Upper respiratory trac - Ipswich-Year2-Med-PBL-Gp-2
advertisement

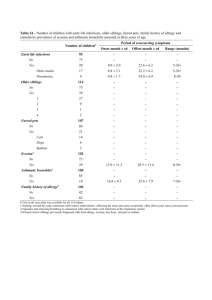
Upper respiratory tract NORMAL FLORA Mouth: Staph epidermidis *Actinomyces Mycoplasma *Candida Viridians streptococci Bacteroides spp. Peptostreptococcus *Fusobacterium *Spirochaetes Nose/Throat: *Staph aureus Staph epidermidis *Streptococcus pneumoniae *Streptococcus pyogenes *Moraxella catarrhalis *Haemophilis influenzae *Neisseria meningitidis Bacteroides Corynebacterium Viridans streptococci Peptostreptococcus Fusobacterium COMMON PATHOGENS & DISEASES CAUSED Mouth: Actinomyces Fusobacterium Spirochaetes Candida albicans (fungi) Nose/throat: Staph aureus Streptococcus pneumoniae Otitis media (1) Sinusitis (1) LRTIs Meningitis Pneumonia Streptococcus pyogenes Pharyngitis Acute glomerulonephritis Rheumatic fever Haemophilus influenzae Otitis media (2) Sinusitis (2) Epiglottitis LRTIs Meningitis Bordetella pertussis SPECIMENS ANTIBIOTICS COMMONLY USED Throat swab tonsillar areas, posterior pharynx and any areas of inflammation Tongue must be depressed in order to minimize contamination with oral secretions most throat infections are viral in origin, throat swabs are only useful if there is a suspicion of a serious overlying bacterial infection Nasopharyngeal swab useful for isolation of Bordetella pretussis Blood Nasal swab determines the carrier state for S. aureus Acute bacterial rhinosinusitis (Streptococcus pneumoniae or Haemophilus influenzae and less frequently by Moraxella catarrhalis) – use amoxicillin If allergic to penicillin: Cefuroxime or cefaclor or doxycycline Acute pharyngitis and/or tonsillitis: Streptococcus pyogenes phenoxymethylpenicillin Whooping cough Moraxella catarrhalis Otitis media (3) Sinusitis in children (2) Neisseria meningitidis Viruses: Adenovirus Rhinovirus Enterovirus Influenzae, parainfluenzae RSV Lower respiratory tract NORMAL FLORA None COMMON PATHOGENS & DISEASES CAUSED Common: Streptococcus pneumoniae Haemophilis Influenzae Moraxella catarrhalis Mycoplasma Mycobacterium Less common: Staph aureus Pseudomonas aeruginosa SPECIMENS Sputum expectorated from the LRT, often contaminated with saliva, mouth and URT organisms. Blood Bronchoalveolar lavage ANTIBIOTICS COMMONLY USED Non-specific cough: lignocaine via nebuliser Acute exacerbations of bronchiectasis: Amoxyicillin If sputum grows P. aeruginosa: ciprofloxacin Aspiration pneumonia: benzlpenicillin PLUS metronidazole Standard short term TB: isoniazid plus Legionella Candida albicans (opportunistic fungi) Class QUINOLONES Drug Ciprofloxacin (C-flox®, Profloxin®) 250, 500, 750 mg (14) rifampicin plus ethambutol plus pyrazinamide Influenza: oseltamivir Indications mostly G-ve cover Side effects rash/itch complicated UTI n&v diarrhoea abdo pain/dyspepsia Traveller’s diarrhoea b'cidal; inhibit bacterial DNA synthesis Shigelosis Norfloxacin (Roxin®, Noroxin®) 400 mg (14) tendonitis, myalgia dizzy Prostatitis photosensitivity Salmonella, Typhoid crystalluria CNS (dizziness, headache, ↓ seizure threshold) **Cipro interacts with warfarin (↑INR) and phenytoin (↓conc.) Cat B3 (fetal arthropathy) avoid in b/f Penicillins Moderate - Broad Spectrum: G+ve, some G-ve Amoxycillin (Amoxil, Moxacin) 250, 500, 1000mg 25mg/mL, 50mg/mL, 100mg/mL b'cidal; interfere with bacterial cell Amoxycillin + Clavulanic acid URTI (G+ve) Pneumonia UTI (G-ve) Bites, clenched fist injuries Otitis media, sinusitis H. pylori eradication WT diarrhoea nausea rash urticaria **ALLERGY** occurs in 10% of ppl – crossreactivity between penicillins, cephalosporins, and carbapenems wall peptidoglycan synthesis (Augmentin, Clavulin) 500/125, 875/125 25mg/mL, 6.25mg/mL 80mg/mL, 11.4mg/mL Narrow spectrum: G+ve Staph Dicloxacillin (Diclocil, Dicloxsig) 250, 500mg Staph. skin infections Pneumonia Osteomyelitis Septicaemia cholestatic hepatitis (augmentin, di/fluclox, cilicaine VK) Flucloxacillin (Flopen, Staphylex) 250, 500mg 25mg/mL, 50mg/mL Strep IV penicillins (benzylpenicillin, benzathine penicillin, phenoxymethylpenicillin, procaine penicillin) C/I: allergy to penicillin, cephalosporin or carbapenems dose reduce in RI Safe to use in pregnancy and breastfeeding Phenoxymethylpenicillin (Abbocillin VK, Cilicaine VK) 250, 500 mg Macrolides b'static; inhibit bacterial protein synthesis by binding to 50S ribosomal sub-unit 1. Roxithromycin (Rulide, Biaxsig) 150, 300mg 50mg dispersible tonsillitis/pharyngitis skin infections Class indications: Alternatives to penicillins and cephalosporins in allergic patients. MAC and pertusis treatment and prophylaxis ______________________ 2. Erythromycin (Eryc, E-mycin) 250, 400mg Chlamydial infections (azithromycin > clarithromycin) n/v diarrhoea abdominal pain candidal infection rash (Stevens-Johnson syndrome) 40mg/mL, 80mg/mL EES H. pylori eradication (clarithromycin) Respiratory tract infections (all except azithromycin) CAP (roxithromycin, azithromycin) 3. Clarithromycin (Klacid, Clarac) 250, 500mg Recurrent tonsillitis (roxithromycin) Skin infections (roxithromycin) QT elongation E>C>A (not with R) Erythromycin causes infantile hypertrophic pyloric stenosis in infants <2 weeks old Drug interactions and abdo discomfort E>C>R>A Trimethoprim b'static; competitively inhibits bacterial folate production essential for bacterial growth(G ve) 4. Azithromycin (Zithromax) 500, 600mg C/I: allergies to macrolides Alprim, Triprim 300 mg Uncomplicated lower UTI Epidymo-orchitis Prostatitis Safe to use in pregnancy and breastfeeding Trimethprim fever itch rash n/v, gastric upset hyperkalaemia* blood dyscrasias megablastic anaemia Co-trimoxazole trimethoprim + sulfamethoxazole Bactrim, Resprim, Septrim 80mg/400mg 160mg/800mg DS, Forte 8mg/mL, 40mg/mL susp. Shigellosis (GI infection) Traveller’s diarrhoea Stevens-Johnsons syndrome C/I: allergy to trimethoprim, severe renal impairment*, megablastic anaemia due to folate deficiency, pregnancy (1st trimester) Sulfamethoxazole photosensitivity headache, drowsiness allergy to sulfamethoxazole, hepatic impairment, late pregnancy Tetracyclines Doxycycline (Doxylin, Doxy, Vibramycin) 50, 100 mg Acne Malaria prophylaxis anorexia sore mouth ADEC Cat B3; avoid in first trimester Safe in b/f GI upset (n/v, dairrhoea, epigastric burning) teeth discolouration enamel dysplasia Respiratory tract infections b’static; inhibit bacterial protein synthesis by reversibly binding to 30S sub-unit of the ribosome CAP Exacerbation of chronic bronchitis Acute bacterial sinusitis photosensitivity Chronic prostatitis ↑ intracranial BP causes headache (doxycycline) oesophageal ulcers inhibition of bone growth Minocycline; abdominal cramps and vestibular toxicity (dizziness, vertigo, ataxia) C/I: allergy to tetracycline, children <8 due to teeth discolouration and enamel dysplasia D/I: retinoids, MTX, rifampicin Minocycline (Akamin, Minomycin) 50, 100 mg Acne OR (with Orfloxixin and Rifampicin) leprosy ADEC Cat D Avoid in b/f (short courses of 7-10 days ok) Nitromidazoles Metronidazole (Flagyl, Metrogyl) 200, 400 mg 40mg/mL Anaerobic bacterial infections (G+ve and G-ve) Protozoal infections n/v abdominal pain diarrhoea anorexia Dental infection metallic taste, furry tongue Aspiration pneumonia CNS effects (dizziness, headaches) Bacterial vaginosis Paraesthesia, peripheral neuropathy H. pylori eradication Wounds (e.g. diabetic foot ulcer) disulfuram reaction when taken with alcohol Tinidazole (Fasigyn, Simplotan) 500 mg Rifampicin Rifadin, Rimycin 150, 300, 600mg C/I: treatment with disulfiram, renal/hepatic impairment TB MRSA ADEC Cat B2 Safe to use in b/f GI irritation (n/v, cramps, diarrhoea) orange-red discolouration of body fluids staining of soft contact lenses rash increase liver enzymes arthralgia, myalgia CNS (dizziness, headache, ataxia, confusion) hepatotoxicity rifamycins are b’cidal; inhibit bacterial RNA polymerase Reserve rifamycins for MRSA, mycobacterial infections and prophylaxis of mengitis and epiglottitis Fuscidic acid Nitrofurantoin C/I: allergy to rifampicin D/I: rifampicin induces CYP450 enzymes lots of significant drug interactions Fucidin® 250 mg Macrodantin® 50, 100 mg MRSA with rifampicin Acute lower UTIs Prophylaxis or long term suppressive treatment in recurrent UTI inhibits bacterial protein, DNA, RNA and cell wall synthesis Avoid use in elderly and renally impaired as more likely to experience peripheral neuropathy. Cephalosporins same mechanism of Moderate Spectrum G+ve: anti-strep, staph G-ve: E. coli, Klebsiella Cephalexin Staphylococcal and streptococcal infections in ADEC Cat C, use with caution Safe to use in b/f lethargy GI upset drowsiness vertigo headache n/v anorexia peripheral neuropathy hepatotoxicity pulmonary toxicity rash GI disturbance (n, d, electrolyte disturbance) rash action as penicillins cross-sensitivity Cephalexin (Keflex) 250, 500 mg (20) people with mild-to-moderate penicillin allergy UTIs due to susceptible Gramnegative bacteria 25, 50 mg/mL headache rarely anaphylactic shock, bronchial obstruction Epididymo-orchitis Surgical prophylaxis (cephazolin) 5-10% cross-reactivity with allergy to penicillins ______________________ + anti-himophilus activity (against Hib) Cefaclor (Ceclor) 375 mg CR (10) 25, 50 mg/mL Otitis media (particularly in children) Respiratory tract infections caused by H. influenzae Acute bacterial sinusitis Cefuroxime (Zinnat) (cefuroxime - gonococcal infections) ______________________ Ceftriaxone (Rocephin) → Broad Spectrum Aminoglycoside Gentamicin Pneumonia Bacterial meningitis Septicaemia Sexually acquired epididymoorchitis (with doxycycline) Empirical treatment of serious Gram-negative infections C/I: immediate/severe allergy to penicillins Ototoxicity (hearing loss, tinnitus, balance problems, n/v) Hepatotoxicity Neuromuscular toxicity (potentially fatal e.g. respiratory depression – treat with calcium gluconate)