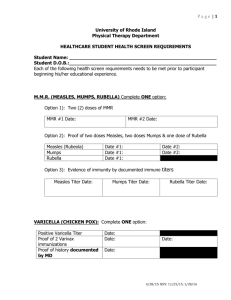
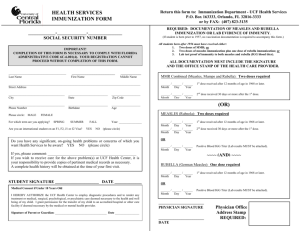
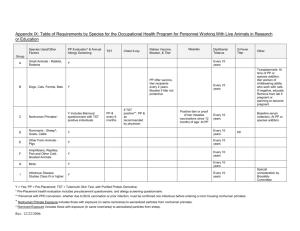
CERTIFIED NURSE AIDE STUDENT HEALTH RECORD PART I - to be completed by Student Name _____________________________________________________________ Date ________________________ Street __________________________________________________________________________________________ City ___________________________________________________ State ____________________ Zip____________ Home Phone ____________________________ Cell __________________________________ Date of Birth ____________________________ Male Female PART II- to be completed by Health Care Provider Physical Assessment: Height _____________ Weight ____________ Date Completed _______________________ BP ____________ P __________ T ___________ R ________ Allergies ________________________________________________________________________________________ _______________________________________________________________________________________________ _______________________________________________________________________________________________ Medications _____________________________________________________________________________________ _______________________________________________________________________________________________ _______________________________________________________________________________________________ Pertinent Past Medical/Surgical History (include impairments and work restrictions) ____________________________ _______________________________________________________________________________________________ _______________________________________________________________________________________________ Head/ENT _______________________________________________________________________________________ Cardiac _________________________________________________________________________________________ Lungs __________________________________________________________________________________________ GI _____________________________________________________________________________________________ Musculo/Skeletal _________________________________________________________________________________ Genito/Urinary ___________________________________________________________________________________ Skin ____________________________________________________________________________________________ Comments _______________________________________________________________________________________ _______________________________________________________________________________________________ _______________________________________________________________________________________________ _______________________________________________________________________________________________ EW 4/13/2010 Continued on reverse Student Name______________________________________________ PART II- to be completed by Health Care Provider (cont’d) Immunization Verification Certificate A. Purified Protein Derivative (PPD) Please provide documentation of a Mantoux skin test for tuberculosis within the previous twelve (12) months, including the date done and size of reaction. For those with a previous positive reaction, documentation attesting to the fact that the individual is not infectious along with any prophylaxis used and the date and size of reaction must be provided by a physician. Performed within the previous 12 months (A tine test is not acceptable.) ............................................... (Date) ________________ Result __________________________________________________________________________________________________ If Mantoux is positive, report of current chest X-ray (within 12 months) ..................................................... (Date) ________________ Result __________________________________________________________________________________________________ B. Rubella (German Measles) Patient has had at least one dose of rubella vaccine, given on or after the first birthday, or serological evidence (blood test) of immunity to rubella, regardless of the age or job status of the person. 1st Dose: (Date) _______________________ __________ 2nd Dose: (Date) _____________________________________ or Immune Titer: (Date) ______________________________ A copy of the lab results for titer tests must be included. C. Rubeola (Measles) Attach written evidence of two doses of live measles vaccine or serological evidence (blood test) of immunity. One dose should have been given on or after the first birthday, and at least one dose should have been given after 1968. The two doses should be separated by at least 30 days. 1st Dose: (Date) _______________________ __________ 2nd Dose: (Date) _____________________________________ or Immune Titer: (Date) ______________________________ A copy of the lab results for titer tests must be included. D. Varicella Zoster (Chickenpox) Patient has had clear history of having had chickenpox .......................... (Date) ________________ or Vaccine Administered ............................................................................................................................ (Date) ________________ or Immune Titer: (Date) ______________________________ A copy of the lab results for titer tests must be included. E. Hepatitis B Patient has completed a vaccination series or has signed a declination statement. 1st Dose ..................................................................................................................................................... (Date) ________________ 2nd Dose .................................................................................................................................................... (Date) ________________ 3rd Dose ..................................................................................................................................................... (Date) ________________ Declination statement (please attach) ................................................................................................................. F. Tetanus Booster within past ten (10) years recommended not required. Received tetan (Date) G. Influenza vaccine (flu shot) within current flu season: The above-named individual has been examined by this office and found to be free of any communicable diseases and physically able to participate in lifting, moving and bathing patients in the Certified Nurse Aide Program at Manchester Community College. NOTE: Immune Titer – A copy of the lab results for titer tests must be included. Name of Physician/Clinic _______________________________________________________________________________________ Address ___________________________________________________ City _______________ State ___________ Zip ___________ Phone ___________________________________________________ Fax ______________________________________________ Signature of Physician _____________________________________________________ Date ____________________ EW, 4/13/2010 p2