Supplement Expanded Methods Study design RALI
advertisement

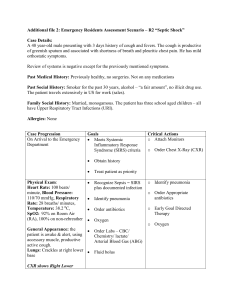
Supplement Expanded Methods Study design RALI-DHF was a prospective, single-center, randomized, double-blind, placebo-controlled proof-of-concept study (NCT01163734, EudraCT 2009-017168-17) funded by a scientific grant from Gilead (Foster City, CA, USA). The trial was approved by the local ethics committee and by the German Federal Institute for Drugs and Medical Devices BfArM. Patients with clinical symptoms of heart failure (NYHA class II-III) undergoing cardiac catheterization as part of the routine diagnostic procedure for standard care were screened for inclusion into the study. Inclusion criteria consisted of LVEF≥45%, E/E′>15 or NT-proBNP>220pg/mL at screening and, as continued eligibility criteria, average resting LVEDP≥18 mm Hg, as well as resting time-constant of relaxation (tau) ≥50 ms at time of cardiac catheterization.1,2 Study conduct and procedures Administration of the study drug was performed in a 1.5:1 ratio (ranolazine vs. placebo). The study treatment began with an intravenous bolus injection of 92 mg (in 10 mL over 2 minutes). A second bolus injection of 92 mg was administered 15 minutes thereafter. Continuous infusion of ranolazine or placebo at a dose of 92 mg/hour (23 mL/hour) was started 5 minutes after the start of the second bolus injection and continued for 24 hours. This dosing regimen was designed to achieve and maintain a therapeutic target ranolazine plasma concentration of ~2500 ng/mL (average concentration achieved by oral dose of 1000 mg twice daily) at the time of post-baseline measurements i.e., 30 minutes after the start of the initial bolus injection. One hour prior to the end of the 24-hour infusion, patients were started on oral study drug 1000 mg (extended release tablets, 2 x 500 mg) twice daily and continued until the end of the study on day 14 (Fig. 1a of the main paper). To assess pharmacokinetic (PK) parameters, PK blood samples were drawn at 10, 20, 30 minutes, and 22 hours after start of intravenous study drug administration. Invasive hemodynamic measurements were initially performed before the first intravenous bolus of study drugs. Pacing was then performed at 120 beats per minute for better comparison between patients and hemodynamic and pressure measurements were 1 again collected.3 These measurements were repeated 30 minutes after the initial intravenous bolus administration at both resting and paced conditions. Three measurements were taken at each time and averaged. Hemodynamic parameters were assessed during rest and pacing for two reasons: First, the goal was to further impair diastolic filling and secondly, we wanted to exclude differences in heart rate as a confounder. Tissue Doppler echocardiography was performed at before catheterization, repeated 60 minutes prior to administration of oral study drug, and at the end of study (Day 14). Cardiopulmonary exercise test (CPET) was performed at baseline and on Day 14. The 12-lead ECG was collected at baseline, prior to start of oral study drug, and at Day 14. Patients were asked to return to the clinic for the End of Study visit on Day 14 (±2 days). The End of Study visit procedures were performed within 2-6 hours after the morning dose. The following key assessments were performed: Complete physical examination including vital signs and weight measurements, 12-lead ECG, echocardiography (prior to CPET), NT-pro-BNP determination and safety labs, CPET, adverse events and concomitant medications. Endpoints The exploratory endpoints were: i) change from baseline to 30 minutes in hemodynamic parameters at both resting and paced conditions including LVEDP, dP/dtmin, tau (derived from a mono-exponential pressure decay fit),3 and ii) change from baseline to Day 14 in echocardiographic parameters including E/E´, CPET parameters including VO 2max, and NTpro-BNP. Statistical considerations The safety analysis set included all patients who received at least one dose of study medication. The full analysis set (FAS) included all patients in the safety analysis set who had at least one post-baseline efficacy measurement. Exploratory efficacy endpoints were analyzed using the FAS, and safety analyses were performed on the safety analysis set. One patient, who was randomized to the ranolazine treatment group and received ranolazine intravenous infusion, was erroneously dispensed placebo tablets. This patient was included only in the 30 minutes and 2-hour time points for analyses of exploratory endpoints, but was included in all safety analyses, both in the ranolazine group. 2 Between-treatment comparisons of all exploratory efficacy endpoints were analyzed using the Wilcoxon rank sum test. Within-treatment comparisons were analyzed using the Wilcoxon signed rank test. Change from baseline was analyzed. Due to the exploratory nature of this study, there were no multiplicity adjustments when testing exploratory endpoints. Therefore, p-values need to be interpreted with caution. Data are presented as mean±SEM. Supplemental Table Parameter LVEDP [mmHg] LVESP [mmHg] PCWP [mmHg] mPAP [mmHg] sPAP [mmHg] dP/dt min [mmHg/s] Tau [ms] t relax [ms] SVR [dyn*s*cm-5] PVR [dyn*s*cm-5] CO [l/min] dP/dt max [mmHg/s] t sys [ms] t sys [%] t dias [ms] stroke vol [ml] Placebo Baseline 30 min 17.7±3.5 14.3±2.3 137.5±12.3 140.9±11.0 19.0±4.4 17.5±3.5 30.2±4.0 28.6±3.9 38.7±5.3 37.3±4.8 -1807.5±134.2 -1851.0±115.7 59.5±2.9 60.7±3.9 165.7±14.2 165.0±12.7 2086.6±273.3 2401.4±336.0 209.5±36.4 224.3±44.2 5.2±1.0 4.8±1.0 1741.1±146.4 1765.4±134.4 234.9±31.6 237.4±21.0 44.2±5.8 44.3±4.7 486.1±23.8 484.0±22.0 46.4±9.3 42.9±9.1 P -value 0.03 0.22 0.41 0.31 0.23 0.64 0.55 0.95 0.04 0.46 0.15 0.95 0.92 0.46 0.95 0.14 Ranolazine P -value P -value Baseline 30 min Plac vs Ran 14.7±2.1 11.0±1.15 0.02 0.97 141.1±7.8 135.7±6.9 0.63 0.30 14.2±2.1 12.3±1.4 0.12 0.80 26.5±2.7 25.2±2.5 0.02 1.00 36.6±3.7 35.3±3.4 0.05 1.00 -2030.8±97.2 -2013.8±84.1 0.90 0.60 52.1±2.6 53.6±2.6 0.07 0.54 133.3±4.9 140.4±5.55 0.01 0.43 1760.9±133.5 1915.5±118.6 0.01 0.21 196.0±10.8 235.5±17.7 0.06 0.71 4.9±0.2 4.3±0.2 <0.01 0.39 2024.1±167.7 1706.2±74.3 0.01 0.04 236.1±15.9 238.2±14.2 0.53 0.84 46.6±3.7 44.9±2.6 0.24 0.54 472.1±21.0 475,09⁺₋21,69 0.32 0.71 42.4±2.1 37.5±2.3 <0.01 0.39 Hemodynamic parameters during catheterization at paced conditions (120 beats per minute). LVEDP=Left ventricular end-diastolic pressure, LVESP=Left ventricular end-systolic pressure, PCWP=Pulmonary capillary wedge pressure, mPAP mean pulmonary arterial pressure, sPAP=systolic pulmonary arterial pressure, tau=time constant for relaxation, t relax=time for relaxation, SVR=systemic vascular resistance, PVR=pulmonary vascular resistance, CO=cardiac output, t sys=time in systole, t dias=time in diastole, stroke vol=stroke volume. All values are mean±SEM. P-value compares baseline vs. 30 min. P-value Plac vs. Ran compares 30 min values between groups. REFERENCES 1. Paulus WJ, Tschöpe C, Sanderson JE, et al. How to diagnose diastolic heart failure: a consensus statement on the diagnosis of heart failure with normal left ventricular ejection 3 fraction by the heart failure and echocardiography associations of the European Society of Cardiology. Eur Heart J 2007;28:2539–50. 2. Massie BM, Carson PE, McMurray JJ, et al. Irbesartan in patients with heart failure and preserved ejection fraction. N Engl J Med 2009;359:2456–67. 3. Wachter R, Schmidt-Schweda S, Westermann D, et al. Blunted frequency-dependent upregulation of cardiac output is related to impaired relaxation in diastolic heart failure. Eur Heart J 2009;30:3027–36. 4