防乳癌Tamoxifen、Evista各有利弊
advertisement

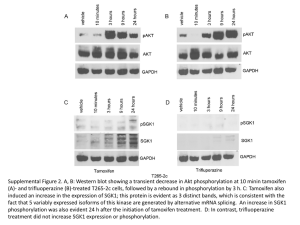
防乳癌 Tamoxifen、Evista 各有利弊 最新研究顯示,罹患乳癌高風險的年長婦女,現在有兩種可預防乳癌的藥物供選擇,但需考量 兩者的優缺點。 研究顯示,雖然最常用的乳癌 荷爾蒙治療藥物 Tamoxifen,效果更佳,且藥效持續更久,但以 Evista 名稱上市、較新的 Raloxifene 藥,則更為安全。 德州大學安德森癌症中心癌症專家李普曼(Scott Lippman)說:「我看不出哪一種藥最好。」但 兩種藥都是具有不同風險和益處的不錯選擇。 李普曼也是「癌症預防研究」期刊的編輯,他 19 日在該期刊發表這篇由聯邦贊助的長期研究 結果;這份報告也將在美國癌症研究協會(AACR)於華府舉行的年會中提報。 Tamoxifen 是在患者診斷後,廣泛用於治療癌症的藥物,Evista 則是治療骨質疏鬆的藥物。不過, 兩種藥物 至今尚未被廣泛視為預防癌症的藥物。專家希望這項研究的發現將有助較高風險的婦 女考量使用兩者其中一種藥物。 這兩種藥物不建 議用於一般乳癌風險的女性,但對於數百萬名因基因突變、家族病史或其他因 素,而有較高風險的女性而言,將可產生極大效果。 該研究顯示,Tamoxifen 可把罹患最嚴重乳癌的機率減少一半,但有造成子宮癌的副作用; Evista 則可降低 38%癌症風險,子宮問題和其他副作用也較少。 這項稱為 STAR 的研究,分析了約有 2 萬名乳癌高風險停經婦女使用不同藥物後的狀況。喬治 城大學科學家約丹(V. Craig Jordan)表示,Evista 顯然比較安全,但是預防癌症的效果卻較快消 減。 Tamoxifen, Evista Prevent Breast Cancer Study Shows Tamoxifen Is a Little More Effective, but Evista May Have Less Risk By Charlene Laino / WebMD Health News April 20, 2010 (Washington, D.C.) -- There are two good drug options for preventing breast cancer in high-risk women, and more women need to take advantage of them, doctors say. Updated results from a large breast cancer prevention trial confirm that both the old standby tamoxifen and the osteoporosis drug Evista can substantially cut the risk of developing breast cancer in high-risk postmenopausal women. Tamoxifen works a little better, but Evista may be a little safer, says study head D. Lawrence Wickerham, MD, of Allegheny General Hospital in Pittsburgh. 1 But "only 5% to 20% of the tens of thousands of women" who could benefit from the drugs use them, says Gabriel Hortobagyi, MD, a breast cancer specialist at the University of Texas M.D. Anderson Cancer Center in Houston who was not involved with the work. Over 192,000 women, about 150,000 of whom were postmenopausal, were diagnosed with breast cancer in 2009, he says. Updated results from the STAR (Study of Tamoxifen and Raloxifene) trial were presented at the annual meeting of the American Association for Cancer Research and published online by the journal Cancer Prevention Research. Tamoxifen has been used for years to help fight breast cancer's return. In 1998, the FDA approved tamoxifen for use by women who hadn't had breast cancer but were at high risk of developing the disease. Evista, known generically as raloxifene, is taken by about half a million women in the U.S. to prevent and treat osteoporosis, or thinning of the bones. In 2007, the FDA approved it for breast cancer prevention in some high-risk postmenopausal women based on earlier results from STAR and other trials. As a breast cancer preventive, they're recommended for women at higher-than-average risk because of genetic mutations, family history, or other factors, including age over 60. Tamoxifen vs. Evista The updated analysis of the federally funded study involved nearly 20,000 postmenopausal women followed for almost seven years during and after treatment with either tamoxifen or Evista. Earlier findings from the study, published in 2006, showed that both drugs reduced the risk of breast cancer by about 50% in high-risk, postmenopausal women. But Evista appeared to carry fewer risks of side effects, with lower rates of uterine cancer and clotting problems. The new findings suggest that several years after treatment, which lasts about five years, tamoxifen is substantially better than raloxifene at preventing breast cancer. About two years after treatment ended, tamoxifen reduced the risk of invasive breast cancer by 50%, while Evista cut risks by 38%. Put another way, Evista was 76% as effective as tamoxifen, says Wickerham, who serves as a consultant to makers of both drugs. Evista was about 78% as effective as tamoxifen at preventing noninvasive breast cancers (lobular carcinoma in situ and ductal carcinoma in situ). But women who took Evista "continued to have substantially fewer of the serious side effects, including uterine cancers, clotting problems, and cataracts, that seem to be barriers to tamoxifen use," he says. 2 There were 2.25 cases of uterine cancer per 1,000 women treated with tamoxifen vs. 1.23 per 1,000 among women treated with Evista. There were 3.30 blood clot events per 1,000 women treated with tamoxifen vs. 2.47 per 1,000 among women treated with Evista. "The absolute risk of these problems for any given woman is quite low, regardless of treatment," says M.D. Anderson's Scott Lippman, MD. There was no difference in death rates among the two groups. Neither of the drugs has been shown to extend lives in high-risk women. Who Is Considered a High-Risk Patient? So which drug is better for which women? Both drugs are only for women at high risk, doctors stress. In the study, women were considered to be at high risk if their risk of developing breast cancer over the next five years was 1.67% based on a simple formula called the Gail model that takes into account age, family history, and other factors. By definition, anyone over age 60 was at high risk. But Hortobagyi says he probably wouldn't give the drugs to a woman in her 60s who is otherwise healthy based on age alone. "It's a discussion each woman needs to have with her doctor. The more risk factors, the greater she will benefit." If you and your doctor conclude you are at increased risk and you are not at risk for blood clots or uterine cancer, both drugs are good breast cancer prevention options, Hortobagyi says. If you are at risk for these problems, Evista is the better choice, he says. All things being equal, some women may want to take tamoxifen because it is slightly more effective, the experts say. On the other hand, postmenopausal women with thinning bones might want to consider Evista because it "offers two benefits in one," Lippman says. The study only included postmenopausal women, but as a treatment for breast cancer, tamoxifen has a proven track record in premenopausal women as well, Hortobagyi says. Evista is only approved for use after menopause, so its safety and effectiveness in premenopausal women is unknown, he says. High-risk premenopausal women who have had a hysterectomy -- and therefore a "close to nonexistent" risk of uterine cancer -- and who have no history of blood clots may want to talk to their doctor about taking tamoxifen, he says. Both drugs cost about $140 a month or $8,400 for five years of treatment. In comparison, treating one case of early breast cancer can easily cost $50,000 to $120,000, according to Hortobagyi. Long term, tamoxifen stops more cancer than Evista (Reuters) - Longer-term results from a head-to-head trial of two drugs that prevent breast cancer shows that tamoxifen works better than rival Eli Lilly and Co's Evista, but with a greater risk of some other cancers and blood clots. 3 After nearly seven years of follow-up, researchers found that women who took tamoxifen for five years were less likely to develop breast cancer than those who took Evista, known generically as raloxifene. But they told a meeting of the American Association for Cancer Research that both drugs are useful and that women should be able to choose. Only tamoxifen is approved for women who have not yet gone through menopause, and many may not want to risk its side effects. Tamoxifen was originally sold by AstraZeneca Plc under the brand name Nolvadex and is now available generically. Both drugs are in a class known as selective estrogen receptor modulators. The researchers on the so-called STAR trial calculate that tamoxifen lowers the risk of breast cancer in high-risk women by 50 percent, compared with 38 percent for Evista. Overall, both drugs also saved lives. "There is no statistically significant mortality difference between the two treatment groups," the team, called the National Surgical Adjuvant Breast and Bowel Project, wrote in the journal Cancer Prevention Research. After 81 months of follow-up, 236 women who took tamoxifen had died of any cause, compared with 202 who took raloxifene. When the researchers first reported their findings from the STAR trial of more than 19,000 women in 2006, there was little difference between the two drugs. Now the differences are clearer, perhaps because raloxifene is less potent than tamoxifen, said the researchers, who were led by Dr. Victor Vogel of the University of Pittsburgh. "The updated results reported here demonstrate that after a median follow-up of 81 months, which represents 60 months of treatment plus an additional 21 months of follow-up, raloxifene no longer appears to be as effective as tamoxifen in preventing primary invasive breast cancer," the researchers concluded. SIDE EFFECTS Tamoxifen's side effects are clearer after more years of study, however. It prevents breast cancer for as long as 15 years. But it raises the risk of rarer diseases such as uterine cancer, while Evista does not. Tamoxifen also raises the risk of blood clots in the leg -- called deep-vein thrombosis -- which can travel to the lungs to cause a pulmonary embolism. "The superiority of tamoxifen over raloxifene in reducing breast cancer risk comes with a cost: significantly more endometrial cancers, hysterectomies for benign disease, thromboembolic events, and cataracts," the researchers wrote. "These toxicities may be acceptable for the treatment of breast cancer but have proved to be a barrier to the use of tamoxifen for preventing primary breast cancers." 4 Women therefore may be more likely to take raloxifene. "Our results demonstrate that raloxifene (compared with tamoxifen) retains substantial benefit in reducing the risk of invasive breast cancer and has fewer life-threatening side effects, including significantly fewer endometrial cancers," the researchers wrote. Women are only eligible to take either drug if they have a high risk of breast cancer -- for instance, if they have had cancer in one breast and want to prevent it from coming back in the other, if they have a genetic risk of breast cancer, or if they have had a benign tumor called ductal carcinoma in situ. 5