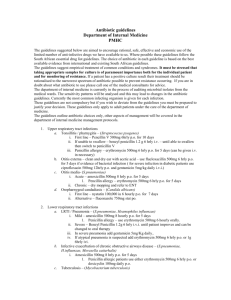
Sexual Transmitted Infections
advertisement

Sexual Transmitted Infections When treating someone with STIs ensure privacy and confidentiality. All treatments should be combined with a HIV test and make efforts to trace and treat all sexual contacts. Provide good sexual health advice, condoms and advice on partner notification, monogamy and informing all partners. Sexually transmitted infections are classified as… Genital ulcer disease Urethral discharge Lower abdo pain Acute scrotal swelling Enlarged LN Balanitis Genital warts Syphilis Gential ulcer disease Where the genitals are covered in painful (herpes) or painless ulcers (chancroid, syphilis). Herpes is the most common cause though these infections can co-exist togather. If there are fluctuant (fluid filled) lymph nodes aspirate and send to the laboratory. Treatment Ciprofloxacin 500mg PO stat Benzathene penicillin 2.4 MU intramuscular stat Acyclovir 800mg BD PO for 7 days If the patient is pregnant or allergic to penicillin Switch Benzathene penicillin to Erythromycin 500mg TID for 15 days Infants born to mothers with GUD should be given Benzathene penicillin 500,000 IU/kg IM stat Follow up the patient after 7-10 days If the ulcers have worsened… Check compliance (traet again if not complied) Azithromycin 2.4g stat If the ulcers have improved slightly… Repeat chancroid treatment ciprofloxacin 500mg stat Provided by T. Whitfield 2012 Follow up the patient until the ulcers have healed, refer for specialist opinion if failing to heal. Urethral discharge This is a painful or painless discharge of small or large volume from the penis or vagina. It may be green in colour (gonorrhoea) or clear. Differential diagnosis includes urinary tract infection, prostatis and schistosomiasis. A discharge is more commonly seen in male patients, female patients may also have the infection and be infective without symptoms. Female partners also need to be treated to prevent reinfection/ spread. Common causes of urethral discharge are Nesseria gonorrhoea, Chlamydia trachomatis and trichomonas vaginalis. In women candida is also a common cause of discharge. Treatment of discharge Gentamicin 240mg IM stat Doxycycline 100mg BD for 7 days Metronidazole 2g stat Clotrimazole500mg pessary (add for women with white discharge) Doxycline cannot be given in pregnancy/lactation use Erythromycin 500mg QID for 7 days Review after 7 days, check compliance and reinvestigate/ refer if symptoms persist. Lower abdominal pain in women If the patient has an overdue or late period the ectopic pregnancy must be excluded before any other intervention is done. βHCG will rule out ectopic pregnancy. Refer to gynaecology immediately if any recent abortion, labour, caesarean, acute vaginal bleed/menorrhagia, abdominal guarding or rebound tenderness. Symptoms and signs include pain on intercourse (dysparuina), discharge, cervical tenderness. In patients should be managed under gynaecology to exclude diagnosis other than PID: I/v fluids Gentamycin 1.5mg/kg IV/IM every 8 hours Chloramphenicol 500mg IV every 6 hours Metronidazole 500mg IV every 8 hours Provided by T. Whitfield 2012 When able to swallow Doxycyline 100mg BD until 10 days of treatment Metronidazole 400mg BD until 10 days of treatment If the patient has no immediate gynaecological problem they can be treated for pelvic inflammatory disease as out-patient: Gentamicin 240mg IM stat Doxycycline 100mg BD for 7 days Metronidazole 400mg BD for 10 days Remove any intrauterine device Review the patient after 72 hours if no improvement refer to gynaecology. Acute scrotal swelling A patient with sudden painful scrotal swelling may have testicular torsion this needs to be excluded, by urgent urological opinion. Feel the testes does it feel like a hydrocele, varicoele or inguinal hernia? Has there been a recent history of trauma? If so this is a surgical problem. If a sexual history suggests UTI then treat Gentamicin 240mg IM stat Doxycycline 100mg BD for 7 days Enlarged inguinal lymph nodes (bubo) Bubo are caused by chancroid and lymphogranuloma venereum. Exclude other causes of lymphadenopathy: foot, leg and genital infections, HIV, TB and leukaemia. Ensure there is no cough impulse or reducibility seen in hernias. Aspirate and fluctuant nodes and send the sample to the lab. If genital ulcers are present treat as for genital ulcer disease (see above). If no genital ulcers treat for lymphogranuloma venereum Doxycycline 100mg BD for 7 days Provided by T. Whitfield 2012 Doxycline cannot be given in pregnancy/lactation use Erythromycin 500mg QID for 14 days. If the lymph nodes persist obtain a biopsy for diagnosis. Balanitis Persitant inflamtion of the end of the penis, persistant in diabetics and HIV infected individuals. If ulcers treat genital ulcer disease, if dischrarge treat as discharge. If itching maybe candidiasis. Treat candida with Gentian violet 1% solution od for 7 days. Clotrimazole pessary to partner. If persists treat with metronidazole 2g stat Counsel risks of UTI. Genital Warts These are wart like lesions on or near the genitals. Treatment: Compound podophyllin paint weekly to the warts. Allow to dry before touching the area with normal skin. Yellow soft paraffin will prevent contact with normal tissue Wash off after 1-4 hours Silver nitrate stick pencil once daily as an alternative Not to be used during pregnancy. In extreme cases surgical removal or electro cautery therapy may be used. Syphilis This is classified as primary, secondary, latent and tertiary. Primary syphilis presents with a painless ‘punched out’ chancre (ulcer) at the site of sexual contact (usually genitals also mouth, hands, anus). In HIV multiple chancre’s can occur. The chancre will appear 14 days to 3 months after infection and will disappear 1-2 months after initial appearance. Secondary syphilis presents 1- 6 months after infection. The most common symptom is a rash which can be macular, popular, pustular or mixed. Its main feature tends to be that it Provided by T. Whitfield 2012 involves the palms and soles of the feet which is rare in other diseases. In HIV secondary syphilis can progress to early neurosyphilis with a clinical picture of meningitis, stroke or fits. Secondary syphilis can also effect other organs and cause lymphadenopathy, snail track mouth ulcers, glomerulonephritis, hepatitis, iritis and arthritis. Latent syphilis occurs after the resolution of ssecondary syphilis at 3-12 weeks. One quarter of these patients will progress to tertiary syphilis. Tertiary syphilis can occur up to 20 years after initial infection, it can take several forms… Gumatous syphilis- granulomatous regions on skin, bone and mucus membranes destroy that area. Cardiovascular syphilis- causes aneurysms and aoritic regurgitation Neurosyphilis- general paresis of the insane (disturbed, confused patient) or tabes dorsalis (ataxia, peripheral sensory loss, arreflexia) Treatment for early syphilis (primary, secondary, latent<2years): Benzathene penicillin 2.4 MU IM (1.2 MU in each buttock) If allergic to penicillin Doxycline 100mg BD for 15 days If also unable to take doxycycline (pregnant/ lactating) Erythromycin 500mg QID for 15 days Treatment for late syphilis (latent> 2years, tertiary except neurosyphilis): Benzathene penicillin 2.4 MU IM (1.2 MU in each buttock) every week for 3 weeks If allergic to penicillin Doxycline 100mg BD for 30 days If also unable to take doxycycline (pregnant/ lactating) Erythromycin 500mg QID for 30 days Treatment for neurosyphilis: Benzylpenecillin 4 MU IV QID for 14 days Benzathene penicillin 2.4 MU IM (1.2 MU in each buttock) every week for 3 weeks If allergic to penicillin Doxycline 100mg BD for 30 days If also unable to take doxycycline (pregnant/ lactating) Erythromycin 500mg QID for 30 days Provided by T. Whitfield 2012