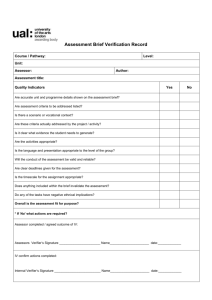
FAQs about mini - CEX and CbD
advertisement

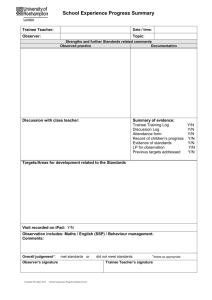
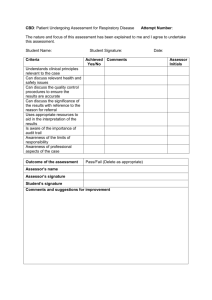
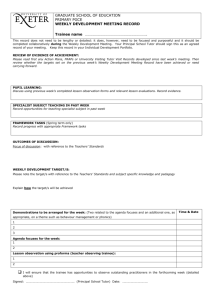
The Pharmacy Vocational Training Scheme Stage 2, 3 & 4 Frequently Asked Questions about mini-Clinical Evaluation (mini-CEX) and Case-based Discussion (CbD) Exercises Version 1.9 March 2014 Mini-Clinical Evaluation Exercise (mini-CEX) What is mini-CEX? Mini-CEX originated in the UK and has been used within medicine for years. It was adapted for use within pharmacy in 2006 and was introduced into the Pharmacy Vocational Training Scheme to enhance learning, in 2011?. A mini-CEX is a 15 – 20 minutes, observed, real-life, interaction between a trainee and a patient and/or doctor. The observer provides the trainee with immediate feedback on this interaction, focussing on the clinical skills, attitudes and behaviours of expected of the trainee. mini-CEX are suitable for use in a variety of situations normally expected of the trainee such as medicine reconciliation, discussing a TPN prescription with a doctor, receiving an MI enquiry on the ward or carrying out medication counselling with a patient e.g. warfarin counselling. Why use the mini-CEX? MiniCEX is time efficient way of assessing trainees in real practice setting and it presents a complete and realistic challenge to trainees. It allows trainees to get feedback on their performance from an experienced pharmacist about a real patient, in real time. Who is involved in the mini-CEX? It is the trainee’s responsibility to indentify and approach the appropriate pharmacist to be an assessor: e.g. the senior pharmacist specialising in the clinical area. Trainees are advised to arrange a time and date for the assessment in advance, and it is suggested that this is organised at the start of the trainee’s rotation. The trainee should not expect the assessment to be done immediately upon request. Where does the mini-CEX happen? The mini-CEX must be conducted in the clinical setting. How long will it last? The observation will take approximately 15 – 20 minutes, followed by immediate feedback. This may take approximately 30 – 60 minutes in total to complete. How many mini-CEX assessments need to be included in the ePortfolio? In total, trainees are expected to have at least 8 mini-CEXs in their portfolio. A minimum of one mini-CEX should be completed for each clinical rotation and should represent a range of different clinical problems and realistic challenges encountered throughout the training period. What happens during the mini-CEX? Time and date arrangement. The mini-CEX is driven by the trainee. Prior to the assessment, it is the trainee’s responsibility to approach the appropriate pharmacist and arrange a time for the assessment to be carried out. It is suggested that a date should be organised at the start of the trainee’s rotation. However, this is dependent on the rotation and workload of each senior pharmacist and sometimes trainees just need to grab an opportunity. However, this should not be the norm and trainees must appreciate the workload of assessors. 1|P a g e Patient selection. The assessor will accompany the trainee to their ward. The trainee will identify 3 previously unseen patients on the ward and the assessor will select one of these patients for the assessment. Understanding that patients might be in theatre or asleep at the time of assessment, a realistic approach should be undertaken. Trainee-patient interaction. In situations where pharmacist-patient interaction is being assessed (e.g. taking of drug history) the assessor should stand at a distance so that they can observe and hear the interaction (e.g. at the end of the patient’s bed). They should not interrupt the interaction with the patient unless they feel that the information being given is detrimental to patient care. Normal ward procedures should be followed by the pharmacist being assessed. The assessor will observe the trainee’s ability to deliver pharmaceutical care to the patient in real time. Trainee-assessor discussion. A discussion between trainee and assessor can be undertaken following a traineepatient interaction. The trainee will briefly present the clinical scenario to the assessor, highlighting key pharmaceutical issues and suggesting appropriate action plan. The discussion should be led by the trainee. The assessor, on the other hand, should practise a passive role in the discussion. The assessor can prompt the trainee using relevant questions to the clinical scenario to assess trainee’s understanding of the clinical scenario. However, the assessor should not dictate how the trainee should deliver the pharmaceutical care unless the action is detrimental to patient care. Trainee-doctor interaction. Similar to trainee-patient interaction, in situations where trainee’s interaction with other members of the multidisplinary team is involved, the assessor will observe the trainee’s ability to interact with other healthcare professionals to delivery pharmaceutical care to the patient in real time. Marking of the CEX form. Following the assessment, it is good to give the feedback as soon after the session as possible. Prior to the CEX a paper version of the form should be printed off and taken to the clinical area for scoring throughout the session. This way the feedback can be given straight after the session and then the assessor can either give the form to the trainee to upload into their Personal Library within their e Portfolio or the assessor can transfer the scores onto a mini CEX form that can be sent by the trainee using the ticketed feedback system. To use the ticketed feedback system the trainee needs to generate a new ticket after which the ‘Generate a New Ticket’ page will appear .The trainee should select the ‘Mini-CEX assessment form’ and fill in the assessor’s details. An email will then be sent to the assessor providing the login code for the assessor to use to ‘log into’ the ePortfolio and complete the ticketed mini-CEX assessment form. The assessment form should be filled in based on the trainee’s performance within each competency area using the rating scale. Feedback to the trainee. This should be done as soon as possible after the session. The assessor will provide feedback on skills essential to the provision of good pharmaceutical care. In keeping with the quality improvement assessment model, the assessor will highlight the trainee’s strengths, identify areas for development and together, the trainee and assessor will agree action points. Approximately two weeks after the mini-CEX, the trainee should meeting with their tutor or the assessor to briefly discuss learning outcomes from the agreed action points. 2|P a g e Feedback to the trainee. The assessor will provide feedback on skills essential to the provision of good pharmaceutical care. In keeping with the quality improvement assessment model, the assessor will highlight the trainee’s strengths, identify areas for development and together, the trainee and assessor will agree action points. Approximately two weeks after the mini-CEX, the trainee should meet with their tutor or the assessor to briefly discuss learning outcomes from the agreed action points. What competency areas will be assessed? The following competency areas will be assessed and the explanation for each competency area is as follows: Delivery of Patient Care 1. Patient consultation Introduction to patient, conducting a patient-centred consultation, exploring the medical/surgical condition with the patient, considering the patient’s own health beliefs, being aware of personal limitations and making appropriate referrals 2. Need for drug Establishing the patient’s background, taking a drug history and gaining the necessary information from a range of sources in order to decide on the appropriateness of drug therapy 3. Selection of the drug Appropriate consideration of evidence-based medicine and drug interactions (drug-drug, drug-disease, drug-patient) 4. Drug specific issues Checking that the drug is prescribed correctly (route, formulation, dose, frequency, course length) and considering available results and what effect they have on drug therapy e.g. U&Es, LFTs 5. Provision of drug product Implementing an effective system for the supply of medicines 6. Medicines information and patient education Provision of medicines and health advice to patients, carers, other pharmacy staff medical and nursing staff, and other healthcare professionals 7. Professionalism Identification and prioritisation of medicines management issues, time management, patient confidentiality, appropriate application of guidelines such as formulary, therapeutic switching policies etc Problem solving 8. Gathering information Accessing and summarising the information required and ensuring the information used is up-to-date 9. Knowledge Knowledge of pathophysiology of common medical/surgical conditions encountered, pharmacology, side effects and drug interactions 10.Analysing information Demonstrating the ability to evaluate information gathered (reliability or source, relevant to patient care), correctly identifying the problem, appraising options, making appropriate decisions and demonstrating a logical approach 11.Overall clinical care An assessment that summarises all of the above in terms of outcome for the patient 3|P a g e What rating scale will be used to access the trainee? The full range of the rating scale should be used and comparison made with what would be expected of any pharmacist at that stage of their vocational training. Trainees should aim for “meets expectations” although it is expected that some ratings will be below this. The key part of mini-CEX is effective feedback and identifying learning needs. Rating Scale Significantly below Performs poorly; very rarely meets the standard expected Below Performs poorly; meets the standard required occasionally Borderline Performs satisfactorily; with appropriate support and direction should meet expectations Meets expectations Performs well and to the standard expected of a pharmacist at that stage in their training Above Performs to a standard higher than what you would expect from a pharmacist at that stage in their training Significantly above Performs to an excellent standard; trainee is ahead of his/her peer group Unable to comment Unable to comment as performance not observed whilst s/he was there How can trainees and assessors learn to use the mini-CEX? Trainees and assessors can learn more about how to use the mini-CEX by viewing the JPB Assessment Tools DVD here. Case – based Discussion (CbD) What is CbD? CbD originated in the UK and has been used within medicine for years. It was adapted for use within pharmacy in 2006 by CoDEG (Competency Development & Evaluation Group) and was introduced into the Pharmacy Vocational Training Scheme to enhance learning, in 2012.CbD is a 20-30 minute discussion between the trainee and their tutor or assessor on a previous case. As with the mini-CEX this is designed to provide feedback clinical skills, problem solving skills and knowledge of trainees in relation to a real life situation. CbD is an assessesment of a trainee in relation to a retrospective patient case, which differentiates this from the miniCEX . CbD can be suitable for a wide range of cases such as discussing the pharmacokinetic or pharmacodynamics of a new drug for a patient, evidence base use of a drug in a particular patient, the legal or ethical issues around patient care, or even based on a patient that has been utilised for a mini-CEX. 4|P a g e Why use the CbD? The CbD allows trainees and their tutor / assessor to discuss previous patient cases in a retrospective view. The assessor can observe how the trainee utilises their problem solving skills and enhance learning by encouraging ref lection. It is not the assessor’s role to interrogate the trainee about the case but to ask questions related to the competencies expected and to assess the trainee’s strengths and weaknesses. Who is involved in the CbD? It is the trainee’s responsibility to indentify and approach the appropriate pharmacist to be an assessor: e.g. the senior pharmacist specialising in the clinical area. Trainees are advised to arrange a time and date for the assessment in advance, and it is suggested that this is organised at the start of the trainee’s rotation. The trainee should not expect the assessment to be done immediately upon request. Where does the CbD happen? The CbD can be conducted in the ward or at a suitable location. The most appropriate place would be somewhere quiet where there will be minimal disruption. How long will the CbD last? The CbD may take approximately 20 minutes but this will depend on the case being discussed. It should not take any longer than an hour. How many CbD assessments need to be included in the e Portfolio? A minimum of one CbD should be completed for each clinical rotation and should represent a range of different clinical problems and realistic challenges encountered throughout the training period. Throughout the training period trainees are expected to complete at least 8 CbDs What happens during the CbD? Time and date arrangement: The CbD is driven by the trainee. Prior to the assessment, it is the trainee’s responsibility to approach the appropriate pharmacist and arrange a time for the assessment to be carried out. It is suggested that a date should be organised at the start of the trainee’s rotation. However, this is dependent on the rotation and workload of each senior pharmacist. Patient selection: The trainee should choose and share three cases which they have prepared in advance and the assessor should select one of these case for the CbD assessment. A previous miniCEX can be used for a CbD. Trainee-assessor discussion: The trainee may bring patient notes, drug charts and other details to help them to discuss their case. The trainee should start the discussion by outlining the key points of the case to the assessor. They should then also highlight the key pharmaceutical care issues and the rationale for the treatment and the care that they provided. After this the assessor should take over the discussion and question the trainee to check if they have fulfilled the assessment criteria. Details of the criteria are on the CbD Form. After this the assessor should give verbal feedback and formal written feedback (using the CbD Form) after the meeting. 5|P a g e The most vital part of the CbD is the feedback given by the assessor to the trainee. The assessor should provide feedback on skills essential to the provision of good pharmaceutical care. In keeping with the quality improvement assessment model, the assessor should highlight the trainee’s strengths, identify areas for development and together, the trainee and assessor should agree action points. Approximately two weeks after the CbD, the trainee should meet with their tutor or the assessor to briefly discuss learning outcomes from the agreed action points. Marking of the CbD: Following the assessment, the trainee should send a CbD assessment form to the assessor from their ePortfolio. To do this, the trainee should log into the ePortfolio, select ‘Learning and Reflection Logs’ from the dropdown menu under ‘Logs’. In the ‘Learning and Reflection Logs’ page, they should then click on the ‘Request Ticket’ tab on the top right corner as depicted below. Subsequently, a ‘Generate a New Ticket’ page will appear and the trainee should select ‘CbD assessment form’ and fill in the information of the assessor. An email will then be sent to the assessor providing the login code for the assessor to log into the ePortfolio to fill up the ticketed mini-CEX assessment form. The assessment form should be filled in based on the trainee’s performance within each competency area using the rating scale. What competency areas will be assessed? The following competency areas will be assessed and the explanation for each competency area is as follows: 6|P a g e Pharmaceutical Needs Assessment / Identification and prioritisation of care issues. Pharmacist has identified correctly the pharmaceutical care issues for patient. The trainee is able to prioritise the pharmaceutical care issues appropriately. Treatment Recommendations Can discuss the treatment of the main medical problem – evidence-based treatment guidelines, drug therapy (mechanism of action of drugs, dosage range, key pharmacokinetic data, cautions, contra-indications, common side effects, major drug interactions, patient counselling points). Patient Monitoring and follow up Can discuss the rationale for the monitoring of the patient’s pharmaceutical care. Can demonstrate practical ongoing and appropriate monitoring of therapy (including kardexes as well as biochemistry, haematology) Can discuss and demonstrate how the care of this patient was managed in conjunction with the wider healthcare team Professionalism Demonstrates ability to prioritise; and was timely and succinct. Can show an ethical approach, and awareness of any relevant legal frameworks. Has insight into own limitations. Considers interface issues. Overall Clinical Judgement Can discuss own judgement , synthesis, caring and effectiveness for this patient What rating scale will be used to assess the trainee? The full range of the rating scale should be used and comparison made with what would be expected of a pharmacist at that stage of their vocational training. Trainees should aim for “meets expectations” although it is expected that some ratings will be below this. The key part of CbD is effective feedback and identifying learning needs. Rating Scale Significantly below Performs poorly; very rarely meets the standard expected Below Performs poorly; meets the standard required occasionally 7|P a g e Borderline Performs satisfactorily; with appropriate support and direction should meet expectations Meets expectations Performs well and to the standard expected of a pharmacist at that stage in their training Above Performs to a standard higher than what you would expect from a pharmacist at that stage in their training Significantly above Performs to an excellent standard; trainee is ahead of his/her peer group Unable to comment Unable to comment as performance not observed whilst s/he was there How can trainees and assessors learn to use the CbD? Trainees and assessors can learn more about how to use the CbD by viewing the JPB Assessment Tools DVD here. Is there a pass or fail mark issued for the mini-CEX and CbD assessments? There is no pass or fail grade associated with these tools but they are rated instead. These assessments are utilised to portray to the trainee how their current performance is and then improving through the feedback given by the tutor/assessor. What are the main differences between the miniCEX and CbD? Though they are both orientated around feedback from the tutor/assessor and then developing an action plan to improve the performance as a trainee, there are differences in the format of the assessment process and the criteria for assessment. In a mini-CEX, the assessor is able to assess the trainee’s practice in the clinical area where as in a CbD the assessor can only assess the trainee’s current knowledge and decision making and facilitate their further learning. In the miniCEX the assessor observes the trainee’s performance in the ward area in real time. The assessor observes the trainee’s interaction with the patient or other health care staff. In a CbD, the trainee and assessor a previously prepared clinical case in a quiet, private area. The CbD assessor may be different to the assessor for the mini--CEX and so they may not have assessed the trainee’s attitude or interpersonal skills. The assessor will ask probing questions which will require a more detailed explanation of the care issues compared to the questions asked in a miniCEX. 8|P a g e