File - Rachael Woods
advertisement

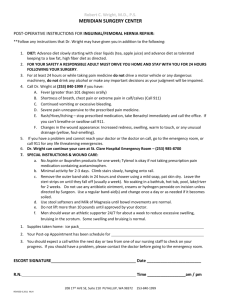
Rachael Woods Major Case Study: Heart Failure and Left Ventricular Assist Device as a Destination Therapy January 17th, 2014 Figure 1.1 (1) Introduction: A.S. is a 71-year-old Caucasian male who weighs 113.90 kg (250.6 lb) and has a height of 182.88 cm (72in). A.S. was admitted for a left ventricular assist device (LVAD) placement as a destination therapy treatment for congestive heart failure class III, stage IV. A.S. was chosen for this study because his case was intriguing; few dietitians are familiar with LVAD therapy and the associated nutritional implications. This study began on December 5th, 2013, and ended on December 20th, 2013. The objective of this study is to closely examine the nutritional requirements for patients who plan to undergo and who have undergone LVAD procedures as a destination therapy. Social History: A.S. is currently retired. Prior to retirement, A.S. owned a business in Wisconsin before moving to Florida 24 years ago, where he worked for an automobile company dealing with parts and services. A.S. is married and has two daughters, ages 42 and 44. A.S. is a devout Catholic. When asked what A.S.’s family responsibilities are he replied with a laugh “laundry and grocery shopping”. A.S. is very active in his 55 and up community, with a passion for politics. A.S. used to be a smoker (quit 20 years ago) and drinks alcohol one to two times per month. 1 Normal anatomy/physiology of affected organs: The heart is a component of the cardiovascular system that consists of arteries, capillaries, and veins (2). Figure 1.2 illustrates the anatomy of the cardiovascular system. Figure 1.2 Anatomy of the heart (3) The heart is a muscle responsible for pumping more than 6,000 liters of blood throughout the body every day (4). The heart is composed of four different chambers, the right atrium, the right ventricle, the left atrium, and the left ventricle (2). Deoxygenated blood (denoted blue in Figure 1.2) enters the heart through the right atrium via the superior vena cava and the inferior vena cava (2). The contraction of the right atrium allows the blood to move from the right atrium into 2 the right ventricle, and the contraction of the right ventricle pumps blood through the pulmonary artery into the lung tissues allowing oxygenation of blood (2). Oxygenated blood (denoted red in figure 1.2) is returned from the lungs to left atrium of the heart via the pulmonary vein. Similar to the right atrium, the contraction of the left atrium allows the movement of blood into the left ventricle. The contraction of the left ventricle pumps oxygenated blood into the aorta, which provides blood to the entire body (2). Cells comprising the body’s tissues and organs use oxygenated blood to provide the fuel for metabolism; deoxygenated blood is returned to the heart via the veins and the process continues. “Heart failure occurs when the heart is unable to pump blood at the rate sufficient to meet the metabolic demands of the tissues or can only do so at an elevated filling pressure”(4). There are many different factors that can lead to heart failure; the three most common are coronary artery disease, high blood pressure, and diabetes (5). Although the aforementioned factors are the most common there are other possible causes as well including: cardiomyopathy (heart muscle disease), heart valve disease (complications secondary to events such as myocardial infarctions), arrhythmias, and congenital defects. When the heart loses its capability to pump efficiently, it comes up with alternative mechanisms to compensate for its losses. The following are three different mechanisms the heart uses to adapt to insufficient function: 1. Frank-Starling mechanism: increased filling volumes (of blood) enlarge the heart and increase cross bridge formation of muscle cells of the heart, which increases contractility (4). 3 2. Hypertrophy: Heart muscle cells (sarcomeres) proliferate to increase muscle size and enhance force of contractility. Enlarged hearts secondary to hypertrophy require additional oxygen consumption to support the demands of additional muscle tissue; therefore hypertrophied hearts are more susceptible to deterioration (4). 3. Activation of neurohormonal systems: (three different mechanisms) a. Norepinephrine increases heart rate and allows for greater contractility and vascular resistance and thus increases blood pressure (4) b. Activation of the renin-angiotensin-aldosterone system, which allows for increase water retention and thus increases blood pressure (4) c. Release of natriuretic peptide (4) Heart failure is categorized into four different stages and four different classes. The stages and classes are provided below in Tables 1.1 and 1.2. Table 1.1 American Heart Association Stages of Heart Failure (6) Presence of heart failure risk Stage A High Risk factors but no heart disease and no symptoms Heart disease is present but there are no symptoms Stage B Asymptomatic (structural changes in heart before symptoms occur) Structural heart disease is Stage C Symptomatic present and symptoms have occurred Presence of advanced heart disease with continued heart Stage D Advanced Disease failure symptoms requiring aggressive medical therapy 4 Table 1.2 Classes of Heart Disease according to the New York Heart Disease Association (7) No limitation of physical activity. Ordinary physical Class I Mild activity does not cause undue fatigue, palpitation, or dyspnea (shortness of breath) Slight limitation of physical activity. Comfortable at rest but Class II Mild ordinary physical activity results in fatigue, palpitation, or dyspnea Marked limitation of physical activity. Comfortable at rest, Class III Moderate but less than ordinary activity causes fatigue, palpitation, or dyspnea Unable to carry out any physical activity without Class IV Severe discomfort. Symptoms of cardiac insufficiency at rest. If any physical activity is undertake, discomfort is increased Heart failure can manifest as left-sided heart failure, right-sided heart failure, or both simultaneously. Left-sided heart failure can be attributed to ischemic heart disease, hypertension, aortic and mitral valve diseases, and myocardial disease (4). As with any disease, symptoms of left-sided heart failure worsen as the disease progresses, Figure 1.3 on the following page illustrates the progression of symptoms. Right-sided heart failure is most always caused by the progression of left-sided heart failure; only in rare cases is there “pure” right-sided heart failure (usually when patients have rare disorders involving the lungs) (4). 5 Figure 1.3 The Progression of Heart Failure Symptoms (4) Decreased cardiac output Decreased O2 delivery/perfusion Cerebral hypoxia, can lead to irritability, loss of attention span, restlessness, and coma & death Orthopenea, (dyspnea when laying down) paroxysmal noctural dyspnea (severe form occuring at night) Reduction in renal perfusion: activates renin-angiotensinaldosterone system: retaining sodium and fluids Perivascular and interstitial edema, worsening pulmonary edema Past Medical History: Past medical history of A.S. includes: congestive heart failure (heart failure) class III, stage IV, cardiomyopathy, coronary artery disease, chronic kidney disease, throat and prostate cancer with radiation, hypertension, gastritis, atrial fibrillation, right bundle branch block, ischemic heart disease, history of myocardial infarction. Surgeries performed prior to this admission include: pacemaker placement and stented coronary artery. Other information related to previous hospital admissions were not documented. 6 Present Medical Status and Treatment: There are numerous ways that heart failure can be treated. According to the National Heart, Lung, and Blood Institute, heart failure can be treated by following a heart healthy diet (such as the TLC diet), physical activity, medications, and surgeries such as pacemaker implantation, implantable cardioverter defibrillators, coronary artery bypass grafts, LVADs, and heart transplants (5). Of the above treatments, A.S. followed a heart healthy diet, took medications, and received an LVAD implantation. Prior to admission, A.S. felt very lethargic, was experiencing shortness of breath, and was not able to perform his normal daily activities. The cause for A.S.’s lethargy was his hearts inability to pump blood effectively throughout his body. When the heart is unable to pump blood through the body effectively, oxygen and essential nutrients cannot be delivered to the organs, tissues, and cells of the body. When the cells comprising tissues and organs are not able to get the oxygen and nutrients they need from the blood, they are not able to carry out their normal functions and so they become compromised, leaving the affected individual feeling ill and tired. Shortness of breath and fatigue can also be caused by fluid retention around the heart and the lungs. When blood becomes congested in the heart it results in systemic venous pressure that can lead to widespread edema; excessive fluid retention can cause pulmonary edema, which makes it difficult for those affected by the disease to breathe (8). Laboratory values are an essential component to any medical examination, as abnormalities are not always externally visible. Throughout A.S.’s stay, lab values 7 related to A.S.’s electrolytes, glucose levels and renal function were closely monitored for trends. Unfortunately, A.S. was not seen for the purpose of this study before he had his LVAD placement and so possible fluctuations prior to surgery could not be monitored. Tables 1.4 and 1.5 show some of A.S.’s abnormal lab values throughout his admission, with the reference ranges denoted in parenthesis (9). Table 1.4 Laboratory findings (12/5) Electrolytes K: 3.3 (3.6-5 mEq/L) Glucose 124 (70-99 mg/dL) BUN, Creatinine WNL Table 1.5 Laboratory findings (12/16) Electrolytes Cl: 94 (101-111 mEq/L) Glucose 94 (70-99 mg/dL) BUN, Creatinine 32(5-20 mg/dL); 1.48(0.6-1.2 mg/dL) Glucose can be elevated during times of stress and while taking certain medications (such as steroids) (10). Stress is most likely the cause for elevated blood glucose in A.S., as he does not have a history of diabetes and was not receiving steroids during the time that the above labs were drawn. Potassium, BUN, and Creatinine can be elevated secondary to renal disease (9). This is most likely the reason for A.S.’s 8 elevated BUN and Creatinine as he has a history of chronic kidney disease. The last lab on the above tables that was out of range was Chloride. Chloride can be low for many different reasons including heart failure (11). Chloride being decreased secondary to heart failure is most likely the case for A.S. as his primary reason for admission to the hospital was for treatment of heart failure via LVAD therapy. As mentioned previously, medication therapy plays a large role in controlling congestive heart failure. It is important to note how medications interact with the body, with each other, and how they affect nutrition status. A.S. was on many different medications throughout his hospital stay. The medications that A.S. received during the days of this study are listed in appendix 1. Observable physical and psychological changes: The first time A.S. was seen for the purpose of this study was about two and a half weeks post-op of his LVAD placement (surgery was on November 19th, and he was first seen for study on December 5th); A.S. was not ambulating and appeared to be very tired and frail. His wife was present in the room and was able to assist with the interview process. Throughout A.S.’s stay at the hospital, his physical and psychological changes were evident; with each visit, his physical and mental status greatly improved. The second time A.S. was seen, he was able to answer all of his questions himself, and was ambulating. As the visits continued, A.S. became more talkative and began telling more personal stories about his life; such as the hardships he faced struggling with heart failure until he had the LVAD placement, rather than just talking about his eating patterns. 9 Treatment: A.S. was admitted to have a surgical procedure performed: LVAD placement. While some individuals receive LVAD treatment as a bridge to heart transplantation, others such as A.S. receive LVADs as a destination therapy. LVADs are used as a destination therapy in patients who are not candidates for heart transplantation. Because A.S. received the LVAD implant as a destination therapy, the purpose of the treatment was to prolong his survival and enhance his quality of life (12). Medical Nutrition Therapy: Nutrition History: A.S. monitors his fat and sodium intake at home, but does not follow any particular diet. A.S.’s wife does the grocery shopping and typically prepares dinner. He and his wife go out to dinner one to two times per week. On a typical day, A.S. eats cereal for breakfast at around 9:00 am. A typical lunch for A.S. is an unspecified sandwich, hot dog, or peanut butter and jelly sandwich at around 1:30 pm. A typical dinner for A.S. consists of turkey breast, meatloaf, chicken, hamburgers, or pizza if he and his wife go out to dinner. A.S. eats all of his meals at his dining room table (not in front of the television although the television can be seen from the table). A.S. participated in a Weight Watchers diet about one year ago and reported that he successfully lost 55 pounds. During the first visit of the study with A.S., a 24-hour recall was performed. Table 1.6 lists the foods as recalled by A.S. and the nutritional breakdown of each. 10 Table 1.6 24-hour recall Food Product Kcals Carbohydrate Protein Fat Ensure Plus 350 kcals 15g 13g 11g Pudding 140 kcals 24g 4g 4g Jello 64 kcals 16g 1g 0g Ensure Plus 350 kcals 13g 51g 11g 0 kcals 0g 0g 0g 904 kcals 68g 69g 26g Diet Tea Total During the visit at which the 24-hour recall was performed, A.S. was on a full-liquid diet. A.S. was not very receptive to this diet order; consuming just 25% and reporting a lack of interest in the foods he was being served. The diet was prescribed because A.S. was intubated four days prior and was receiving enteral nutrition during his intubation. The general protocol for diet advancement post enteral nutrition is to progress from clear liquid to full liquid to solid foods (9). Although many practitioners use the progression from clear liquids to full liquids to solid foods, there is currently not any scientific literature stating that solid foods cannot be initiated as soon as the gut is functioning and tolerating some liquids (9). During the first visit, A.S.’s nutrition problem was diagnosed as inadequate protein energy intake related to decreased ability to consume sufficient protein energy as evidenced by intake less than recommended needs. This diagnosis was 11 formulated on the premises of the full liquid diet that was only fractionally consumed. The caloric needs for those with heart failure are as follows (8): Basal energy expenditure calculated using the Harris-Benedict Equation Add to basal value an additional 15%-25% for minimal physical activity Add another 10%-20% for hypermetabolism of severe heart failure Determine carbohydrate (40%-60%), protein (10%-15%), and fat (30%-40%) adjust based on concurrent conditions Major surgery or sepsis increases energy requirements by 20%-50% Based on the above criteria A.S.’s estimated energy needs during the visit on December 5th were 3,200 kcals: (BEE =2050kcals + 20% for minimal activity = 2500 + 10% for hypermetabolism = 2700 + 20% for surgery= ~ 3200 kcals/day and 80120g protein/day). The hospital that housed A.S. used a different method for calculating caloric and protein needs but still obtained similar results (used kcal/kg method using adjusted body weight). Based on A.S.’s estimated caloric and protein needs and the information provided by A.S.’s intake from his 24-hour recall, A.S. was not consuming enough kcals or protein to meet his needs which is why the aforementioned nutritional diagnosis was made. Formal education in the form of written literature was not given to A.S. during the first visit of this study, however verbal information was given. The importance of adequate calories and protein consumption for wound healing was 12 discussed. The topic of fat, sodium, and fluid restriction were not discussed at the time because A.S. was on a full liquid diet. Eventually A.S.’s diet was advanced to a Solid Regular Coumadin/Warfarin Cardiac diet with Wolk Shake supplements three times a day, and this was observed during the second visit of this study. A.S. was much more receptive to this diet than the previously prescribed diet consuming 100%. The purpose of this diet was to limit the amount of fat, sodium, and vitamin K A.S. was receiving. The cardiac diet is used in the clinical setting to manage symptoms of hypertension and fluid retention secondary to diseases associated with the heart (13). A.S. was also on a vitamin K monitored diet because he was receiving Coumadin. Vitamin K assists in blood coagulation and so the dosage of Coumadin and vitamin K consumption must be closely monitored to ensure that there is a balance between the two. Having a balance prevents blood clotting (too much vitamin K and not enough Coumadin) and extreme thinness of blood (not enough vitamin K and too much Coumadin) (14). Wolk Shakes are produced onsite by the hospital. The purpose of this supplement is to increase calories and protein consumption in those patients who would benefit from additional calories and protein if the diet alone is not providing an adequate amount for weight gain and wound healing (15). During the second visit of the study A.S. did not have any acute nutrition related problems and so a formal nutrition diagnosis was not made secondary to 100% food/beverage intake and 100% Wolk Shake intake three times a day. Formal education in the form of written literature was not given to A.S. during this visit as he was consuming enough calories and protein to meet his needs. 13 A.S. also appeared to have a decent knowledge base regarding the parameters of the cardiac diet as he stated he limited salt and fat intake prior to admission. Prognosis: Based on A.S.’s length of stay at the hospital and the physiological and psychological advancements that were observed, it appears that the prognosis for A.S. is quite good. However, as with any major surgery, there are some risk factors to consider when determining the overall prognosis for A.S. The most common complications post LVAD implantations are infection and sepsis (18%-59% of recipients) (12). Stroke is another common risk factor associated with LVAD therapy; the risk increases as long as the device remains in the patient’s body (12). The nutritional prognosis for A.S. can be viewed as either positive or negative. One positive is that with increasing BMI, the risk for mortality decreases (good for A.S. as his BMI was 36.1) (16). Furthermore for some individuals with heart failure, metabolites such as glucose and lactate will restore to normal levels. Unfortunately, the prognosis for protein restoration isn’t as good. In patients with heart failure, changes in myocardial metabolism occur resulting in decreased amino acid levels in cardiac tissues (16) and LVAD therapy does not allow for the recovery of these amino acid stores. A.S. appeared to be very motivated to get better. The day of his discharge he spoke of the struggles he faced throughout the progression of his disease and how thankful he was for the advancements in technology that allowed him to get a second chance at life. A.S. could not wait to get home to his family for the holidays and finally begin to enjoy his retirement. 14 Summary and Conclusion: This study allowed me to follow a patient from pre-surgery to post surgery, and finally to discharge for the first time. Studying A.S. for an extended period of time enabled me to observe the progression of the patient, and how nutrition intervention played a role in those progressions. The research that was performed throughout the case study allowed me to strengthen my knowledge in cardiac nutrition beyond the topic of LVAD therapy. This case study also allowed for me to research different methods of calculating needs that are not necessarily used by the hospital. It was interesting to learn how different equations can be used for different conditions, and how the degree of those conditions has an effect on how the equation itself is manipulated. The part that I liked most about this study was the ability to follow A.S. throughout his stay. I felt that it really allowed me to get to know him as an individual rather than just as a patient. I think this is important when it comes to working in healthcare because healthcare providers have to be empathetic towards their patients in order to provide them with the best care possible. All in all I thought this case study provided me with a great experience. Sure, there was a lot of time that was put into it, but there wasn't a second that I wasn't learning. This study has definitely allowed me to strengthen my clinical knowledge and has allowed me to become more confident in my capabilities as a future Registered Dietitian. 15 Appendix 1: Medications (14) Medication Albuterol Amiodarone Purpose Serves as a bronchod ilator & vasodilat or Antiarrhy thmatic agent Table 1.5 A.S.’s Medications Nutritional Drug interactions implications Tenormin, Normodyne, Lopressor, Corgard, Inderla, Lanoxin, Epipen, Alupent, Xoponex, Asendin, Norpramin, Adapin, Tofranil, Nardil, Eldepryl, Parnate Iodine, Trazodone, Coumadin, Lipitor, Questran, Mevacor, Zocor, Tagamet, Plavix, Crixivan, Norvir, Alavert, Rheumatrex, Rifadin, St. John’s wort Other Side Effects Nausea, diarrhea, dry mouth, constipation, dyspepsia, vomiting, gastrointestinal motility disorder, stomatitis, dry throat, heart burn, gastrointestinal distress, low potassium Uncontrollable shaking, nervousness, headache, cough, throat irritation, muscle/bone/back pain, irregular heartbeat, chest pain, rash, hives, itching, swelling of face/throat/tongue/lips/eyes/han ds/feet/ankles/lower legs, increased difficulty breathing, difficulty swallowing, hoarseness Anorexia, nausea, vomiting, loss of appetite, constipation, altered taste, changes in amount of saliva, changes in ability to taste and smell, cannot drink grapefruit juice Headache, decreased sex drive, difficulties falling asleep, flushing, dry eyes, rash, restlessness, intolerance to heat/cold, thinning hair, excessive sweating, changes in menstrual cycle, swelling in neck, eye pain, swelling of hands/feet/ankles/lower legs, uncontrollable shaking, numbness in arms and legs, muscle weakness 16 Bumetanide Carvedilol Loop diuretic with rapid onset, used to lower blood pressure, treat edema Vasodilat or, reduces periphera l vascular resistanc e, decreases blood pressure, used to treat heart failure Prednisone, Lanoxin, Indocin, Eskalith, hypertension medications Nausea, vomiting, loose stools, thirst, constipation, low potassium Muscle cramps, weakness, dizziness, sore throat with fiver, ringing in ears, loss of hearing, unusual bleeding/bruising, severe rash w/peeling skin, difficulties breating/swallowing Tagment, Catapres, Neoral, Lanoxin, Cardizem, Epipen, Prozac, Insulin, MAOIs, Marplan, Nardil, Parnate, Eldepryl, Paxil, Rythmol, Serpalan, Rifadin, Calan Diarrhea, nausea, vomiting, gastrointestinal pain, hyperglycemia, extreme hunger, extreme thirst, weight gain, melena, periodontitis, GI hemorrhage, cannot consume alcohol Weakness, blurred vision, tiredness, lightheadedness, dizziness, headache, joint pain, difficulties falling asleep, cough, numbness in arms and legs, faintness, shortness of breath, chest pain, irregular heartbeat, rash, hives, itching 17 DocusateSenna Humulin Humalog Stool softener No medicine interactions but can affect absorption of some medications Gastrointestinal cramping, esophageal impaction, nausea, duodenal bezoars Faintness, brown discoloration of urine Lowers blood glucose levels. Should be taken during a meal Cadura, Minipress, Hytrin, Flomax, Hypoglycemia, redness, swelling, Uroxatral, ACE inhibitors, Elspar, Hypoglycemia, fat and itching at injection site, rash Tenormin, Coreg, Normodyne, build up, weight gain, and/or itching over entire body, Lopressor, Corgard, Inderal, constipation, monitor shortness of breath, wheezing, Betapace, Blocadren, Proglycem, alcohol consumption. dizziness, blurred vision, fast diuretics, MAO inhibitors, Meals should not be heartbeat, sweating, difficulty hormonal contraceptives, niacin, skipped and a diabetic breathing/swallowing, weakness, Sandostatin, Actos, Medrol, diet should be muscle cramps, abnormal Deltasone, Asprin, Sulfa Antibiotics, followed heartbeat, swelling of arms, hands, Thyroid medications feet, ankles, or lower legs Lowers blood glucose quickly. Should be taken 15 minutes before a meal ACE inhibitors, Lotensin, Capoten, Vasotec, Monopril, Prinivil, Univasc, Aceon, Accupril, Altace, Mavik, Edarbi, Atacand, Teveten, Avapro, Cozaar, Benicar, Micardis, Diovan, Tenormin, Normodyne, Lopressor, Corgard, Inderal, Antara, Lopid, Niacin, Reyataz, Prezista, Lexiva, Crixivan, Kaletra, Viracept, Norvir, Invirase, Aptivus, Catapres, Lanoxin, Norpace, Hypoglycemia, weight gain, constipation, large weight gain over a short period of time, monitor alcohol consumption. Meals should not be skipped and a diabetic diet should be followed Hypoglycemia, redness, swelling, itching at injection site, change in thickness of skin, rash and itching, difficulty breathing, hives, wheezing, fast heartbeat, sweating, weakness, muscle cramps, abnormal heartbeat, shortness of breath, swelling of the arms, hands, feet, ankles, or lower legs, 18 diuretics, Prozac, Marplan, Nardil, Eldepryl, Parnate, Sandostatin, oral contraceptives, Actos, Avandia, Decadron, Medrol, Deltasone, NebuPent, Trental, Symlin, Aspirin, Trisalate, Arthropan, Dolobid Lactobacillus Acidophillus Treats/pr events diarrhea (especiall y helpful for those taking antibiotic s) Immunosuppressant’s can increase risk of getting sick. These include: Imuran, Simulect, Neoral, Zenapax, CellCept, Prograf, Orasone, glucocorticoids Prevents/treats diarrhea. No known reactions with foods Pantoprazole Treats gastroeso phageal reflux disease (GERD) Coumadin, Reyataz, Lanoxin, diuretics, iron supplements, Nizoral, Rheumatrex, Viracept B12 deficiencies, nausea, vomiting, gas, severe diarrhea with watery stools, stomach pain, weakened stomach lining Ranolazine Antiangina (chest pain) Biaxin, Sporanox, Nizoral, Crixivan, Viracept, Norvir, Invirase, Carbatrol, Dilantin, Mycobutin, Rifadin, Priftin, St. John’s wort, Thiamine deficiency, folic acid deficiency, elimination of grapefruit juice from Is likely safe for pregnant and breastfeeding women, should not be given to those with compromised immune systems, may cause problems with individuals who have short bowel syndrome Headache, joint pain, blistering or peeling skin, rash, hives, itching, swelling of the eyes, face, lips, mouth, throat, or tongue, difficulty breathing/swallowing, hoarseness, irregular/fast/pounding heartbeat, excessive tiredness, dizziness, lightheadedness, muscle spasms, uncontrollable shaking of body, seizures, fever Headache, dizziness, fast/pounding/irregular heartbeat, difficulty breathing, fainting 19 Cordarone, Pacerone, Anafranil, Norpramin,Tofranil, Emend, Propulsid, Gengraf, Lanoxin, Cardizem, Norpace, Tikosyn, Erythrocin, Diflucan, Haldol, Risperdal, Geodon, Avelox, Orap, Betapace, Zagam, Calan diet, nausea, constipation 20 Spironolactone Controls high blood pressure, heart failure, and edema Lotensin, Capoten, Vasotec, Monopril, Prinivil, Univasc, Aceon, Accupril, Altace, Mavik, Edarbi, Teveten, Avapro, Cozaar, Benicar, Micardis, Diovan, Advil, Aleve, Lanoxin, Midamor, Dyrenium, Lovenox, Eskalith, Decadron, Medrol, Deltasone Potassium supplements Dizziness, unsteadiness, headache, enlarged/painful breasts, irregular menstrual periods, vaginal bleeding, difficulty Reduced sodium diet, maintaining/achieving erection, avoidance of deepening of voice, increased hair potassium rich growth, drowsiness, tiredness, foods/medications, restlessness, muscle vomiting, diarrhea, weakness/pain/cramps, stomach pain/cramps, pin/burning/numbing in hands nausea, loss of and feet, inability to move appetite, dry mouth arms/legs, changes in heartbeat, confusion, lack of energy, jaundice, rash, hives, itching, difficulty breathing/swallowing 21 Coumadin Prevents blood clotting Zovirax, Zyloprim, Xanax, Cipro, Biaxin, Noroxin, Ketek, Tygacil, Acova, Pradaxa, Angiomax, Iprivask, Refludan, Diflucan, Onmel, Nizoral, Monistat, Noxafil, Diflucan, Onmel, Lamisil, Vfend, Pletal, Plavix, Persantine, Effient, Ticlid, Emend, Celebrex, Flector, Nalfon, Advil, Indocin, Ponstel, Aleve, Daypro, Feldene, Clinoril, Cordarone, Rythmol, Norvasc, Cardizem, Calan, Singulair, Accolate, Zyflo, Xeloda, Gleevec, Tasigna, Lipitor, Tagamet, Pepcid, Zantac, Reyataz, Sustiva, Intelence, Lexiva, Crixivan, Viracept, Norvir, Invirase, Aptivus, Nuvigil, Provigil, Carbatrol, Dilantin, Banzel, Rifadin, Celexa, Pristiq, Cymbalta, Lexapro, Prozac, Luvox, Savella, Paxil, Zoloft, Neoral, Antabuse, Oxsoralen, Flagyl, oral contraceptives, Oxandrin, Actos, Inderal, Vibryd, Monitor vitamin K intake, gas, change in the way things taste, nausea, vomiting, diarrhea, loss of appetite, Abdominal pain, bloating, loss of hair, feeling cold or having chills, hives, rash, itching, difficulty breathing/swallowing, swelling of face/throat/lips/eyes, hoarseness, chest pain/pressure, swelling of hands/feet/ankles/lower legs, fever, infection, extreme tiredness, lack of energy, pain in upper right of stomach, jaundice, flu-like symptoms 22 Bibliography: 1. WebMD. Heart Failure Health Center. Available at: http://www.webmd.com/heart-disease/heart-failure/left-ventricular-assistdevice. Accessed January 2nd, 2014. 2. Fregmen BF, Frucht SS. Medical Terminology: A Living Language. 4th ed. Upper Saddle River, NJ: Pearson; 2009:132-137. 3. Tool Loop. Veins in the Cardiovascular System. Available at: http://www.tooloop.com/veins-in-the-cardiovascular-system/. Accessed January 9th, 2014. 4. Kumar V, Abbas AK, Fausto N, Aster JC. Pathologic Basis of Disease. 8th ed. Philadelphia, PA: Sunders Elsevier; 2010:533-537. 5.National Heart, Lung, and Blood Institute. What is Heart Failure? Available at: http://www.nhlbi.nih.gov/health/health-topics/topics/hf/. Updated January 9th 2012. Accessed January 9th, 2014. 6. Emory Healthcare. Heart Failure Stages & Functional Classifications. Available at: http://www.emoryhealthcare.org/heart-failure/learn-about-heartfailure/stages-classification.html. Accessed January 11th 2014. 7. Heart Failure Society of America. Questions About HF. Available at: http://www.abouthf.org/questions_stages.htm. Accessed January 11th, 2014. 8. Schwartz DB, DiMaria, RA. The A.S.P.E.N. Nutrition Support Core Curriculum a CaseBased Approach-The Adult Patient. 1st ed. Silver Spring, MD: American Society for Parenteral and Enteral Nutrition; 2007:495-501. 9. Mahan KL, Escott-Stump S, Raymond, JL. Krause’s Food and the Nutrition Care Process. 13th ed. St. Louis, MO: Elsevier Saunders; 2012:194;897. 10. Mayo Clinic. Diseases and Conditions. Available at: http://www.mayoclinic.org/diseases-conditions/diabetes/expertblog/diabetes-blog/BGP-20056560. Accessed January 11th, 2014. 11. Mayo Clinic: Mayo Medical Laboratories. Test ID: Cl. Available at: http://www.mayomedicallaboratories.com/testcatalog/Clinical+and+Interpretive/8460. Accessed January 11th, 2014. 12. Rizzieri, A., Verheijde, J., Rady, M., & McGregor, J. (2008). Ethical challenges with the left ventricular assist device as a destination therapy. Available at http://www.ncbi.nih.gov/pmc/articles/PMC2527574/. Accessed December 17th, 2013. 13. American Dietetic Association. Nutrition Care Manual®. Heart Failure: Nutrition Prescription. http://nutritioncaremanual.org/topic. Accessed December 17th, 2013. 14. Medline Plus Trusted Health Information for You. Drugs, Supplements, and Herbal Information. Available at: http://www.nlm.nih.gov/medlineplus/druginformation.html. Accessed January 9th, 2014. 15. Florida Hospital. Enteral Nutrition Formulary. 2013 16. Weitzel LB, Ambardekar AV, Brieke A, Cleveland JC, Serkova NJ, Wischmeyer PE, Lowes BD. Left Ventricular Assist Device Effects on Metabolic Substrates in the Failing Heart. April 2013; 8(4):1-6 23