Epidemiology and Clinical Manifestations of Children With
advertisement

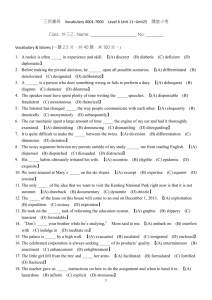
Epidemiology and Clinical Manifestations of Children With Macrolide-Resistant Mycoplasma pneumonia Pneumonia in Taiwan Ping-Sheng Wu, MD,1 Luan-Yin Chang, MD, PhD,2 Hsiao-Chuan Lin, MD,3 Hsin Chi, MD,4 Yu-Chia Hsieh, MD, PhD,5 Yi-Chuan Huang, MD,6 Ching-Chuan Liu, MD, MPH,7 Yhu-Chering Huang, MD, PhD,5* and Li-Min Huang, MD, PhD 2** Summary. Mycoplasma pneumoniae accounts for 10–30% of community-acquired pneumonia (CAP) in children. This study reveals the epidemiology and clinical manifestations of children with macrolide-resistant (MLr) M. pneumoniae pneumonia in Taiwan. Respiratory tract specimens were collected from children hospitalized with CAP for evaluation via PCR followed by DNA sequencing for several point mutations related to the MLr character. Of the 412 specimens collected during the study period, 60 (15%) were positive for M. pneumoniae, 14 (23%) of which presented point mutation (all A2063G) in 23S rRNA. Clinical symptoms and chest Xray findings between the MLs and MLr groups were not significantly different. However, the MLr group had longer mean duration of fever after azithromycin treatment (3.2 days vs.1.6 days, P 1 0.02) and significantly higher percentage of changing antibiotics for suspected MLr strain(42% vs. 13%, P 1 0.04). Although 58% of children in the MLr group did not receive effective antibiotics, all children were discharged without sequelae. In conclusion, 15% of CAP in children is caused by M. pneumoniae and the macrolide-resistance rate is 23% in Taiwan. Despite ineffective antibiotics, children with MLr M. pneumoniae pneumonia recover completely. Pediatr Pulmonol. 2013; 48:904–911. _ 2012 Wiley Periodicals, Inc. Key words: children; drug resistance; macrolides; Mycoplasma pneumoniae pneumonia. Funding source: National Health Research Institutes, Taiwan. INTRODUCTION Mycoplasma pneumoniae (M. pneumoniae) is an important respiratory pathogen in children that causes many upper and lower respiratory tract diseases, including wheezing, coryza, and bronchopneumonia.1 It accounts for 10–30% of community-acquired pneumonia (CAP) in children.2,3 Because of the lack of cell walls, beta-lactam antibiotics are not effective and macrolides are generally the first choice antibiotics for the treatment of M. pneumoniae infections. M. pneumoniae pneumonia is considered a self-limiting disease but 1Department of Pediatrics, Buddhist Tzu Chi General Hospital, Taipei Branch, Taipei, Taiwan. 2Department of Pediatrics, National Taiwan University Hospital, Taipei, Taiwan. 3Department of Pediatrics, China Medical University Hospital, Taichung, Taiwan. 4Department of Pediatrics, Mackay Memorial Hospital, Taipei, Taiwan. 5Division of Infectious Diseases, Department of Pediatrics, Taoyuan Chang-Gung Memorial Hospital and Chang-Gung University College of Medicine, Taoyuan, Taiwan, Taiwan. 6Division of Infectious Diseases, Department of Pediatrics, Kaohsiung Chang-Gung Memorial Hospital and Chang-Gung University College of Medicine, Kaohsiung, Taiwan. 7Department of Pediatrics, National Cheng-Kung University Hospital, Tainan, Taiwan. Ping-Sheng Wu and Luan-Yin Chang contributed equally to this work. Conflict of interest: None. *Correspondence to: Yhu-Chering Huang, MD, PhD, Department of Pediatrics, Chang-Gung Memorial Hospital, No. 5, Fu-Hsin Street, Kweishan, Taoyuan 333, Taiwan. E-mail: ychuang@adm.cgmh.org.tw **Correspondence to: Li-Min Huang, MD, PhD, Department of Pediatrics, National Taiwan University Hospital, 7, Chung-Shan South Road, Taipei 100, Taiwan. E-mail: lmhuang@ntu.edu.tw Received 14 May 2012; Accepted 22 August 2012. DOI 10.1002/ppul.22706 Published online 20 November 2012 in Wiley Online Library (wileyonlinelibrary.com). _ 2012