The frequency of nasal foreign bodies is not known.
advertisement

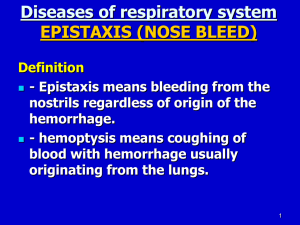
Foreign Bodies, Nose Jonathan I Fischer, MD, Staff Physician, Department of Emergency Medicine, Yale New Haven Hospital Asim Tarabar, MD, Assistant Professor, Department of Surgery, Section of Emergency Medicine, Yale University School of Medicine; Consulting Staff, Department of Emergency Medicine, Yale-New Haven Hospital Contributor Information and Disclosures Updated: Sep 15, 2008 Print This Email This Introduction Background Nasal foreign bodies (NFBs) are commonly encountered in emergency departments. Although more frequently seen in the pediatric setting, they can also affect adults, especially those with mental retardation or psychiatric illness. Children's interests in exploring their bodies make them more prone to lodging foreign bodies in their nasal cavities. In addition, they may also insert foreign bodies to relieve preexisting nasal mucosal irritation or epistaxis. As benign as a nasal foreign body may seem, it harbors the potential for morbidity and even mortality if the object is dislodged into the airway. Foreign bodies can be classified as either inorganic or organic. Inorganic materials are typically plastic or metal. Common examples include beads and small parts from toys. These materials are often asymptomatic and may be discovered incidentally. Organic foreign bodies, including food, rubber, wood, and sponge, tend to be more irritating to the nasal mucosa and thus may produce earlier symptoms. The most common locations for nasal foreign bodies to lodge are just anterior to the middle turbinate or below the inferior turbinate. Unilateral foreign bodies affect the right side about twice as often compared to the left. This may be due to a preference of right-handed individuals to insert objects in their right naris. Pathophysiology Nasal foreign bodies can cause damage to the nasal cavity and surrounding structures. They can produce local inflammation, which may result in a pressure necrosis. This, in turn, can cause mucosal ulceration and erosion into blood vessels producing epistaxis. The swelling can cause obstruction to sinus drainage and lead to a secondary sinusitis. Organic foreign bodies tend to swell and are usually more symptomatic than inorganic foreign bodies. Firmly impacted and unrecognized foreign bodies can in time become coated with calcium, magnesium, phosphate, or carbonate and become a rhinolith. Rhinoliths are radio-opaque and typically are found on the floor of the nasal cavity. Rhinoliths can remain undetected for years and only upon growth do they produce symptoms that lead to their discovery. In comparison to foreign bodies in the ear, NFBs often fail to be recognized for longer periods of time because they usually produce fewer symptoms and are more difficult to visualize. Button batteries, magnets, and living foreign bodies can be particularly destructive and are further discussed below (see Special Considerations). All foreign bodies harbor the potential for swallowing or airway obstruction if displaced posteriorly. Frequency The frequency of nasal foreign bodies is not known. Morbidity/Mortality The foreign body itself may cause irritation to the patient; however, morbidity is primarily caused by the resulting inflammation, mucosal damage, and extension into adjacent structures. Reported complications include sinusitis, acute otitis media, nasal septal perforation, periorbital cellulitis, meningitis, acute epiglottitis, diphtheria, and tetanus. Race The prevalence of nasal foreign bodies by race is not known. Sex Some studies have demonstrated greater prevalence in males than in females (ie, 58% males1); however, this trend has not been universal. Age Among children, those aged 2-5 years have the highest incidence of NFBs. Children develop their pincer grip at about 9 months of age; in theory, this would be necessary for most cases of NFB insertion. Clinical History In most cases, the insertion of the nasal foreign body (NFB) is witnessed, and the dilemma of diagnosis is eliminated. In one study, presentations over 48 hours after the time of insertion accounted for 14% of all cases.2 In addition to obtaining a thorough history from the patient and his or her primary guardian(s), it is important to interview all caretakers that have recently spent time with the patient (ie, babysitters, counselors). Once the diagnosis is missed, the foreign body may not be detected for days, weeks, or even years. Among the delayed presentations, the most common clinical scenario is unilateral nasal discharge. Nevertheless, clinicians must entertain the diagnosis of NFB in all patients with nasal irritation, epistaxis, sneezing, snoring, sinusitis, stridor, wheezing, or fever. Some authors even report discovering NFBs as the etiology of more unusual patient presentations, such as irritability, halitosis, or generalized bromhidrosis (body malodor). Failure to recognize “occult” nasal foreign bodies can allow persistence for years inside a patient’s nasal cavity. To avoid complications and delayed treatment, clinicians must maintain a high index of suspicion for this diagnosis. Physical The physical examination is the main diagnostic tool, and a cooperative patient is essential for success. Parents and staff may be needed to comfort and immobilize a child to allow for a thorough otorhinolaryngologic examination. Sedation is often helpful in the pediatric population. Maximal visualization of the nasal cavity is obtained by wearing a head-lamp. Some authors recommend positioning children younger than 5 years in a supine lying position and older children in a sitting "sniffing" position to allow optimal visualization. A nasal speculum may also help to view the nasal cavity, although some authors report less patient anxiety and equally good visualization by using one's thumb to pull the nose upward. In addition to adequate inspection of the nasal cavity, assessing for complications of the nasal foreign body is important. Visualize the tympanic membranes for signs of acute otitis media, assess for sinusitis, check for nuchal rigidity in the toxic child, and auscultate the chest and neck for wheezing or stridor, which may be a clue of foreign body aspiration. Lastly, looking for additional foreign bodies, whether they are in the nose or other body cavities, is important. Differential Diagnosis Epistaxis Sinusitis Polyps Tumor Upper respiratory infection (URI) Unilateral choanal atresia Workup The extent of the workup depends on the clinical scenario. For most isolated nasal foreign bodies, no diagnostic testing is indicated. With the exception of metallic or calcified objects, most nasal foreign bodies (NFBs) are radiolucent. When an alternate diagnosis (ie, tumor, sinusitis) is being considered, imaging (ie, CT scan) may be helpful. On the other hand, if concern for an ingested or aspirated foreign body exists, radiography of the chest/abdomen should be performed. An aspirated radiolucent foreign body may be inferred by postobstructive air trapping, and an ingested foreign body will show up if it is radiopaque, as most ingested foreign bodies are. Treatment Planning/Pretreatment Repeated attempts at nasal foreign body (NFB) removal are likely to be successively more difficult, and the object may become more deeply lodged. Therefore, careful planning is important to maximize the likelihood of removal on the first attempt. Having the necessary instruments at the bedside is essential, as is the clinician's knowledge of several techniques. In addition, emergency airway supplies should be readily available in the event that manipulation of the foreign body results in aspiration. Pharmacological vasoconstriction of the nasal mucosa can facilitate both examination and removal of a NFB. Anesthesia and mucosal vasoconstriction can be accomplished by applying several drops of 1% lidocaine (without epinephrine) and 0.5% phenylephrine to the affected nostril. For the apprehensive patient, a nebulized solution of 1-2 mL of 1:1000 epinephrine has been used successfully for mucosal vasoconstriction. Of note, the author of the nebulized epinephrine case report only recommends its use if the NFB is large enough that posterior movement is unlikely and if the practitioners are experts at securing airways. Specific Removal Techniques Several removal techniques are available, and the choice of a particular method depends upon the NFB type, the supplies available, and the clinician's comfort with each method. For easily visualized nonspherical and nonfriable objects, most clinicians prefer direct instrumentation. If the object is poorly visualized, spherical, or unsuccessfully removed by direct instrumentation, balloon-catheter removal is a preferred method. For large, occlusive NFBs, positive pressure techniques are commonly used. All attempts at removal can be complicated by mucosal damage and bleeding. In addition, all failed attempts can result in posterior displacement of the NFB. Each method is described below. Direct instrumentation This technique is ideal for easily visualized, nonspherical, and nonfriable foreign bodies. Previously described instruments include hemostats, alligator forceps, or bayonet forceps. Friable and spherical foreign bodies are particularly difficult to remove by this technique: friable objects may tear, and spherical objects may be difficult to grasp and result in posterior displacement. In addition, hooked probes (ie, right-angle hook) can be used for objects that are easily visualized but difficult to grasp. The hook is placed behind the NFB and then rotated so the hook angle is behind the bulk of the object. The object is then pulled forward. Interestingly, some authors have suggested using the combination of direct instrumentation to grasp an object while having a balloon catheter (see next paragraph) placed behind the object to prevent posterior displacement during removal attempts. Balloon catheters This approach is ideal for small, round objects that are not easily grasped by direct instrumentation. Authors have used Foley catheters (ie, 5, 6, or 8) or Fogarty catheters (ie, #6 biliary or #4 vascular), and the Katz Extractor oto-rhino foreign body remover (InHealthTechnologies, CA) is also an option. The biliary Fogarty catheter has been preferred over the vascular Fogarty catheter by some authors because its balloon is firmer and theoretically less prone to rupture. Regardless of catheter type, the technique is similar. First, the balloon is inspected, and the catheter is coated with 2% lidocaine jelly. Then, it is inserted past the foreign body and inflated with air or water (2 mL in small children and 3 mL in larger children). After inflation, the catheter is withdrawn, pulling the foreign body with it. Positive pressure Large and occlusive foreign bodies are especially amenable to the positive pressure technique. Several techniques have been developed to expel the NFB out by force provided in the form of positive pressure. The least invasive form, "forced exhalation," can be accomplished by occluding the unaffected nostril and asking the child to blow hard out his or her nose. If this fails, the positive pressure can be applied by either the parent's mouth ("parent's kiss"3) or a bag-valve-mask. With either method, a tight seal is formed around the child's mouth, while avoiding the nose. The unaffected nostril is then occluded, and a forceful puff of air is provided. If these techniques do not completely remove the object, they may at least dislodge the object more anteriorly and allow for removal using the previously described techniques. Another positive pressure technique delivers air into the unaffected naris with the patient's mouth closed. In this technique, the patient is placed on his or her side (foreign body side down), and the delivery device (known as a "Beamsley Blaster") provides high-flow oxygen (10-15 L/min) into the unaffected naris. To set up the Beamsley Blaster, one end of oxygen tubing connects to the oxygen source and the other end is connected to a male-male oxygen tube adaptor that is placed in the patient's unaffected naris. A potential complication unique to positive pressure techniques is barotrauma to the lungs or the tympanic membranes. However, to date, no cases of this have been reported. Suction This technique is ideal for easily visualized smooth or spherical foreign bodies. The catheter tip is placed against the object, and suction is turned on to 100-140 mm Hg (readily supplied by standard medical suction equipment). A strong seal is important for success of this technique, and authors have recommended using a Schunkt-neck catheter with its plastic umbrella tip or a Frazier catheter with a segment of pliable tubing connected to its tip for a strong seal with the foreign body. Glue This method is ideal for easily visualized smooth or spherical foreign bodies that are dry and nonfriable. A thin coat of cyanoacrylate adhesive is placed on the tip of a wooden or plastic applicator, which is then pressed against the foreign body for 60 seconds and removed. Without full cooperation of the patient, the nasal mucosa is easily injured by misplaced glue. Posterior displacement Rarely, a foreign body may be so posterior that the above techniques will not work. In these cases, after consultation with a specialist, it may be necessary to induce further posterior displacement of the object into the oropharynx for removal. Of course, this would require general anesthesia, endotracheal intubation, and esophageal occlusion. Magnet A case report demonstrated successful removal of a loose ball bearing from a nasal cavity using a household magnet.4 The authors believe that a strong magnet may be especially useful to remove button batteries, which are associated with mucosal edema and significant bleeding with direct instrumentation, making visualization especially difficult. Irrigation This technique has been strongly criticized for carrying a significant risk of aspiration or choking. The authors do not recommend use of this method; however, it will be reviewed so that clinicians can be aware of its existence. The irrigation technique is performed by forceful squeezing of a bulb syringe filled with 7 mL of normal saline into the unaffected naris. For excellent patient education resources, visit eMedicine's Ear, Nose, and Throat Center. Also, see eMedicine's patient education article Foreign Body, Nose. Special Considerations Metallic button batteries: Metallic button batteries are small and shiny and found in many toys making them strong candidates for nasal foreign body (NFB) insertion. Once inserted into the nose, they cause destruction by low-voltage electrical currents, electrolysis-induced release of sodium hydroxide and chlorine gas, and even liquefactive necrosis if their alkaline contents leak out. Complications from button batteries are relatively common, occurring in 6 of 11 cases reviewed in one series.5 In addition, they can occur rapidly, as discussed by Gomes et al, which reported nasal cavity burns from a battery that was in a nose for only 12 hours.6 Button batteries require prompt removal and a thorough inspection of the nasal cavity for complications. It is particularly important not to irrigate the nasal cavities to avoid spreading alkaline content that may have leaked out.6 Magnetic NFBs: Small magnets have been used recreationally as imitation earrings as well as therapeutically for splinting after septoplasty. In the literature, magnetic NFBs have been shown to cause pressure necrosis and even perforation of the nasal septal mucoperichondrium. Therefore, they require prompt removal. Living NFBs: Larvae and worms have been known to occasionally inhabit the nasal cavities of those living in tropical and unhygienic environments. They can lead to destruction of the nasal mucosa and subsequent necrosis of septal cartilage and turbinates. Some authors have even reported extension to the orbit and paranasal sinuses. Because of the invasive nature of these NFBs, treatment typically consists of instillation of an agent to kill the larvae or worm, followed by surgical debridement and antibiotic therapy. These cases should be managed in conjunction with a specialist. Miscellaneous Consultation In general, nasal foreign bodies can be safely removed by emergency physicians. However, an otolaryngological specialist should be promptly consulted for cases of failed removal or a NFB complicated by significant damage to adjacent structures. A nonemergent referral to a specialist be should made when there is concern for a tumor or mass. Medical/Legal Pitfalls It is crucial to have the supplies and staff needed to deal with an airway emergency during manipulation of the NFB. Failure to consult a specialist when managing an NFB complicated by significant damage to nasopharynx (ie, button battery content leakage) is a pitfall. Delay in diagnosis of complications of nasal foreign bodies, such as sinusitis and acute otitis media, can result in prolonged morbidity. This can be avoided by performing a thorough examination and by reexamining the nasal cavity after removal of the NFB. Failure to search for additional foreign bodies in patients found to have one NFB is a pitfall. Failure to contact a specialist when a tumor or mass is suspected can result in delayed diagnosis of a malignancy. Foreign Bodies, Ear Rate this Article Email to a Colleague Last Updated: February 20, 2006 Synonyms and related keywords: foreign objects in the ear, object in ear canal, object in ear, ear pain, hearing loss, tympanic membrane perforation, ear problems, ear foreign body AUTHOR INFORMATION Section 1 of 9 Author Information Introduction Clinical Differential Diagnosis Workup Treatment Medications Miscellaneous Bibliography Author: Robin Mantooth, MD, Consulting Staff, Department of Emergency Medicine, Integris Southwest Medical Center Robin Mantooth, MD, is a member of the following medical societies: American College of Emergency Physicians, and Christian Medical and Dental Society Editor(s): Edmond Hooker, MD, Assistant Clinical Professor, Department of Emergency Medicine, University of Louisville, Wright State University; Francisco Talavera, PharmD, PhD, Senior Pharmacy Editor, eMedicine; Mark W Fourre, MD, Program Director, Department of Emergency Medicine, Maine Medical Center, Associate Clinical Professor, Department of Surgery, University of Vermont School of Medicine; John Halamka, MD, Chief Information Officer, CareGroup Healthcare System, Assistant Professor of Medicine, Department of Emergency Medicine, Beth Israel Deaconess Medical Center; Assistant Professor of Medicine, Harvard Medical School; and Steven C Dronen, MD, FAAEM, Director of Emergency Services, Director of Chest Pain Center, Department of Emergency Medicine, Ft Sanders Sevier Medical Center Disclosure INTRODUCTION Section 2 of 9 Author Information Introduction Clinical Differential Diagnosis Workup Treatment Medications Miscellaneous Bibliography Foreign bodies of the ear are relatively common in emergency medicine. They are seen most often but not exclusively in children. Various objects may be found, including toys, beads, stones, folded paper, and biologic materials such as insects or seeds. CLINICAL Section 3 of 9 Author Information Introduction Clinical Differential Diagnosis Workup Treatment Medications Miscellaneous Bibliography History Most adults are able to tell the examiner that there is something in their ear, but this is not always true. For example, an older adult with a hearing aid may lose a button battery or hearing aid in their canal and not realize it. Children, depending on age, may be able to indicate that they have a foreign body, or they may present with complaints of ear pain or discharge. Patients may be in significant discomfort and complain of nausea or vomiting if a live insect is in the ear canal. Patients may present with hearing loss or sense of fullness. Physical: The physical examination is the main diagnostic tool. Physical findings vary according to object and length of time it has been in the ear. An inanimate object that has been in the ear a very short time typically presents with no abnormal finding other than the object itself seen on direct visualization or otoscopic examination. Pain or bleeding may occur with objects that abrade the ear canal or rupture the tympanic membrane, or from the patient's attempts to remove the object. Hearing loss may be noted. With delayed presentation, erythema and swelling of the canal and a foul-smelling discharge may be present. Insects may injure the canal or tympanic membrane by scratching or stinging. Causes A patient, caretaker, or sibling intentionally places an object in the ear canal and is unable to remove it. Insects may crawl or fly into the ear. DIFFERENTIAL DIAGNOSIS Section 4 of 9 Author Information Introduction Clinical Differential Diagnosis Workup Treatment Medications Miscellaneous Bibliography Abrasions to ear canal Cerumen impaction Hematoma Otitis externa Tumor Tympanic membrane perforation WORKUP Section 5 of 9 Author Information Introduction Clinical Differential Diagnosis Workup Treatment Medications Miscellaneous Bibliography No specific lab or radiologic studies are recommended. The physical examination is the main diagnostic tool. Use an otoscope while retracting the pinna in a posterosuperior direction. A head mirror with a strong light source, operating otoscope, or operating microscope also may be used. Refractory objects may require extraction by an ear, nose, and throat (ENT) specialist. TREATMENT Section 6 of 9 Author Information Introduction Clinical Differential Diagnosis Workup Treatment Medications Miscellaneous Bibliography Prehospital care: No specific prehospital treatment exists other than transport to a hospital. Occasionally, treating significant pain or nausea may be necessary. Emergency department care: Patients in extreme distress secondary to an insect in the ear require prompt attention. The insect should be killed prior to removal, using mineral oil or lidocaine (2%). Methods of removal Irrigation is the simplest method of foreign body removal, provided the tympanic membrane is not perforated. An electric ear syringe, available in some areas, may be very helpful for irrigation. Use of the commercial product Waterpik is not recommended because the high pressure it generates may perforate the tympanic membrane. Irrigation with water is contraindicated for soft objects, organic matter, or seeds, which may swell if exposed to water. Suction is sometimes a useful means of foreign body removal. Suction the ear with a small catheter held in contact with the object. Grasp the object with alligator forceps. Place a right-angled hook behind the object and pull it out. Avoid any interventions that push the object in deeper. The physician may need to sedate the patient to attempt removal of the object. Use mild sedation following a procedural sedation protocol. Special instances Cyanoacrylate adhesives (eg, Superglue) may be removed manually within 24-48 hours once desquamation occurs. If adhesive touches the tympanic membrane, remove it more carefully and refer patient to an ENT specialist. Remove batteries immediately to prevent corrosion or burns. Do not crush battery during removal. Consultations Consult an ENT specialist if the object cannot be removed or if tympanic membrane perforation is suspected. Patient Education For excellent patient education resources, visit eMedicine's Ear, Nose, and Throat Center. Also, see eMedicine's patient education article Foreign Body, Ear. MEDICATIONS Section 7 of 9 Author Information Introduction Clinical Differential Diagnosis Workup Treatment Medications Miscellaneous Bibliography After the foreign body is removed, fill the ear canal 5 times/day for 5-7 days with a combination antibiotic and steroid otic suspension (eg, Cortisporin). MISCELLANEOUS Section 8 of 9 Author Information Introduction Clinical Differential Diagnosis Workup Treatment Medications Miscellaneous Bibliography Medical/Legal Pitfalls Failure to consider diagnosis when typical history is not given (eg, older patients) Failure to prevent further damage when attempting to remove the object, especially when the object is next to the tympanic membrane Failure to diagnose serious damage to ossicles, retained middle ear foreign body, or perilymphatic leak. Failure to diagnose bilateral foreign bodies. Failure to provide appropriate follow-up for people with chronic ear problems Epistaxis Last Updated: July 19, 2005 Synonyms and related keywords: nasal hemorrhage, nosebleed, nose bleed, bloody nose AUTHOR INFORMATION Section 1 of 10 Author Information Introduction Clinical Differentials Workup Treatment Medication Follow-up Miscellaneous Bibliography Author: Jeffrey Evans, MD, Consulting Staff, Clinical Instructor of Emergency Medicine, Department of Emergency Medicine, Mount Auburn Hospital Coauthor(s): Todd Rothenhaus, MD FACEP, Director of Medical Informatics, Assistant Professor of Emergency Medicine, Department of Emergency Medicine, Boston University School of Medicine Jeffrey Evans, MD, is a member of the following medical societies: American College of Emergency Physicians Editor(s): Francis Counselman, MD, Program Director, Chair, Professor, Department of Emergency Medicine, Eastern Virginia Medical School; Francisco Talavera, PharmD, PhD, Senior Pharmacy Editor, eMedicine; Mark W Fourre, MD, Program Director, Department of Emergency Medicine, Maine Medical Center, Associate Clinical Professor, Department of Surgery, University of Vermont School of Medicine; John Halamka, MD, Chief Information Officer, CareGroup Healthcare System, Assistant Professor of Medicine, Department of Emergency Medicine, Beth Israel Deaconess Medical Center; Assistant Professor of Medicine, Harvard Medical School; and Steven C Dronen, MD, FAAEM, Director of Emergency Services, Director of Chest Pain Center, Department of Emergency Medicine, Ft Sanders Sevier Medical Center Disclosure INTRODUCTION Section 2 of 10 Author Information Introduction Clinical Differentials Workup Treatment Medication Follow-up Miscellaneous Bibliography Background: Epistaxis is defined as acute hemorrhage from the nostril, nasal cavity, or nasopharynx. It is a frequent ED complaint and often causes significant anxiety in patients and clinicians. However, more than 90% of patients who present to the ED with epistaxis may be successfully treated by an emergency physician (EP). Pathophysiology: Epistaxis is classified on the basis of the primary bleeding site as anterior or posterior. Hemorrhage is most commonly anterior, originating from the nasal septum. A common source of anterior epistaxis is the Kiesselbach plexus, an anastomotic network of vessels on the anterior portion of the nasal septum. Anterior bleeding may also originate anterior to the inferior turbinate. Posterior hemorrhage originates from branches of the sphenopalatine artery in the posterior nasal cavity or nasopharynx. Frequency: In the US: Epistaxis occurs in 1 of every 7 people. Mortality/Morbidity: Mortality is rare and is usually due to complications from hypovolemia, with severe hemorrhage or underlying disease states. Increased morbidity is associated with nasal packing. Posterior packing can potentially cause airway compromise and respiratory depression. Packing in any location may lead to infection. Sex: No sex predilection exists. Age: Bimodal incidence exists, with peaks in those aged 2-10 years and 50-80 years. CLINICAL Section 3 of 10 Author Information Introduction Clinical Differentials Workup Treatment Medication Follow-up Miscellaneous Bibliography History: Controlling significant bleeding or hemodynamic instability should take precedence over obtaining a lengthy history. Note the duration of the hemorrhage and the side of initial bleeding. Inquire about previous epistaxis, hypertension, hepatic or other systemic disease, easy bruising, or prolonged bleeding after minor surgical procedures. Recurrent episodes of epistaxis, even if selflimited, should raise suspicion for significant nasal pathology. Use of medications, especially aspirin, nonsteroidal anti-inflammatory drugs (NSAIDs), warfarin, heparin, ticlopidine, and dipyridamole should be documented, as these not only predispose to epistaxis but make treatment more difficult. Nausea is a possible symptom. Physical: Approximately 90% of nosebleeds can be visualized in the anterior portion of the nasal cavity. Massive epistaxis may be confused with hemoptysis or hematemesis. Blood dripping from the posterior nasopharynx confirms a nasal source. Perform a thorough and methodical examination of the nasal cavity. o Blowing the nose decreases the effects of local fibrinolysis and removes clots, permitting a better examination. Application of a vasoconstrictor prior to the examination may reduce hemorrhage and help to pinpoint the precise bleeding site. Topical application of a local anesthetic reduces pain associated with the examination and nasal packing. o Gently insert a nasal speculum and spread the naris vertically. This permits visualization of most anterior bleeding sources. A posterior source is suggested by failure to visualize an anterior source, by hemorrhage from both nares, and by visualization of blood draining in the posterior pharynx. Causes: Most cases of epistaxis do not have an easily identifiable cause. Local trauma (ie, nose picking) is the most common cause, followed by facial trauma, foreign bodies, nasal or sinus infections, and prolonged inhalation of dry air. A disturbance of normal nasal airflow, as occurs in a deviated nasal septum, may also be a cause of epistaxis. Iatrogenic causes include nasogastric and nasotracheal intubation. Children usually present with epistaxis due to local irritation or recent upper respiratory infection (URI). Oral anticoagulants and coagulopathy due to splenomegaly, thrombocytopenia, platelet disorders, or AIDS-related conditions predispose to epistaxis. The relationship between hypertension and epistaxis is implicated. Epistaxis is more common in hypertensive patients, and patients are more likely to be acutely hypertensive during an episode of epistaxis. Hypertension, however, is rarely a direct cause of epistaxis, and therapy should be focused on controlling hemorrhage before blood pressure reduction. Epistaxis is more prevalent in dry climates and during cold weather. Vascular abnormalities that contribute to epistaxis may include the following: o Sclerotic vessels o Hereditary hemorrhagic telangiectasia o Arteriovenous malformation o Neoplasm o Septal perforation, deviation o Endometriosis DIFFERENTIALS Section 4 of 10 Author Information Introduction Clinical Differentials Workup Treatment Medication Follow-up Miscellaneous Bibliography Barotrauma Disseminated Intravascular Coagulation Endometriosis Foreign Bodies, Nose Hemophilia, Type A Hemophilia, Type B Plant Poisoning, Glycosides - Coumarin Sinusitis Toxicity, Cocaine Toxicity, Nonsteroidal Anti-inflammatory Agents Toxicity, Rodenticide Toxicity, Salicylate Toxicity, Warfarin and Superwarfarins Other Problems to be Considered: Chemical irritants Hepatic failure Leukemia Osler-Weber-Rendu syndrome Rhinitis Thrombocytopenia Heparin toxicity Ticlopidine toxicity Dipyridamole toxicity Trauma Tumor WORKUP Section 5 of 10 Author Information Introduction Clinical Differentials Workup Treatment Medication Follow-up Miscellaneous Bibliography Lab Studies: The following laboratory studies are recommended in the presence of major bleeding or if a coagulopathy is suspected: o Obtain a hematocrit count and type and cross if a history of persistent heavy bleeding is present. o Obtain a complete blood count (CBC) if a history of recurrent epistaxis, a platelet disorder, or neoplasia is present. o The bleeding time is an excellent screening test if suspicion of a bleeding disorder is present. o Obtain the international normalized ratio (INR)/prothrombin time (PT) if the patient is taking warfarin or if liver disease is suspected. Imaging Studies: Sinus films are rarely indicated. Other Tests: CT scanning and/or nasopharyngoscopy may be performed if a tumor is the suspected cause of bleeding. Angiography is rarely indicated. TREATMENT Section 6 of 10 Author Information Introduction Clinical Differentials Workup Treatment Medication Follow-up Miscellaneous Bibliography Emergency Department Care: Upon initial arrival to the ED, patients should be instructed to grasp and pinch their entire nose, maintaining continuous pressure for at least 10 minutes. Gowns, gloves, and protective eyewear should be worn. Adequate light is best provided by a headlamp with an adjustable narrow beam. Patients should be positioned comfortably in a seated position, holding a basin under their chin. As always, first address the patient's airway, breathing, and circulation (ABCs). Severe epistaxis may require endotracheal intubation. Rapid control of massive bleeding is best secured with an epistaxis balloon or Foley catheter, as outlined below. Patients with significant hemorrhage should receive an IV line and crystalloid infusion, as well as continuous cardiac monitoring and pulse oximetry. Patients frequently present with an elevated blood pressure; however, a significant reduction can usually be obtained with analgesia and mild sedation alone. Specific antihypertensive therapy is rarely required and should be avoided in the setting of significant hemorrhage. Insert pledgets soaked with an anesthetic-vasoconstrictor solution into the nasal cavity to anesthetize and shrink nasal mucosa. Soak pledgets in 4% topical cocaine solution or a solution of 4% lidocaine and topical epinephrine (1:10,000) and place them into the nasal cavity. Allow them to remain in place for 10-15 minutes. If a bleeding point is easily identified, gentle chemical cautery may be performed after the application of adequate topical anesthesia. The tip of a silver nitrate stick is rolled over mucosa until a grey eschar forms. To avoid septal necrosis or perforation, only one side of the septum should be cauterized at a time. To be effective, cautery should be performed after bleeding is controlled. If attempts to control hemorrhage with pressure or cautery fail, the nose should be packed. Options include traditional nasal packing, a prefabricated nasal sponge, or an epistaxis balloon. o Traditional (Vaseline gauze) packing: This traditional method of anterior nasal packing has been supplanted by readily available and more easily placed tampon and balloons. It is commonly performed incorrectly, using an insufficient amount of packing placed primarily in the anterior naris. Placed in this way, the gauze serves as a plug rather than as a hemostatic pack. Physicians inexperienced in proper placement of a gauze pack should use a nasal tampon or balloon. The proper technique for placement of a gauze pack is as follows: 1. Grasp the gauze ribbon, about 6 inches from its end, with bayonet forceps. Place it in the nasal cavity as far back as possible, ensuring that the free end protrudes from the nose. On the first pass, the gauze is pressed onto the floor of nasopharynx with closed bayonets. 2. Next, grasp the ribbon about 4-5 inches from the nasal alae and reposition the nasal speculum so that the lower blade holds the ribbon against lower border of nasal alae. Bring a second strip into the nose and press downward. 3. Continue this process, layering the gauze from inferior to superior until the naris is completely packed. Both ends of ribbon must protrude from the naris and should be secured with tape. If this does not stop the bleeding, consider bilateral nasal packing. o Compressed sponge (Merocel): Trim the sponge to fit snugly through the naris. Moisten the tip with surgical lubricant or topical antibiotic ointment. Firmly grasp the length of the sponge with bayonet forceps, spread the naris vertically with a nasal speculum, and advance the sponge along the floor of the nasal cavity. Once wet with blood or a small amount of saline, the sponge expands to fill the nasal cavity and tamponade bleeding. o Anterior epistaxis balloons: Anterior epistaxis balloons may come in different lengths but have only one chamber. Cover the balloon with antibiotic ointment or lubricate it with water, insert it along the floor of the nasal cavity, and inflate it slowly with sterile water or air (per the manufacturer's recommendations) until the bleeding stops. o Posterior epistaxis balloons: Posterior epistaxis balloons generally have separate anterior and posterior balloons. After passing the posterior balloon through the naris and into the posterior nasal cavity, inflate it with 4-5 mL of sterile water and gently pull it forward to fit snugly in the posterior choana. After bleeding into the posterior pharynx has been controlled, fill the anterior balloon with sterile water until the bleeding completely stops. Avoid overinflation because pressure necrosis or damage to the septum may result. Record the amount of fluid placed in each balloon. If a Foley catheter is used, place a 12-16F catheter with a 30-cc balloon into the nose along the floor of the nasopharynx, until the tip is visible in the posterior pharynx. Slowly inflate the balloon with 15 mL of sterile water, pull it anteriorly until it firmly sets against the posterior choanae, and secure it in place with an umbilical clamp. Use a buttress clamp with cotton gauze to avoid pressure necrosis on the nasal alae or columella. Finally, an anterior nasal pack should be placed. Consultations: Epistaxis that requires posterior packing should be managed in cooperation with an ear, nose, and throat (ENT) specialist. Because of multiple possible complications, admission is required, usually in a monitored setting. MEDICATION Section 7 of 10 Author Information Introduction Clinical Differentials Workup Treatment Medication Follow-up Miscellaneous Bibliography Patients discharged from the hospital with anterior packing should receive follow-up care with an ENT specialist within 48-72 h. Nasal packing prevents drainage of sinuses. Consider placing patients on a broad-spectrum antibiotic to cover all likely pathogens in the context of the clinical setting. Oral analgesics should be prescribed to assure quality patient care. Drug Category: Antibiotics -- Therapy must cover all likely pathogens in the context of the clinical setting. Consider giving patients a penicillin or first-generation cephalosporin. Drug Name Amoxicillin (Biomox, Trimox) -- Treats infections caused by susceptible organisms and used as prophylaxis in minor procedures. Adult Dose 250-500 mg PO q8h; not to exceed 3 g/d Pediatric Dose Contraindications 20-50 mg/kg/d PO q8h Documented hypersensitivity Interactions Reduces the efficacy of oral contraceptives Pregnancy B - Usually safe but benefits must outweigh the risks. Precautions Adjust dose in renal impairment Drug Name Cephalexin (Keflex) -- First-generation cephalosporin, which is primarily active against skin flora. Used for skin structure coverage and as prophylaxis in minor procedures. Adult Dose 250-1000 mg PO q6h; not to exceed 4 g/d Pediatric Dose 25-50 mg/kg/d PO q6h; not to exceed 3 g/d Contraindications Documented hypersensitivity Interactions Coadministration with aminoglycosides increases nephrotoxic potential Pregnancy B - Usually safe but benefits must outweigh the risks. Precautions Adjust dose in renal impairment Drug Category: Analgesics -- Pain control is essential to quality patient care. It ensures patient comfort, promotes pulmonary toilet, and enables physical therapy regimens. Most analgesics have sedating properties, which are beneficial for patients who have painful skin lesions. Avoid NSAIDs and aspirin. Drug Name Acetaminophen (Tylenol, Aspirin Free Anacin, Feverall) -- DOC for treating pain in documented hypersensitivity to aspirin, upper GI disease, or concurrent administration of oral anticoagulants. Adult Dose 325-650 mg PO q4-6h or 1000 mg PO tid/qid; not to exceed 4 g/d Pediatric Dose <12 years: 10-15 mg/kg/dose PO q4-6h prn; not to exceed 2.6 g/d> >12 years: 650 mg PO q4h; not to exceed 5 doses in 24 h Contraindications Documented hypersensitivity Interactions Rifampin can reduce analgesic effects; coadministration with barbiturates, carbamazepine, hydantoins, and isoniazid may increase hepatotoxicity Pregnancy B - Usually safe but benefits must outweigh the risks. Precautions Hepatotoxicity possible in chronic alcoholism following various dose levels; severe or recurrent pain or high or continued fever may indicate a serious illness; contained in many OTC products, and combined use with these products may result in cumulative doses exceeding recommended maximum dose Drug Name Hydrocodone bitartrate and acetaminophen (Vicodin ES) -- For the relief of moderate to severe pain. Adult Dose 1-2 tab or cap PO q4-6h prn for pain <12 years: Based on acetaminophen dose of 10-15 g/kg/dose PO q4-6h prn; not to exceed 10 mg/dose of hydrocodone bitartrate or 2.6 g/d of acetaminophen> Pediatric Dose >12 years: Based on acetaminophen dose of 750 mg PO q4h; not to exceed 5 doses q24h Contraindications Documented hypersensitivity Interactions Phenothiazines may decrease the analgesic effects; toxicity increases with coadministration of CNS depressants or tricyclic antidepressants Pregnancy C - Safety for use during pregnancy has not been established. Precautions Tabs contain metabisulfite, which may cause allergic reactions FOLLOW-UP Section 8 of 10 Author Information Introduction Clinical Differentials Workup Treatment Medication Follow-up Miscellaneous Bibliography Further Inpatient Care: Admit patients with posterior packing. Elderly patients or patients with cardiac disorders or chronic obstructive pulmonary disease (COPD) should receive supplemental oxygen and be admitted to a monitored setting. Significant or uncontrolled bleeding from a posterior site may require operative management. At most centers, selective arterial embolization has become the treatment of choice for severe epistaxis. Further Outpatient Care: Patients discharged with anterior packing should receive follow-up care with an ENT specialist within 48-72 hours. Nasal packing increases the risk of sinusitis or toxic shock syndrome. Patients discharged with nasal packing should be prescribed a penicillin or first-generation cephalosporin. Oral analgesics should also be prescribed. Advise patients to avoid aspirin, aspirin-containing products, and NSAIDs. Patients who take warfarin may generally continue their current regimen unchanged. Temporary discontinuation of warfarin or active reversal of coagulopathy is indicated only in cases of uncontrolled hemorrhage and supratherapeutic INR. Give patients specific written follow-up instructions. Complications: Sinusitis Septal hematoma/perforation External nasal deformity Mucosal pressure necrosis Vasovagal episode Balloon migration Aspiration Prognosis: With proper treatment, prognosis is excellent. Patient Education: For rebleeding or future nosebleeds, patients should be instructed to firmly pinch their entire nose for 10-15 minutes. Ice packs do not help. For excellent patient education resources, visit eMedicine's Ears, Nose, and Throat Center. Also, see eMedicine's patient education article Nosebleeds. MISCELLANEOUS Section 9 of 10 Author Information Introduction Clinical Differentials Workup Treatment Medication Follow-up Miscellaneous Bibliography Medical/Legal Pitfalls: Posterior nasal packing is particularly uncomfortable for the patient and promotes hypoxia and hypoventilation. Failure to admit and appropriately monitor all patients who require posterior packing may result in significant mortality. Attempts at nasal packing may result in significant slowing but not cessation of hemorrhage. Failure to completely control hemorrhage is an absolute indication for consultation with an ENT specialist in the ED. Nasal packing can lead to serious infection. Patients discharged with anterior nasal packs should be started on oral antibiotics. Tumors or other serious pathology are infrequent causes of epistaxis. However, all patients who present with epistaxis should have follow-up care arranged with an ENT specialist for a complete nasopharyngeal examination. BIBLIOGRAPHY Section 10 of 10 Author Information Introduction Clinical Differentials Workup Treatment Medication Follow-up Miscellaneous Bibliography Ahmed A, Woolford TJ: Endoscopic bipolar diathermy in the management of epistaxis: an effective and cost-efficient treatment. Clin Otolaryngol 2003 Jun; 28(3): 273-5[Medline]. Cassisi NJ, Biller HF, Ogura JH: Changes in arterial oxygen tension and pulmonary mechanics with the use of posterior packing in epistaxis: a preliminary report. Laryngoscope 1971 Aug; 81(8): 1261-6[Medline]. Choudhury N, Sharp HR, Mir N, Salama NY: Epistaxis and oral anticoagulant therapy. Rhinology 2004 Jun; 42(2): 92-7[Medline]. Cook PR, Renner G, Williams F: A comparison of nasal balloons and posterior gauze packs for posterior epistaxis. Ear Nose Throat J 1985 Sep; 64(9): 446-9[Medline]. Elwany S, Kamel T, Mekhamer A: Pneumatic nasal catheters: advantages and drawbacks. J Laryngol Otol 1986 Jun; 100(6): 6417[Medline]. Fairbanks DN: Complications of nasal packing. Otolaryngol Head Neck Surg 1986 Mar; 94(3): 412-5[Medline]. Fuchs FD, Moreira LB, Pires CP, et al: Absence of association between hypertension and epistaxis: a population-based study. Blood Press 2003; 12(3): 145-8[Medline]. Guarisco JL, Graham HD 3d: Epistaxis in children: causes, diagnosis, and treatment. Ear Nose Throat J 1989 Jul; 68(7): 522, 528-30, 532 passim[Medline]. Herkner H, Havel C, Mullner M: Active epistaxis at ED presentation is associated with arterial hypertension. Am J Emerg Med 2002 Mar; 20(2): 92-5[Medline]. Karras DJ, Ufberg JW, Harrigan RA, et al: Lack of relationship between hypertension-associated symptoms and blood pressure in hypertensive ED patients. Am J Emerg Med 2005 Mar; 23(2): 106-10[Medline]. Keen MS, Moran WJ: Control of epistaxis in the multiple trauma patient. Laryngoscope 1985 Jul; 95(7 Pt 1): 874-5[Medline]. Larsen K, Juul A: Arterial blood gases and pneumatic nasal packing in epistaxis. Laryngoscope 1982 May; 92(5): 586-8[Medline]. Okafor BC: Epistaxis: a clinical study of 540 cases. Ear Nose Throat J 1984 Mar; 63(3): 153-9[Medline]. Pope LE, Hobbs CG: Epistaxis: an update on current management. Postgrad Med J 2005 May; 81(955): 309-14[Medline]. Singer AJ, Blanda M, Cronin K, et al: Comparison of nasal tampons for the treatment of epistaxis in the emergency department: a randomized controlled trial. Ann Emerg Med 2005 Feb; 45(2): 134-9[Medline]. Siniluoto TM, Leinonen AS, Karttunen AI, et al: Embolization for the treatment of posterior epistaxis. An analysis of 31 cases. Arch Otolaryngol Head Neck Surg 1993 Aug; 119(8): 837-41[Medline]. Teymoortash A, Sesterhenn A, Kress R, et al: Efficacy of ice packs in the management of epistaxis. Clin Otolaryngol Allied Sci 2003 Dec; 28(6): 545-7[Medline]. Viducich RA, Blanda MP, Gerson LW: Posterior epistaxis: clinical features and acute complications. Ann Emerg Med 1995 May; 25(5): 592-6[Medline]. Wurman LH, Sack JG, Flannery JV Jr, Lipsman RA: The management of epistaxis. Am J Otolaryngol 1992 Jul-Aug; 13(4): Middle Ear, Tympanic Membrane, Perforations Matthew L Howard, MD, JD, Head and Neck Surgery (Retired), Kaiser Permanente Medical Center, Santa Rosa, California Contributor Information and Disclosures Updated: Oct 6, 2008 Print This Email This Overview Workup Treatment Follow-up References Keywords Introduction Tympanic membrane perforation (TMP) is a condition as old as the human species. Problem The tympanic membrane, also called the eardrum (or just the drum), is a stiff (but flexible), translucent, diaphragmlike structure. The eardrum moves synchronously in response to variations in air pressures, which constitute sound waves. The drum's vibrations are transmitted through the ossicular chain to the cochlea. In the cochlea, vibratory mechanical energy changes to electrochemical energy and streams via the eighth cranial nerve to the brain. The tympanic membrane and its attached ossicles thus act as a transducer, changing one form of energy into another form. Tympanic membrane perforations (TMPs) can result from disease (particularly infection), trauma, or medical care. Perforations can be temporary or persistent. Effect varies with size, location on the drum surface, and associated pathologic condition. Frequency Incidence of tympanic membrane perforation (TMP) in the general population is unknown. One survey found that that 4% of a population of Native American children had tympanic membrane perforation (TMP).1 Another study found that 3% of children treated with ventilation tubes had the condition.2 However, the incidence in the general population has not been studied. Even the exact number of surgical tympanic membrane perforation (TMP) repairs performed each year is unknown. Analysis of government statistics indicates that perhaps 150,000 tympanoplasties are performed per year in a population of 280 million. Etiology Infection is the principal cause of tympanic membrane perforation (TMP). Acute infection of the middle ear may cause a relative ischemia in the drum concurrent with increased pressure in the middle ear space. This leads to a tear or rupture of the eardrum that is usually preceded by severe pain. If the perforation does not heal, it leaves a residual tympanic membrane perforation (TMP). A prominent school of thought now advocates less aggressive use of antibiotics. Those who hold this position recognize that many episodes of otitis media are caused by viruses, so they resolve spontaneously; advocates of this position desire to slow emergence of antibiotic-resistant bacterial strains. Evidence is emerging that an increased incidence of acute mastoiditis is resulting from reduced use of antibiotics.3 Time will tell whether increased incidence of perforation and other complications of otitis media, such as brain abscess, meningitis, and septic sigmoid sinus thrombosis, also occur. Ear canal infections rarely cause tympanic membrane perforations (TMP). When this occurs, it is often associated with infection by Aspergillus niger. Traumatic perforations may result from blows to the ear (eg, being struck with the flat of the hand; falling from water skis with the head hitting the water surface, ear down). Exposure to severe atmospheric overpressure from an explosion can tear the drum.4 Tympanic membrane perforation (TMP) from water pressure occurs in scuba divers, usually in a drum with atrophy from previous disease. Objects used to clean the ear canal can perforate the drum. Inexpertly performed irrigation of the ear canal for wax can lead to perforation. In some settings, when irrigation for cerumen is relegated to medical assistants, otolaryngologists may see 10-20 patients per year with this injury. Tympanic membrane perforation (TMP) is intentionally created whenever a surgeon makes an incision in the eardrum (myringotomy). When pressure-equalizing tubes (ventilating tubes) are placed, the TMP purposely is held open. Failure of surgically created openings to heal when the tube extrudes results in chronic tympanic membrane perforation (TMP). Pathophysiology The eardrum tends to heal itself. Even eardrums that have been perforated multiple times often remain intact. At times, a perforation heals with a thin membrane consisting only of mucosal and squamous epithelial layers without a fibrous middle layer. Such a neomembrane may be so thin that it can be mistaken for a perforation instead of a healed perforation. Neomembranes may retract deeply into the middle ear, sometimes making them more difficult to distinguish from actual perforations. Examination under the operating microscope resolves ambiguity. Deep retraction, especially in the posterior superior quadrant of the drum, may presage formation of cholesteatoma. The presence of perforation renders the ear more susceptible to infection if water enters the ear canal. If bacteria-contaminated water passes through the perforation, infection can result. Water surface tension may protect the ear from penetration through a very small perforation. This explains higher infection rates from hair washing than from swimming activities (ie, soap lowers surface tension so water can enter the middle ear). Presence of perforation is an absolute contraindication to irrigation for cerumen removal. History of perforation is also an absolute contraindication unless personal knowledge derived from prior examination indicates an intact drum. Presentation Perforation symptoms may include audible whistling sounds during sneezing and nose blowing, decreased hearing, and a tendency to infection during colds and when water enters the ear canal. Copious purulent drainage, which may be sanguineous in both acute and chronic perforation, confirms both perforation and infection. Ear canal infections also can cause purulent drainage, but usually in lesser amounts. Perforations uncomplicated by infection or cholesteatoma are never painful. Presence of pain should alert the physician to a concurrent disease process. Perforations accompanied by otorrhea or cholesteatoma are usually not painful. Indications Many persons live their lives with tympanic membrane perforations that are entirely without symptoms. Repair of such lesions is usually not indicated. Perforations may be associated with recurrent infection when exposed to water. In swimmers, divers, and other water sports enthusiasts, repair may be indicated as a quality-of-life issue. Hearing loss may be present, especially with larger perforations, and may be a reason for repair. Because a risk to residual hearing exists with every operation on the ear drum, a riskbenefit analysis in which the patient participates is mandatory. For example, question whether the person may be helped just as much with use of a hearing aid. Relevant Anatomy The tympanic membrane has 2 distinct zones. The larger of the 2 zones is the pars tensa. This zone consists of a tough and resilient fibrous layer with a diaphanous mucosal layer inside and squamous epithelium outside. The smaller zone is the pars flaccida, which lies superior to the suspensory ligaments of the malleus and lacks a fibrous layer. Perforations of this area often are described as more frequently associated with complications. This is true if the definition of TMP includes depressions of the drum into the middle ear, forming saclike structures (retraction pockets). Clearly, such pockets are more often associated with cholesteatoma formation. Behind (or medial to) the drum is the middle ear. In front of the drum (or lateral or exterior) is the ear canal. The drum lies at an angle to the bore of the ear canal, creating a vestibule, which can retain cerumen or debris. The malleus is invested by the fibrous layer of the tympanic membrane, securely incorporating it within the drum. Contraindications Tympanic membrane perforation (TMP) may be unilateral or bilateral. Select the worsehearing ear first when performing bilateral tympanic membrane perforation (TMP) repair. If increased hearing loss complications ensue, the better-hearing ear remains uninjured. For the same reason, if tympanic membrane perforation (TMP) is present in a patient's single hearing-capable ear, only incipient life-threatening complications justify repair attempts. Workup Imaging Studies Radiography and MRI are of no value unless the clinical picture suggests ossicular destruction and/or cholesteatoma. Asymptomatic perforations, especially if hearing is near normal, require no imaging studies. Other Tests Most tympanic membrane perforations (TMPs) are diagnosed using routine otoscopy. Small perforations may require otomicroscopy for identification. Some hearing screening programs include middle ear impedance testing. Screening tympanometry may reveal abnormalities consistent with perforation. Confirmation still requires examination. Always perform audiometry upon initial TMP diagnosis and again before any repair attempt, whether in the office or in the operating room. o Preoperative and postoperative audiography should always be performed. A major conductive loss not only alerts the surgeon to the possible existence of ossicular lesions, but documentation of a preexisting sensorineural hearing loss may protect the surgeon from later allegations that the surgery caused the hearing loss. o Audiometry often reveals normal hearing. The presence of mild conductive hearing loss is consistent with perforation, and a conductive component of at least 30 dB indicates possible ossicular discontinuity or a pathologic condition. Diagnostic Procedures In rare cases, otomicroscopy and impedance studies still leave the tympanic membrane perforation (TMP) diagnosis questionable. To provide evidence of perforation (in the form of a stream of bubbles), fill the ear canal with sufficient distilled water or sterile saline to cover the tympanic membrane and have the patient perform the Valsalva maneuver. A negative test result is suggestive but not definitive. A positive test result is caused only by tympanic membrane perforation (TMP). Histologic Findings In chronic tympanic membrane perforation (TMP), squamous epithelium is found adjacent to middle ear mucosa and creates a perforation edge with no raw surface. Such healing of the perforation edge is undoubtedly a contributing factor to perforation persistence. Treatment Medical Therapy Medical therapy for perforations is directed at controlling otorrhea. Take into account ototoxicity risk from topically applied eardrops when treating ear infections concurrent with tympanic membrane perforation (TMP). Infection alone occasionally can cause sensorineural hearing loss. Clinical toxicity from eardrops in the presence of ear infection has not been demonstrated unequivocally, although experiments in animals clearly demonstrate a correlation. Legal implications of administration of ototoxic eardrops preceding sensorineural hearing loss are clear. For this reason, avoid eardrops containing gentamicin, neomycin sulfate, or tobramycin in the presence of tympanic membrane perforation (TMP). When they are used, substitute a less toxic alternative as soon as drainage and mucosal edema begin to subside. Avoiding contamination of the middle ear space with water via the tympanic membrane perforation (TMP) is critical in minimizing otorrhea from a perforation. Systemic antibiotics are occasionally used when controlling otorrhea from a TMP. Antibiotics (eg, trimethoprim-sulfamethoxazole, amoxicillin) directed at typical respiratory flora suffice in most cases. Overgrowth with Pseudomonas aeruginosa or resistant Staphylococcus aureus may occur. Failure of drainage to clear after several days' therapy may require alteration of therapy following culture and sensitivity tests. A tendency of the ear canal to pseudomonad overgrowth indicates that the most accurate testing can be obtained by suctioning a culture specimen (under microscopic control) directly from the middle ear through the perforation. Under routine circumstances, the surface tension of water may prevent it from entering the middle ear through a small perforation. The addition of soap reduces the water tension. The ear is therefore at greater risk of infection during hair-washing or bathing than from plain water. Surgical Therapy Treatment of tympanic membrane perforation (TMP) falls into 3 categories. No treatment is necessary for nonswimming patients with minimal hearing loss and no history of recurrent ear infection. A hearing aid may prove the only necessary treatment for patients with symptomatic hearing loss but no infection or swimming history. Two options exist for patients who are not in either category. Office treatments The first option is to perform one of the available office treatments. Such treatments have the best chance of working when the perforation is small and involves neither the umbo nor the annulus. Several methods apply. The simplest, but least effective, method is to cauterize the edges of the tympanic membrane perforation (TMP) with a caustic, such as trichloroacetic acid (10% solution), and then apply a small patch of cigarette paper. This technique was developed in the 1800s; it presumably remains in the repertoire because it sometimes works. Mechanical stripping of the perforation margin (with topical anesthetic or without) before applying the patch slightly increases the success rate. A fat-plug tympanoplasty can be performed. Obtain a small plug of fat from the postauricular sulcus with the patient under local anesthesia. Prepare the tympanic membrane perforation (TMP) by anesthetizing its margins with carefully applied phenol solution. Next, mechanically débride the edges with microcup forceps. The fat is then tucked into the perforation, extending both into the canal and into the middle ear space. The paper-patch method has a reported success rate of 67%; the fat-plug tympanoplasty of 87%.5 Another successful office treatment, which has the major disadvantage of requiring 6-10 weekly postsurgical office visits, is the irritant oil method. In this method, freshen the perforation by stripping the margin using microcup forceps. Performed carefully, this can often be accomplished without anesthetic. If necessary, use a small amount of phenol solution for anesthesia. Apply a cotton ball that is 1-2 mm larger than the diameter of the perforation to the tympanic membrane perforation (TMP). The patient then instills a solution of irritative and aromatic oils daily into the ear. The solution is dispensed in 30-mL dropper bottles and is formulated by the pharmacy (all substances United States Pharmacopoeia [USP] grade) as 2 mL eucalyptol, 1.10 mL methyl salicylate, 0.39 g thymol, 0.455 g menthol, 1.20 mL oil of orange, 20.25 g sifted powdered sodium borate, 20.25 g powdered boric acid, 60 mL of 90% ethyl alcohol, saffron to suit for color, and water in a sufficient quantity to make 5000 mL. Change the cotton weekly. Repeat edge freshening if no progress is seen. This nonsurgical method was initially reported to have a 70% success rate, and this author has obtained similar results using it as the sole therapy for perforations occupying less than 25% of the drum area.6, 7 Other recently reported forms of office treatment use fibrin glue or a patch composed of a hyaluronic acid ester and a dressing component. The use of basic fibroblast growth factor with a proprietary patch that consists of a silicone layer and atelocollagen has been described. Excellent success has been reported, but with very small numbers of patients. Time will tell if these new techniques will prove useful additions to treatment options. Tympanoplasty The second option is to perform tympanoplasty with the patient under local or general anesthesia. An incision may be made behind the ear or entirely through the ear canal, depending on the location and size of the tympanic membrane perforation (TMP). Repair requires preparation of a suitable bed for placement of a graft. By far, the most commonly used grafting material is postauricular fascia. Allograft tympanic membranes obtained from cadavers, once abandoned because of fear of transmitting viral pathogens, are again being used. Grafts may be placed either medially or laterally to the perforation. Surgeon preference plays a part in these decisions and in decisions concerning the technical problems associated with size and location of the perforation and the shape, angle, and bore of the ear canal. Tympanoplasty successfully closes the tympanic membrane perforation (TMP) in 9095% of patients. Fortunately, second and third operations succeed in more than 90% of the remaining patients. Consequently, fewer than 1 per 1000 persons still has tympanic membrane perforation (TMP) after 3 operations. Preoperative Details Preoperative preparation of the ear for surgery consists of eliminating infection whenever possible. Preoperative preparation of the patient includes convincing the smoker to stop during the immediate postoperative period. Intraoperative Details The first known incident of tympanoplasty performed on the wrong ear occurred in 2004. Surgeons are therefore advised to adopt methods similar to those used in other fields, and mark the ear to be operated upon with ink while the patient is awake and able to confirm the accuracy of the selection. Postoperative Details Postoperative care is identical for office treatment and operating room repair techniques. Instruct patients to keep water out of their ears. When incisions and ear canal packing are present, use protective dressings, which are commercially available. Otherwise, silicone rubber plugs (also commercially available) or cotton balls waterproofed with a little petroleum jelly suffice. Follow-up Risk of cholesteatoma formation, either through the natural course of the disease or from squamous epithelium trapped during treatment, requires regular follow-up care for all patients postoperatively. Several annual visits should be the minimum once tympanic membrane perforation (TMP) healing is verified. Untreated tympanic membrane perforation (TMP) may not require regular follow-up care if a patient can be relied upon to seek medical advice if hearing changes or persistent drainage from the ear is noted. Location of the tympanic membrane perforation (TMP) informs the timing and frequency of follow-up care. Perforations in the pars tensa (stiff portion of the drum) rarely lead to complications. The exceptions are pars tensa perforations located at the annulus or rim of the tympanic membrane. Tympanic membrane perforations (TMPs) in this location are at risk of developing middle ear cholesteatoma from migration of surface epithelium into the middle ear. Perforations in the pars flaccida (the portion without a fibrous center layer) are more frequently associated with complications and require more frequent follow-up care. For excellent patient education resources, visit eMedicine's Ear, Nose, and Throat Center. Also, see eMedicine's patient education article Perforated Eardrum. Complications Each operation carries a risk of exacerbating hearing loss. Exact incidence of such hearing loss is unclear, with reported rates varying widely in the medical literature. In one series, approximately 1 per 500 operations resulted in much worse hearing. In another, the rate was nearly 2% for some degree of loss. Of 1000 patients, expect one to experience a perforation and 4 to endure lost hearing. In a small group of patients, persistent eustachian tube dysfunction leads to late complications, such as cholesteatoma, reperforation, or middle ear effusion. When the underlay technique of tympanoplasty is used, incidence of intratympanic cholesteatoma is less than 1%.5 These complications each require unique treatment.