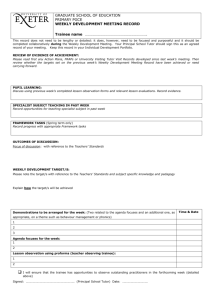
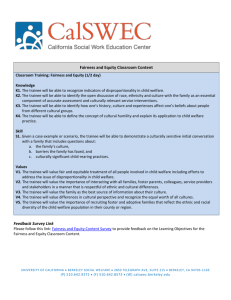
Trainee ARCP Record Book
advertisement

ACCS-Wales Workbook & ARCP Record Book For CT1 and 2 ACCS Trainees in the Welsh School ACCS – Wales Version 2.7 June 2014 1 Contents Introduction 3 Who’s Who & Contact Information 4 Trainee Representatives 5 Social Media 5 ACCS Curriculum 5 Educational Supervisors 6 Looking After Yourself (Your Health) 7 Protecting Your Patients (The Francis Report) 7 ARCP Checklist 8 Personal Details 13 Common Competences 14 Major Presentations 16 Acute Presentations 17 Advice for ACCS-EM Trainees 19 Anaesthesia for ACCS 20 Practical Procedures 22 Acute Medicine Paperwork 25 Emergency Medicine Paperwork 45 Anaesthesia Paperwork 72 Intensive Care Medicine Paperwork 92 A Career in Intensive Care Medicine? 112 2 Introduction Since the introduction of the new ACCS curriculum in May 2010 ACCS training is described under the headings of: 1. Common Competencies 2. Major Presentations 3. Acute Presentations 4. Anaesthesia in ACCS 5. Practical Procedures Some of this training must be obtained in a particular module, but other competencies can be achieved in any of the modules, provided that all are achieved by the end of year 2. This system can make it difficult for trainees and trainers to keep track of what competencies remain outstanding, and the ACCS workbook is designed to make this process easier. The workbook gives trainees and trainers a central document where all the required competencies and clinical procedures can be recorded, and correct paperwork identified. Trainees should use the e-portfolio for their parent specialty; non-parent modules may be completed on e-portfolio or paper, but ACCS-EM and ACCS-Medicine trainees are encouraged to use the e-portfolio for all modules. The Anaesthesia e-portfolio only contains anaesthesia-specific forms, so anaesthetists must use paper forms for other modules. Each time the trainee completes a module within the ACCS programme a Structured Training Report (StR) should be completed by the Module Supervisor. All “paperwork” whether on e-portfolio or paper, should be summarised on the paper checklists in this workbook. Supervisors’ signatures in the workbook are not necessary – “see e-portfolio” etc is acceptable. WPBAs including MSFs differ slightly between specialties, and should be completed using the paperwork specific to the specialty being assessed, NOT the parent specialty. Specialty-specific MSF and other WPBA forms, as well as all the specialty-specific paperwork, can be found in this workbook. At the ARCP the trainee should submit this workbook summarising the acquired competencies, along with the paper or e-portfolio evidence. A detailed ARCP Checklist can be found on pages 8-12. 3 Rachel Walpole: Training Programme Director, ACCS Wales Who’s Who and Contact Information Training Programme Director / Lead for ACCS Wales: Rachel Walpole, Consultant Anaesthetist, Newport Email: Rachel.Walpole@wales.nhs.uk Specialty Leads ACCS Lead for Anaesthesia: Rachel Walpole, Consultant Anaesthetist, Newport Email: Rachel.Walpole@wales.nhs.uk ACCS Lead for Acute Medicine: Llifon Edwards, Consultant Physician, Newport Email: Llifon.Edwards@wales.nhs.uk ACCS Lead for Intensive Care Medicine: Alison Ingham, Consultant Anaesthetist & Intensivist, Bangor Email: Alison.Ingham@wales.nhs.uk ACCS Lead for Emergency Medicine: Robin Roop, Consultant Emergency Medicine, Wrexham Email: Robin.Roop@wales.nhs.uk Hospital Leads University Hospital of Wales, Cardiff: Melvyn Jenkins-Welch, Consultant Anaesthetist Email: Melvyn.Jenkins-Welch@wales.nhs.uk Morriston Hospital, Swansea: Dinendra Gill, Consultant Emergency Physician Email: Dinendra.Gill@wales.nhs.uk Royal Gwent Hospital, Newport: Rachel Walpole, Consultant Anaesthetist Email: Rachel.Walpole@wales.nhs.uk Ysbyty Gwynedd, Bangor: Alison Ingham, Consultant Anaesthetist & Intensivist, Bangor Email: Alison.Ingham@wales.nhs.uk Wrexham Maelor Hospital: Ben Thomas, Consultant Physician 4 Email: Ben.Thomas@wales.nhs.uk Specialty Training Manager, Deanery Ms Lisa Bassett Email: BassettL@cardiff.ac.uk Trainee Representatives There are 2 elected trainee representatives, one from CT1 and one from CT2. They represent trainees’ views at Specialist Training Committee meetings. Please contact one of them if there are issues you wish to bring to the attention of the STC. CT2: Jonathan Lloyd-Evans (Cardiff) Email: jlloydevans@gmail.com CT1: will be elected in September 2014 Educational Supervision Each department has an identified Educational Supervisor who takes responsibility for ACCS trainees (see page 6). You should contact this person before you begin the placement or as soon as possible afterwards, and arrange for an initial meeting within 2 weeks of starting in post. If you are unsure who is supervising you please email Lisa Bassett, address above. Social Media There is an ACCS Wales Facebook Group and Twitter account. On Facebook, please search for ACCS Wales and join the group, it is open to everyone. You are welcome to use it to share information or to put questions to other members of the group. For Twitter: follow @ACCSWales to receive information, reminders and updates. ACCS Curriculum The ACCS Curriculum can be found on the ACCS pages of the Welsh Deanery Website: http://www.walesdeanery.org/index.php/en/trainees-in-training.html 5 Educational Supervisors Wrexham Lead: Ben Thomas Anaesthesia: Venkataravan Madhavan ITU: Mahmoud Wagih AM: Ben Thomas EM: Robin Roop Swansea Lead: Dinendra Gill Anaesthesia: Tracey Wall ITU: Vijay Kumar AM: Praveen Eadala EM: Dinendra Gill Cardiff Lead: Melvyn Jenkins-Welch Anaesthesia: Melvyn Jenkins-Welch ITU: Sabine Grundler AM: Simon Barry & Andrew Freedman EM: Susan Allen Newport Lead: Rachel Walpole (Anaesthesia) Anaesthesia: Helen Jewitt ITU: Babu Muthuswamy Acute Med: Llifon Edwards ; Cardiology: Philip Campbell; Respiratory Med: Sara Fairbairn EM: Tim Rogerson Nevill Hall Lead: Ed Curtis Anaesthesia & ITU: Ed Curtis EM: Ella Harrison-Hansley Bangor Lead: Alison Ingham Anaesthesia & ITU: Alison Ingham AM: Mahdi Jibani EM: Leesa Parkinson 6 Looking after Yourself Medicine is a stressful profession, and Core Training can be particularly difficult because of frequent changes of post, a steep learning curve, and exam pressures. The GMC makes clear that a good doctor looks after their own health and well-being as well as that of their patients. If you find yourself struggling then either your Educational Supervisor or any Consultant that you feel able to talk to should be your first source of support. However if you feel unable to confide in a senior colleague, you may wish to make use of the BMA helpline; it is not necessary to be a BMA member to use it: BMA Counselling & Doctor Adviser Service: 0845 9200169 Alternatively, Health for Health Professionals Wales offers free Psychotherapy referral to any doctor in Wales. It is a confidential service funded by the Welsh Government. http://www.hhpwales.co.uk Tel 0800 0582738 between 9am and 5pm Mon-Fri, calls free from a landline. Protecting your Patients & The Francis Report The Francis Report stressed that junior doctors have a duty to “blow the whistle” if they feel that they have witnessed poor standards of patient care. Concerns about standards should ideally be discussed with your Educational Supervisor, the College Tutor or Clinical Director. If you do not feel able to speak to any of these people, you can contact a member of the ACCS STC who works outside of your own hospital (contact details on p.4). Alternatively, the Intranet should have details of your Health Board’s Whistleblowing Policy. (It may be “Whistleblowing”, or “Raising Concerns” etc). 7 ACCS ARCP Checklist Trainees should attend with their portfolio, ACCS Workbook and the following: Enhanced Form R: should be completed and returned at least 2 weeks in advance of the ARCP. Absence Monitoring Declaration: this is a self-declaration of any unplanned absences since your last ARCP. You should record any absences other than Annual Leave and Study Leave. Examples of unplanned absences are Sick Leave, Maternity or Paternity Leave, Compassionate Leave, etc. Study Leave Record: This can be printed out from Intrepid. GMC Survey: Evidence of completion. The portfolio requirements for ACCS ARCPs are in 2 parts: 1. Competencies that can be achieved at any point during CT1 and 2 but must be achieved by the end of CT2. 2. Competencies and evidence of satisfactory performance in each of the modules (usually 2) undertaken since the last ARCP. CT2 trainees should present all paperwork relating to the entire 2 years of ACCS training, even if it has previously been presented at the CT1 ARCP. Please note that an ARCP Structured Report must be presented for each module of training, even if the module is incomplete (usually a June / July ARCP for a module that ends in July). 8 ACCS ARCP Checklist Major & Acute Presentations, Practical Procedures The following competencies must be achieved by the end of CT2. Trainees for CT1 ARCP should have evidence that progress is being made towards achieving these competencies. Common Competencies At least 50% achieved to level 2 descriptors Ref: Workbook p13 Definitions of descriptors can be found at: http://www.accs.severndeanery.nhs.uk/assets/Accs/Curriculum/CommonCompetenciesfor ACCSleveldescriptorscurriculumpage.docx All 6 Major Presentations Ref: Workbook p15; at least 2 during EM and 2 during AM. 28 Acute Presentations: At least 20 of the 38 by WPBA: 10 during EM, 10 during AM. 8 further Acute Presentations covered by WPBAs including ACAT, or by e-learning, reflective entries, teaching and audit. Ref: Workbook p16 39 Practical Procedures: At least 39 of the 44. Ref: Workbook p20 ALS-Provider Mandatory for all ACCS trainees by the end of CT2. This is in addition to a WPBA for Cardiorespiratory Arrest (see Major Presentations). EM Trainees must be APLS and ATLS-Providers (or equivalent) by the end of CT3. 9 ACCS ARCP Checklist Individual Module Requirements Anaesthesia o ARCP Structured Report o Initial Assessment of Competency Certificate (IACC) o All required WPBAs are incorporated into the IACC o A Multi-Source Feedback: 360o Team Assessment of Behaviour (MSF) o Copy of Logbook o Educational Agreement Intensive Care Medicine o Educational Supervisor’s Report o Logbook o 6 x Directly Observed Procedural Skills (DOPS) o 4 x Case Based Discussions (CBD) o 3 x Clinical Evaluation Exercises (CEX) o Multi-Source Feedback: 360o Team Assessment of Behaviour (MSF) WPBAs Should Include: o 2 of the 6 Major Presentations: CBD or CEX (formative) o Sepsis is suggested 10 ACCS ARCP Checklist Acute Medicine o Educational Supervisor’s Report o Multi-Source Feedback: 360o Team Assessment of Behaviour (MSF) o Educational Agreement WPBAs: o 3 x Acute Care Assessment Tools (ACAT) o 3 x Case Based Discussions (CBD) o 3 x Clinical Evaluation Exercises (CEX) o 5 x Directly Observed Procedural Skills (DOPS) o A different 5 from those assessed in EM WPBAs Should Include: o 2 of the 6 Major Presentations: CBD or CEX (formative) o 10 of the 38 Acute Presentations: CBD, CEX or ACAT (formative) Please note that Multiple Consultant Reports (MCRs) are not required for ACCS, though ACCS-Medicine trainees may choose to do them. 11 ACCS ARCP Checklist Emergency Medicine o Structured Training Report o Multi-Source Feedback: 360o Team Assessment of Behaviour (MSF) o Training Agreement o Logbook WPBAs: o o o o 1 x Acute Care Assessment Tools (ACAT) 3 x Case Based Discussions (CBD) 4 x Clinical Evaluation Exercises (CEX) 5 Directly Observed Procedural Skills (DOPS) using specific forms; these 5 are suggested: Airway maintenance Primary Survey in Trauma Wound Management Fracture or Joint Manipulation 1 other of the 44 listed practical procedures not covered elsewhere (list below) WPBAs Should Include: o 2 of the 6 Major Presentations: summative* CBD or CEX; must be Consultant assessment. o 5 of the 38 Acute Presentations, summative* CBD or CEX; must be Consultant assessment, these 5 are suggested: Abdominal Pain Breathlessness Chest Pain Head Injury Mental Health o 5 further Acute Presentations, ACAT (formative*) *A summative assessment has a pass/fail outcome and must be assessed by a Consultant. A formative assessment is not a pass or fail assessment and can be performed by any appropriate person. 12 Personal Details Trainee’s Name GMC Number ACCS Parent Specialty College Training Number Base Hospital(s) Parent Specialty Supervisor* Module 1 Specialty / Dates Module 1 Clinical Supervisor** Module 2 Specialty / Dates Module 2 Clinical Supervisor** Year 1 ARCP Date Outcome Date Outcome Module 3 Specialty / Dates Module 3 Supervisor** Module 4 Specialty / Dates Module 4 Supervisor** Year 2 ARCP *Parent Specialty Supervisor is a Consultant in the base hospital from the trainee’s parent specialty. This person provides continuity of support over the 3-year programme, and is a source of careers advice, exam support etc. **Module supervisor (Also known as Clinical Supervisor) is the person responsible for the trainee during that module and will be the person completing the Structured Training Report at the end of that specific module with the trainee. 13 COMMON COMPETENCES Many of these competences are an integral part of clinical practice and as such will be assessed concurrently with the clinical presentations and procedures assessments. Trainees should use these assessments to provide evidence that they have achieved the appropriate level. Descriptors of required performance at each level can be found at: http://www.accs.severndeanery.nhs.uk/assets/Accs/Curriculum/CommonCompetenciesforACCSl eveldescriptorscurriculumpage.docx For a small number of common competences alternative evidence should be used, e.g. assessments of audit and teaching, completion of courses, management portfolio. At least 50% of Common Competences should be signed off by the end of the CT2 ACCS year. Competency 1 Level achieved (Sign and date) 2 3 1) History taking 2) Clinical examination 3) Therapeutics and safe prescribing 4) Time management and decision making 5) Decision making and clinical reasoning 6) The patient as central focus of care 7) Prioritisation of patient safety in clinical practice 8) Team working and patient safety 9) Principles of quality and safety improvement 10) Infection control 14 4 Competency 1 Level achieved (Sign and date) 2 3 11) Managing long term conditions and promoting patient self-care 12) Relationships with patients and communication within a consultation 13) Breaking bad news 14) Complaints and medical error 15) Communication with colleagues and cooperation 16) Health promotion and public health 17) Principles of medical ethics and confidentiality 18) Valid consent 19) Legal framework for practice 20) Ethical research 21) Evidence and guidelines 22) Audit 23) Teaching and training 24) Personal behaviour 25) Management and NHS structure 15 4 MAJOR PRESENTATIONS These are seen as the cornerstone of the clinical skills of ACCS trainees and they should all be signed off by the end of the second year. 2 must be completed during the Emergency Medicine module and must be assessed by a Summative Assessment by a Consultant using either a CbD or mini-CEX specifically designed for Summative Assessment (Curriculum pages 221 & 225). 2 will be assessed in the Acute Medicine module and the other 2 can be done in any of the modules, but it is recommended that the Septic Patient should be signed off in the Intensive Care Medicine module. Anapylaxis and Cardiorespiratory Arrest may be simulated – BUT an ALS Course is not a substitute for either of these. The knowledge, skills and behaviours to be achieved for each presentation are listed in the curriculum pp 75– 84. Presentation ACCS Module AM/EM/ICM/An Date Modular (Clinical) supervisor 1) Anaphylaxis 2) Cardiorespiratory Arrest 3) Major Trauma 4) Septic Patient 5) Shocked Patient 6) Unconscious Patient 16 ACUTE PRESENTATIONS There are 38 Acute Presentations (APs). 10 should be signed off during the AM module, and 10 during the EM module. At least 8 further APs should be covered by ACAT, e-learning, reflective entries, teaching and audit. There are 5 APs that require the trainee to complete specific summative WPBA during the EM module (see table). Up to 5 APs can be covered by a single ACAT in either EM or AM. The knowledge, skills and behaviours required for each presentation are listed in the curriculum pp86-140. Presentation 1) Abdominal Pain including loin pain ACCS Module AM/EM/ICM/ An Date Modular (Clinical) supervisor EM 2) Abdominal Swelling, Mass & Constipation 3) Acute Back Pain 4) Aggressive/disturbed behaviour 5) Blackout/Collapse 6) Breathlessness 7) Chest Pain EM EM 8) Confusion: Acute/Delirium 9) Cough 10) Cyanosis 11) Diarrhoea 12) Dizziness and Vertigo 13) Falls 14) Fever 15) Fits / Seizure 16) Haematemesis & Melaena 17) Headache 18) Head Injury EM 17 19) Jaundice 20) Limb Pain & Swelling – Atraumatic 21) Neck pain 22) Oliguric patient 23) Pain Management 24) Painful ear 25) Palpitations 26) Pelvic pain 27) Poisoning 28) Rash 29) Red eye 30) Suicidal ideation / Mental health EM 31) Sore throat 32) Syncope and pre-syncope 33) Traumatic limb and joint injuries 34) Vaginal bleeding 35) Ventilatory Support 36) Vomiting & Nausea 37) Weakness & Paralysis 38) Wound assessment and management 18 Advice for ACCS-EM Trainees: Prepare now for your CT3 ARCP! The ACCS Curriculum covers CT1-2 but it is worth anticipating the requirements for CT3 as it is much easier to get the competencies signed off as you see them rather than trying to “chase” then later. By the end of CT3 you will need the following: All 6 Major Presentations by Summative WPBA assessed by a Consultant: Anaphylaxis and Cardiorespiratory Arrest may be assessed by simulation ALS-Provider status is not a substitute for this assessment All 38 Acute Presentations: 20 of these to be covered by WPBA during CT1-2 as detailed on p17 of this Workbook. The remaining 18 to be covered by WPBA or by e-learning, reflection, teaching etc o 8 by the end of CT2 o And all 18 by the end of CT3 NB: The e-learning modules are designed to help you pass MCEM; another reason not to leave them for CT3. All 45 DOPS: 39 by the end of CT2 as detailed on p21 of this Workbook. All 45 by the end of CT3. o Pacing and Cardioversion made by assessed by simulation. 19 ANAESTHESIA FOR ACCS Within the ACCS anaesthesia module the trainee must achieve the Initial Assessment of Competence (IAC). The 17 WPBAs that make up the IAC are listed under Practical Procedures (see next section). Date Signature and name of supervisor Initial Test of competency passed 20 21 PRACTICAL PROCEDURES There is a list of 44 Practical procedures in the ACCS Curriculum; 39 should be completed by the end of the second year. Some procedures and their assessment are specific to certain elements of the ACCS programme and a specific type of WPBA has been recommended: these have been indicated in brackets using the key below. These include the 17 that are associated with the Anaesthetic Initial Assessment of Competence. Mi, A = Mini-CEX(Anaesthetic), D = DOPs, C = CBD Practical procedures 1. Arterial cannulation 2. Peripheral venous cannulation 3. Central venous cannulation 4. Arterial blood gas sampling ACCS Module WBA type Date Modular (Clinical) supervisor ICM (D) ICM (D) ICM (D) ICM (Mi,D) 5. Lumbar puncture 6. Pleural tap and aspiration 7. Intercostal drain: Seldinger 8. Intercostal drain: Open 9. Ascitic tap 10. Abdominal paracentesis 11. Airway protection 12. Basic and advanced life support EM (D) Anaes (D) 13. DC Cardioversion 22 14. Knee aspiration 15. Temporary pacing (external/ wire) 16. Reduction of dislocation/ fracture EM (D) 17. Large joint examination 18. Wound management 19. Trauma primary survey EM (D) EM (D) 20. Initial assessment of the acutely unwell 21. Secondary assessment of the acutely unwell 22. Connection to a mechanical ventilator 23. Safe use of drugs to facilitate mechanical ventilation 24. Managing the patient fighting the ventilator 25. Monitoring Respiratory function ICM (D) ICM (C) ICM (C) ICM (C) Anaesthesia Initial Assessment of Competence (IAC) - as listed below from Preoperative assessment to Emergency surgery 26. Preoperative assessment 27. Management of spontaneously breathing patient 28. Administer anaesthesia for laparotomy Anaes (A) Anaes (A) Anaes (A) 23 29. Demonstrate RSI 30. Recover patient from anaesthesia 31. Demonstrate function of anaesthetic machine 32. Transfer of patient to operating table 33. Technique of scrubbing up and donning gown and gloves 34. Basic competences for pain management 35. Patient Identification 36. Post op N&V 37. Airway assessment 38. Choice of muscle relaxants and induction agents 39. Postoperative analgesia 40. Postoperative oxygen therapy 41. Emergency surgery 42. Safe use of vasoactive drugs and electrolytes 43. Deliver a fluid challenge safely to an acutely unwell patient 44. Describe actions required for accidental displacement of tracheal tube or tracheostomy Anaes (A) Anaes (A) Anaes (D) Anaes (D) Anaes (D) Anaes (D) Anaes (C) Anaes (C) Anaes (C) Anaes (C) Anaes (C) Anaes (C) Anaes (C) ICM (Mi,C) ICM (C) ICM (C) 24 Acute Medicine Paperwork Contents of this section: Structured Training Report form (to be completed at the end of the module) Induction Appraisal Form (to be completed at the start of the module) ACAT Form DOPS form MiniCEX form CbD form MSF Guidelines MSF form MSF Results Summary Please note that Multiple Consultant Reports (MCRs) are not required for ACCS, though ACCS-Medicine trainees may choose to do them. Recommended Reading / Useful Websites: The Oxford Handbook of Acute Medicine And / or The Oxford Handbook of Clinical Medicine Each £25-£30 available on Amazon 25 Structured Training Report for Acute Medicine Module The clinical/modular supervisor must complete this STR, having reviewed the trainee’s learning portfolio and WPBAs. Alternatively please substitute a print out of the STR from the Medicine e Portfolio. Current Placement Base Hospital/Department Dates Clinical supervisor WPBA in Current Placements Assessment Number Comments Mini-CEX (min 3 in 6 months) DOPs (min 5 in 6 months) List procedures included in DOPs and ensure they are signed off in Practical procedures CBD (min 3 in 6 months) ACAT (min 3 in 6 months) MSF 26 Experiential outcomes (please review evidence in learning portfolio) Comments Major Presentations (at least 2 out of 6) Acute Presentations: WPBAs (at least 10 of the 38) Acute Presentations: ACAT, e-learning, Reflective Entries, Teaching, Audit (at least 8 of the 38) Log book Clinical Governance/Audit Exams / Other Educational Achievements Life Support Courses 27 Other Courses Other Achievements Other outcomes to be considered that may not be in the learning portfolio. (e.g. Critical Incidents, Complaints) Summary of Trainees Assessment Supervisor to complete. Please attach evidence if available to support opinions or give examples of behaviours. Pen Picture of Trainee: Clinical Professionalism Communication Academic Endeavour/Learning 28 I confirm that this is an accurate description/summary of this trainee’s learning Portfolio and WPBA, covering the period from ………………..to ………………. Strengths of Trainee Suggestions for improvement Supervisor Name and Signature Date: Trainee Signature Date: Induction Appraisal Form (ACCS Acute Medicine Attachment) Trainee: Meeting Date: Timetable of regular weekly fixed commitments eg ward rounds, clinics, etc 29 DAY Monday: AM PM Teaching etc Tuesday: Wednesday: Thursday: Friday: Out of hours work: Arrangements for senior review of admissions: Are there any other induction considerations to be taken into account? e.g. duties of the placement(s); arrangements for clinical supervision; academic and welfare support: What are the objectives for the trainee, for the ACCS curriculum? What evidence will be used to ensure these objectives have been met? Main Curriculum Objectives and Evidence of Achievement: These are documented fully in the ACCS handbook, but by the end of the attachment the trainee must be able to provide a minimum of:3 x Acute Care Assessment Tools (ACAT) 30 3 x Case Based Discussions (CBD) 3 x Clinical Evaluation Exercises (CEX) 5 x Directly Observed Procedures (DOPS) A Multi-Source Feedback: 360o Team Assessment of Behaviour (MSF) Completed Workplace Assessments In addition:- Assessments must include Acute Coronary Syndrome. - Should aim to see as many of the “top 20 presentations” as possible. Top 20 Acute Presentations: Abdominal Pain* Acute Back Pain Blackout / Collapse Vomiting / nausea Weakness / paralysis Breathlessness* Chest Pain* Confusion Cough Diarrhoea Falls Fever Headache Rash Palpitations Fits/ Seizure Poisoning Limb Pain/swelling Jaundice Haematemesis / Melaena * These presentations are required to be assessed during the EM module and so cannot count towards the 10 required for AM. Generic Competencies: These are as documented in the ACCS handbook. What learning methods will be used to meet these objectives? Is any study leave planned? Are there any training concerns at this stage? Supervisor's Signature Trainee’s Signature 31 Acute Care Assessment Tool (ACAT) Instructions ACAT Instructions: A different observer for each assessment Observers can be any doctor from SpR grade and above, who was responsible for the supervision of the take you are being assessed on The process is trainee led (choosing the take period) An ACAT should take no longer than 15 minutes, and this includes the feedback given over the different sections of the ACAT assessment forms The completed ACAT forms should be entered onto the trainee’s ‘e’ portfolio. Clinical assessment Quality of History and Examination to arrive at appropriate differential diagnoses Medical record keeping Quality of recording of patient encounters on the take, and including drug and fluid prescriptions Investigations and referrals Quality of a trainee’s choice of investigations, and referrals over a take period Management of critically ill patient Quality of treatment given to critically ill patients encountered on the take (assessment, investigations, urgent treatment administered, involvement of appropriate colleagues including senior) Prioritisation of cases and issues within the take, ensuring sickest patients seen first and the patient’s most pressing issues are dealt with initially. Time management Recognition of the quality of a colleague’s initial clerking to inform how much further detail is needed. A full repeat clerking is not always needed by a more senior doctor. Management of Take / Team working Appropriate relationship with and involvement of other health professionals Clinical leadership Appropriate delegation and supervision of junior staff. Handover OVERALL CLINICAL JUDGEMENT Quality of the handover of care of patients from the take to the relieving team. If patients have been transferred to a different area of care then this applies to the quality of the handover to the new team. Quality of the trainee’s integrated thinking based on clinical assessment, investigations and referrals resulting in the patients’ management plan 32 33 34 35 36 37 38 RCP Guidelines for completing a MSF assessment Dear Colleague, Name of ‘Rater’: Please write name of ‘rater’ here The Royal Colleges of Physicians (UK) are now using multisource feedback (MSF), otherwise known as 3600 assessment, to assess doctors in training. MSF assessment is a method of assessing generic skills such as communication, leadership, team working, teaching, punctuality and reliability. This allows objective systematic collection and feedback of performance data on an individual, which is derived from a number of stakeholders in their performance. This assessment method has been shown, in a UK pilot study, to provide a reliable rating of an individual doctor. ‘Raters’ are people with whom the doctor being assessed works and this includes nurses, other doctors, secretaries and other clerical staff and other allied health professionals. The data from 20 ‘raters’ forms is put together to provide the doctor with structured feedback about their performance. You have been asked to assess: Please write name of doctor to be assessed here What is required of you? 1. You have been selected by the trainee or their educational supervisor to assess the trainee. 2. We would be grateful if you would complete the accompanying form about the trainee. MSF is used to assess the behaviour, team working and communication skills of trainees. It is NOT an assessment of knowledge or practical skills. 3. Ordinarily the trainee will not be able to identify you and will not see your individual responses. The trainee’s educational supervisor will collate the information from all of the MSF assessments onto a single summary form, which will be used to give the trainee feedback. Trainees will not normally see any individual responses/forms or scores. In the event of a legal challenge the Data Protection Act may allow the information to be released, but should not be released until the legal process has run its course. 4. Please score the trainee from 1 (extremely poor) to 9 (extremely good). A score of 13 would be considered unsatisfactory, 4-6 satisfactory and 7-9 would be considered above that expected, for a trainee at the same stage of training and level of experience. You must justify each score of 1-3 with at least one explanation/example in the comments box, failure to do so will invalidate the assessment. If you feel unable to comment on an aspect you may mark the ‘Don’t know’ box. 5. If you feel, for whatever reason, that the trainee doctor falls below what you believe to be a minimum standard for a qualified doctor who is training to be a consultant it is important for you to make this clear on the form. 6. If you have had insufficient contact with the trainee to assess certain aspects then please fill in the ‘Don’t know’ box. 7. Please make written comments to supplement or explain your scoring if you think this may be helpful, you must do this for all scores of 1-3. Please write clearly. 8. When you have FULLY completed the form please return it in the envelope provided to the trainee’s educational supervisor, NOT the . This process will be conducted sensitively and carefully so you should feel free to give honest answers to questions, as this is fundamental to the success of the process. © 2008 Royal Colleges of Physicians - modified for use in Wales 39 How to complete the form Your completed form will be scanned to enable a quick and accurate analysis of results, to aid this process please keep the following in mind: 1. 2. 3 4. Try not to fold your form Only use pens with black or dark blue ink & print firmly Only write in allocated areas on the form - if you have any additional comments please use a separate sheet of paper For optimum accuracy print in capital letters / numbers (where applicable) and avoid contact with the edge of the box. For example: A B C D E F G H 5. I J K L M N O P 1 2 3 4 5 6 7 8 9 Shade circles like this: Mark any mistakes made like Please detach the completed MSF assessment form and put it in the envelope provided, seal it, and either hand it to the educational supervisor or put it in the internal post to them. Do NOT give the completed form directly to the trainee . Thank you for your help. © 2008 Royal Colleges of Physicians - modified for use in Wales 41 RCP MSF feedback and summary form of trainee’s scores This form is to be completed by the educational supervisor at the end of the 6 month module Trainee’s GMC number: Name of trainee: Educational supervisor’s name: Medicine Attachment: Form to be completed by the educational supervisor before meeting with the trainee: Items Number of “raters” who scored item Range of “raters” scores Mean “raters” score Self score Any score of 1-3 or “Yes”for item 6? Attitude to staff Attitude to patients Reliability and Punctuality Communication skills: patients Communication skills: colleagues 42 Honesty and integrity, do you have any concerns? Team player skills Leadership skills Overall professional Competence Grade of “raters” Comments from “raters” 43 Future recommendations for training: Signature: Date: Trainee Educational Supervisor 44 Emergency Medicine Paperwork Contents of this section: Structured Training Report form (to be completed at the end of the module) Training Agreement Personal Development Plan MSF Form DOPS form Formative CbD form Summative CbD form Formative MiniCEX form Summative MiniCEX form ACAT-EM form Recommended Reading / Useful Websites: The Oxford Handbook of Emergency Medicine £25-£30, available on Amazon and elsewhere 45 College of Emergency Medicine Structured Training Report for ACCS EM CT1 The Educational Supervisor must complete this STR, having reviewed the trainee’s e-portfolio Trainees Name and GMC Number Educational Supervisor name and GMC Number Deanery / School Wales Training Unit GMC programme /Post approval number Date of assessment Period covered in this assessment, start and end dates ARCP decision tool for EM CT1 Assessments and number required Number completed Outcome Comments Common Competences CC 1-25 At least 50% to level 2 in CT1&2 Please see section below Core Major Presentations Adult (CMP1-6) 2/6 summative in EM CT1 Core Acute Presentations CAP Adults 1-38 5/38 summative in CT1, in specified topics X1 ACAT-EM covering 5/38 APs Additional 10/38 using ACAT, e-learning etc Adult Practical Procedures = 45 5 EM DOPs required (4 specified + additional) Min assessments in EM CT1 = 13 2 MPs, 5 APs, 1 ACAT, 5 DOPs Management and leadership 46 Examinations = MCEM A (not mandatory) Safeguarding Children Level 1&2 (not mandatory) ALS-Provider Experience 800 patient in 6/12 EM Please review trainees log book or equivalent* MSF Other outcomes to be considered Activity Date Outcome Comments PDP Educational achievements Evidence of reflective practice Critical incidents Complaints Periods of absence from the post, include sick leave Out of programme time, but not annual leave * trainee must provide either an hard copy or electronic log book, indicating number of patients seen and in what clinical areas, e.g. resus, majors, paeds or minors 47 Common Competencies progression Completion of the EM WPBA tools on the e-portfolio will automatically populate the trainee’s common competences framework. Using this framework and knowledge of the trainees competence against the common competency curriculum the following table should describe the level at which the trainee is working at present i.e. level 1-4. Domain Competence level 1-4 Comments (if any) History taking Clinical examination Therapeutics and safe prescribing Time management and decision making Decision making and clinical reasoning The patient as central focus of care Prioritisation of patient safety in clinical practice Team working and patient safety Principles of quality and safety improvement Infection control Managing long term conditions and promoting patient self-care Relationships with patients and communication within a consultation Breaking bad news Complaints and medical error Communication with colleagues and cooperation Health promotion and public health Principles of medical ethics and confidentiality 48 Valid consent Legal framework for practice Ethical research Evidence and guidelines Audit Teaching and training Personal behaviour Management and NHS structure Strengths of trainee Weaknesses of trainee Suggestions for development Issues not covered elsewhere Does the ES recommendation to ARCP panel for this trainee to progress to next stage of training Yes No If no, reasons why and specific areas that need to be addressed ES Name and Signature Trainee Signature Date: Date: 49 Training Agreement for ACCS EM and Non-EM Trainees This is a training agreement between the CT1/2 trainees and their educational supervisors in the emergency department. Training agreement declaration As a trainee I understand and agree that I shall attend/complete the following training requirements during my placement in the ED: Develop a personal educational plan with my educational supervisor at the start of my placement. Read the curriculum produced by the College of Emergency Medicine (CEM) Complete the required Workplace based assessments: Summative assessments should only be completed by Consultants or Associate Specialists. Formative assessments may be completed by registrars as well as consultants. 1. 2 Summative Assessments (Mini-CEX OR CBD) by a Consultant on 2 of the Major Presentations using the specific summative Mini-CEX or generic summative CBD forms. 2. 5 Summative Assessments on the following 5 Acute Presentations (Chest Pain, Abdominal Pain, Mental Health, Head Injury, Breathlessness) using the specific summative Mini-CEX or generic summative CBD forms and completed by Consultants. 3. The above assessments will consist of a minimum of 4 Mini-CEX and 3 CBDs. 4. 1 x ACAT-EM which may cover up to 5 additional Acute Presentations (not including the 5 specified in point 2) 5. 5x DOPS (using specific DOPs forms to include Airway, Wound management, Primary Survey in trauma, Joint or fracture manipulation + one other from ACCS list of practical procedures) 6. 10 additional assessments of acute presentations using a combination or ■ ■ ■ e-learning reflective entries teaching and audit assessments 50 additional ACAT-EMs 7. 1 x MSF (minimum of 10 to include 3 Consultants) Participate fully in the educational programme of the ED and be prepared to spend some of my own time on educational activities, including audit Complete promptly all training and assessment documentation, including my Portfolio of evidence and log book; and participate as required in assessment meetings, i.e. ARCP I understand that it is my responsibility to: Familiarise myself with the training programme Ensure that I request study time in good time and complete the relevant trust leave form/online request so that suitable arrangements can be made within the ED Arrange my 3 meetings and sign off (Structured Training Form) with my educational supervisor As a trainer I understand and agree that: The trainee is working with a ACCS focus in the ED with appropriate supervision I will do my best to see that the trainee receives all the support which will enable them to train successfully I will develop a personal educational plan with my trainee at the start of his/her placement. This plan will take into account their current training needs and the time and resources available I will meet with the trainee on at least 3 separate occasions, at the beginning, mid point and end of their placement for appraisal I will complete a structured training report prior to the trainee's ARCP Trainee's name and signature: Trainer's name and signature: Date: 51 Personal Development Plan Trainee name: What development needs and goals do I have? Explain the need and goal Training number: How will I address them? Explain the action you intend to take & what resources you will need Date by which I plan to achieve the goal Date agreed for achieving the goal The outcome How will you show that you have achieved the goal? Completed Completion agreed by Your supervisor (date & sign) COLLEGE OF EMERGENCY MEDICINE MULTI-SOURCE FEEDBACK (MSF) This form is completely anonymous. Trainee name: Grade of assessor: UNKNOWN Not Observed Date / / 1 2 3 4 5 Performance Performance Partially Meets Expectations Performance Performance Exceeds Expectations Performance Consistently Exceeds Expectations Does Not Meet Expectations Meets Expectations Good Clinical Care 1 Medical knowledge and clinical skills 2 Problem-solving skills 3 Note-keeping – clarity; legibility and completeness 4 Emergency Care skills 1-5 or UK Comments on this doctors clinical care Relationships with Patients 1 Empathy and sensitivity 2 Communicates well with all patient groups 3 Treats patients and relatives with respect 4 Appreciates the pyscho-social aspects of patient care 5 Offers explanations Comments on this doctors relationships with patients 1-5 or UK Comments Relationships with Colleagues 1 Is a team-player 2 Asks for others’ point of view and advice 3 Encourages discussion Empathy and sensitivity 4 Is clear and precise with instructions 5 Treats colleagues with respect 6 Communicates well (incl. non-verbal communication) 7 Is reliable 8 Can lead a team well 9 Takes responsibility 10 “I like working with this doctor” 1-5 or UK Comments on this doctors relationships with colleagues Teaching and Training 1 Teaching is structured 2 Is enthusiastic about teaching 3 This doctor’s teaching sessions are beneficial 4 Teaching is presented well 5 Uses varied teaching skills 1-5 or UK Comments on this doctors teaching and training skills Global ratings and concerns 1 Overall how do you rate this Dr compared to other ST1 Drs 2 How would you rate this trainees performance at this stage of training 3 Do you have any concerns over this Drs probity or health? 1-5 or UK General comments 54 COLLEGE OF EMERGENCY MEDICINE MULTI-SOURCE FEEDBACK (MSF) Trainee name: Summary of Responses UNKNOWN Not Observed Date / / 1 2 3 4 5 Performance Performance Partially Meets Expectations Performance Performance Exceeds Expectations Performance Consistently Exceeds Expectations Does Not Meet Expectations Meets Expectations Good Clinical Care 1 Medical knowledge and clinical skills 2 Problem-solving skills 3 Note-keeping – clarity; legibility and completeness 4 Emergency Care skills 1 2 3 4 5 UK Comments 1 2 3 4 5 UK Comments Comments on this doctors clinical care Relationships with Patients 1 Empathy and sensitivity 2 Communicates well with all patient groups 3 Treats patients and relatives with respect 4 Appreciates the pyscho-social aspects of patient care 5 Offers explanations Comments on this doctors relationships with patients 55 Relationships with Colleagues 1 Is a team-player 2 Asks for others’ point of view and advice 3 Encourages discussion Empathy and sensitivity 4 Is clear and precise with instructions 5 Treats colleagues with respect 6 Communicates well (incl. non-verbal communication) 7 Is reliable 8 Can lead a team well 9 Takes responsibility 10 “I like working with this doctor” 1 2 3 4 5 UK Comments Comments on this doctors relationships with colleagues Teaching and Training 1 1 Teaching is structured 2 Is enthusiastic about teaching 3 This doctor’s teaching sessions are beneficial 4 Teaching is presented well 5 Uses varied teaching skills 2 3 4 5 UK 4 5 UK Comments on this doctors teaching and training skills Global ratings and concerns 1 Overall how do you rate this Dr compared to other ST1 Drs 2 How would you rate this trainees performance at this stage of training 3 Do you have any concerns over this Drs probity or health? 1 2 3 General comments Summarised by: ………………………………………………………………………. Educational Supervisor 56 College of Emergency Medicine Direct Observation of procedural Skills – DOPs Trainee name: Assessor: Assessor GMC No: Grade of assessor: Date / / Procedure observed (including indications) Please TICK to indicate the standard of the trainee’s performance in each area Not observ ed Further core learning needed Demonstrates good practice Must address learning points highlight ed below Should address learning points highlighte d below Demonstrates excellent practice Indication for procedure discussed with assessor Obtaining informed consent Appropriate preparation including monitoring, analgesia and sedation Technical skills and aseptic technique Situation awareness and clinical judgement 57 Safety, including prevention and management of complications Care /investigations immediately post procedure Professionalism, communication and consideration for patient, relatives and staff Documentation in the notes Completed task appropriately Things done particularly well Learning points Action points Assessor Signature: Trainee Signature: 58 College of Emergency Medicine Formative Case Based Discussion CbD Trainee name: Assessor: GMC assessor No: Grade of assessor: Date Not observed / Presentation – please see curriculum for number Case discussed (brief description) Please TICK to indicate the standard of the trainee’s performance in each area / Further core learning needed Demonstrates good practice Must address learning points highlighted below Should address learning points highlighted below Demonstrates excellent practice Record keeping Review of investigations Diagnosis Treatment Planning for subsequent care (in patient or discharged patients) Clinical reasoning Patient safety issues Overall clinical care 59 Things done particularly well Learning points Action points Assessor Signature: Trainee Signature: 60 College of Emergency Medicine Summative Case Based Discussion CbD Trainee name: Assessor: GMC assessor No: Grade of assessor: Date / Record keeping Records should be legible and signed. Should be structured and include provisional and differential diagnoses and initial investigation & management plan. Should record results and treatments given. Review of investigations Undertook appropriate investigations. Results are recorded and correctly interpreted. Any Imaging should be reviewed in the light of the trainees interpretation Diagnosis The correct diagnosis was achieved with an appropriate differential diagnosis. Were any important conditions omitted? Not observed Expected behaviours Unsuccessful Presentation – please see curriculum for number Successful Case discussed (brief description) / 61 Treatment Emergency treatment was correct and response recorded. Subsequent treatments appropriate and comprehensive Planning for subsequent care (in patient or discharged patients) Clear plan demonstrating expected clinical course, recognition of and planning for possible complications and instructions to patient (if appropriate) Clinical reasoning Able to integrate the history, examination and investigative data to arrive at a logical diagnosis and appropriate treatment plan taking into account the patients co morbidities and social circumstances Patient safety issues Able to recognise effects of systems, process, environment and staffing on patient safety issues Overall clinical care The case records and the trainees discussion should demonstrate that this episode of clinical care was conducted in accordance with good clinical practice and to a good overall standard Overall Successful Unsuccessful If more than two “not observed” then unsuccessful 62 Things done particularly well Learning points Action points Assessor Signature: Trainee Signature: 63 College of Emergency Medicine Formative Mini-Clinical Evaluation Exercise - Mini-CEX Trainee name: Assessor: Assessor GMC no. Grade of assessor: Date Case discussed (brief description) Please TICK to indicate the standard of the trainee’s performance in each area Not observed / / Presentation – please see curriculum for number Further core learning needed Demonstrates good practice Must address learning points highlighted below Should address learning points highlighted below Demonstrat es excellent practice Initial approach History and information gathering Examination Investigation Clinical decision making and judgment Communication with patient, relatives, staff 64 Overall plan Professionalism Things done particularly well Learning points Action points Assessor Signature: Trainee Signature: 65 College of Emergency Medicine Summative Mini-Clinical Evaluation Exercise - Mini-CEX Trainee name: Assessor: Assessor GMC no. Grade of assessor: Date Case discussed (brief description) / / Presentation – please see curriculum for number Descriptors of poor performance Successf ul unsucce ssful Initial approach History and information gathering History taking was not focused Did not recognise the critical symptoms, symptom patterns Failed to gather all the important information from the patient, missing important points Did not engage with the patient Was unable to elicit the history in difficult circumstances- busy, noisy, multiple demands Examination Investigation Failed to detect /elicit and interpret important physical signs Did not maintain dignity and privacy Was not discriminatory in the use of diagnostic tests 66 Clinical decision making and judgment Communication with patient, relatives, staff Did not identify the most likely diagnosis in a given situation Did not construct a comprehensive and likely differential diagnosis Did not correctly identify those who need admission and those who can be safely discharged. Did not recognise atypical presentation Did not recognise the urgency of the case Did not select the most effective treatments Did not make decisions in a timely fashion Decisions did not reflect clear understanding of underlying principles Did not reassess the patient Did not anticipate interventions and slow to respond Did not review effect of interventions Communication skills with colleagues Did not listen to other views Did not discuss issues with the team Failed to follow the lead of others when appropriate Rude to colleagues Did not give clear and timely instructions Inconsiderate of the rest of the team Was not clear in referral process- was it for opinion, advice, or admission Communication with patients Did not elicit the concerns of the patient, their understanding of their illness and what they expect Did not inform and educate patients/carers Did not encourage patient involvement/ partnership in decision making Did not respect confidentiality Did not protect the patients dignity 67 Overall plan Insensitive to patients opinions/hopes/fears Did not explain plan and risks in a way the patient could understand Was slow to progress the case Did not ensure patient was in a safe monitored environment Did not anticipate or recognise complications Did not focus sufficiently on safe practice Did not follow published standards guidelines or protocols Did not follow infection control measures Did not safely prescribe Professionalism Overall Successful Unsuccessful (this outcome if any one criteria unsuccessful Things done particularly well Learning points Action points Assessor Signature: Trainee Signature: 68 College of Emergency Medicine The Acute Care Assessment Tool (ACAT-EM) form Trainee name: Assessor: Assessor GMC no. Grade of assessor: Date Setting, Acute presentations covered (5 max for EM) / / Timing, duration and level of responsibility Please TICK to indicate the standard of the trainee’s performance in each area Not observed Further core learning needed Demonstrates good practice Must Should address address learning learning points points highlighted highlighted below below Demonstrates excellent practice Clinical Assessment Medical record keeping Investigation and treatment of the critically ill patient Time management Management of the team 69 Clinical leadership Patient safety Handover Overall Clinical Judgement Which aspects were done well Learning points Unsatisfactory acute presentation? – which Plan for further AP assessment, specify WPBA tool and review date Trainees Comments Action points Assessor Signature: Trainee Signature: 70 ACAT –EM Assessment Domains Description Clinical assessment and clinical topics covered Quality of history and examination to arrive at appropriate diagnosis- made by direct observation in different areas especially in the resuscitation room. Medical record keeping Quality of recording of patient encounters including drug and fluid prescriptions No more than 5 AP should be covered in each ACAT and this should involve a review of the notes and management plan of the patient. Investigations and Quality of trainees choice of investigations and referrals referrals Management of patients Quality of treatment given (assessment, investigation, urgent treatment given involvement of seniors) Time management Prioritisation of cases , doesn’t spend too much time with any one patient Management of take/team working Appropriate relationship with and involvement of other health professionals Clinical leadership Appropriate delegation and supervision of junior staff Handover Quality of handover of care of patients between EM and in patient teams and in house handover including obs/CDU ward Patient safety Able to recognise effects of systems, process, environment and staffing on patient safety issues Overall clinical judgement Quality of trainees integrated thinking based on clinical assessment, investigations and referrals. safe and appropriate management, use of resources sensibly 71 Anaesthesia Paperwork Contents of this section: Structured Training Report form (to be completed at the end of the module) Learning Agreement ACCS Trainee Appraisal Record MSF Instructions MSF form MSF Summary form Recommended Reading / Useful Websites: The Oxford Handbook of Anaesthesia o Approx £30, available on Amazon and elsewhere. Junior Anaesthetists of Wales (JAW) – on Facebook and Twitter Welsh School of Anaesthesia o www.welshschool.co.uk 72 Structured Training Report for Anaesthesia Module Current Placement Base Hospital/Department Dates Clinical supervisor 1. Basic Level Training BASIS of Anaesthetic Practice – Please tick all completed units of training to date Preoperative Assessment Premedication Induction of general anaesthesia Intra-operative Care Post-operative and recovery room care Introduction to anaesthesia for emergency surgery Management of Cardiac & Respiratory Arrest Control of Infection Initial Assessment of Competence signed Primary FRCA Status Date: Date passed No. of attempts MCQ SOE OSCE Other Specialty Examinations Achieved and Dates: 73 2. Workplace based assessments tools (WPBAs) completed: Assessment Number Summary of Comments Anaes –CEX DOPs CBD MSF Please include MSFSummary Sheet as an appendix to this report 3. Experiential Outcomes Activity 1 Log-Book Date/s Outcomes Comment Total Cases in 6 month module: Expected activity achieved / not achieved. 2 Audits Completed / not completed / presented 3 Research projects work in progress/completed 4 Publications 5 Teaching 74 6 Management Development 7 Presentations 8 Courses attended Other qualifications gained (e.g. ATLS, APLS, PGCE) 4.Other outcomes Date/s 1 Reported adverse incidents Outcome Comment Resolved/pending (The PG Dean in Wales has instructed that all No case to find/ critical incidents involving accountable a named trainee must be reported at their ARCP) 2 3 Complaints / Resolved/pending disciplinary issues/ No case to find/ litigation accountable Other A 75 No. of days sick leave taken in the 6 months………………….. (Please verify with department secretary / manager) Sections 5-8 will usually be completed by the College Tutor. The College Tutor should be guided by the results of MSF and/or other sources which will endeavour to ensure that, as far as possible, ratings are recorded objectively. If a trainee’s performance is deemed below average or un-acceptable in the following sections, please outline how this conclusion was reached and provide supporting documentation where possible. 5. Clinical Skills - Based on MSF and other sources Good: * Below average: * Un-acceptable: Performing to expected standard sometimes performance is inadequate often performance is inadequate History taking Physical examination Investigation & Diagnosis Judgement & Patient Management Practical Skills Communications Skills 76 6. Knowledge (please tick the appropriate boxes) Good: * Below average: * Un-acceptable: Performing to expected standard sometimes performance is inadequate often performance is inadequate Basic Science Clinical 7. Attitudes (please tick the appropriate boxes) Good: * Below average: * Un-acceptable: Performing to expected standard sometimes performance is inadequate often performance is inadequate Reliability Initiative Administration Time Keeping 77 8.Relationships (please tick the appropriate boxes) Good: * Below average: * Un-acceptable: Performing to expected standard sometimes performance is inadequate often performance is inadequate Patients Colleagues Other Staff Would you expect a satisfactory outcome for the ARCP? Y / N If you feel the ARCP is not going to be satisfactory the Programme Director must be contacted well in advance of the ARCP interview. 78 Strengths of Trainee: Suggestions for improvement: Comments: Signed by: _________________________ (Educational Supervisor) Date ________________ Signed by: _________________________ (College Tutor) Date ________________ Signed by: _________________________ (Trainee) Date ________________ 79 Welsh School of Anaesthesia LEARNING AGREEMENT Our goal is to provide an ideal working and learning environment. Postgraduate medical education takes time and effort by the teachers and learners. We aim to provide: A named educational supervisor: Dr ……………………………… A comprehensive Induction Program Regular teaching in protected time Supervised operating theatre lists Appropriate clinical supervision at all times Opportunities to attend and present at journal club An adequate library, computers with internet access and other learning resources Regular constructive feedback An appraisal system Annual assessments For your part we expect you to: Familiarize yourself and adhere to the duties and responsibilities of a doctor registered with the General Medical Council and outlined in the Council’s document “Good Medical Practice”. Download and familiarise yourself with the CCT in Anaesthesia document (and ACCS Core Training document if appropriate) Download and familiarise yourself with the contents of the Gold Guide to specialty training Familiarize yourself with the anaesthetic departments’ guidelines and protocols. Participate fully in your clinical and educational programme Be prepared to spend some of your own time on educational activities Develop and maintain a learning portfolio Book appointments for regular appraisals Be receptive to feedback and develop your personal learning plan with your appraiser. Complete promptly all training and assessment documentation required by your educational supervisor Seek help from your appraiser or educational supervisor if you have any problems Maintain standards of punctuality, cleanliness and appearance expected of a healthcare professional Be responsible and considerate when booking leave 80 Trainee name:___________________________ Signature: ____________________ Date: ________________ Educational Supervisor Name:__________________Signature: _____________________ Date : ________________ Please keep the completed original form in your portfolio and give a photocopy to your Educational Supervisor. 81 WELSH SCHOOL OF ANAESTHESIA ACCS TRAINEE APPRAISAL RECORD Name: ………………………………………………. Parent Specialty: …………………………………… Rotation Details: Aug 20… – Jan 20… : ……………………………… CT1 Feb – July 20… : ……………………………… CT1 Aug 20… – Jan 20… : ……………………………… CT2 Feb – July 20… : ………………………………. CT2 Aug 20… – July 20… : ………………………………. CT Parent Specialty Pre-ACCS experience: Dates: ………………………………………………………………… ……………… Exams passed and dates: …………………………………. …………….. Exam planned and date: …………………………………. ……………… Resuscitation Training: ALS (required for all ACCS Trainees before CT2 ARCP) Provider Instructor No Booked APLS* (obligatory for EM only, before CT3 ARCP) Provider Instructor No Booked ATLS* (obligatory for EM only, before CT3 ARCP) Provider Instructor No Booked Registered with parent college Yes No Advised to Registered with RCoA (for e-learning) Yes No Advised to Portfolio Yes No Advised to *or equivalent 82 Section 2: 3 month appraisal 1) Progress towards Initial Competencies: 2) Logbook review: 3) Progress towards other objectives: 3) Feedback from trainers: 4) Has attendance at teaching sessions been satisfactory? 5) Study Leave Additional Comments: Signed: ………………………………………. Print: ……………………..Date: …………………… (Trainer) Signed: ……………………………………….. Print: ……………………Date: ……………………. (Trainee) 83 Section 3: 6 month appraisal 1) Certificate of Initial Competencies Achieved: 2) Logbook review: 3) Results of Multi-Source Feedback: 4) Completed Assessment Tools: DOPS (6) AnaesCEX (2) CbD (2) 5) Other achievements in this post: 6) Study Leave 7) Trainee Feedback Additional Comments: Signed: ………………………………………. Print: ……………………..Date: …………………… (Trainer) Signed: ……………………………………….. Print: ……………………Date: ……………………. (Trainee) 84 Welsh School of Anaesthesia Multi Source Feedback Instructions for Use Assessment subject 1. Select 12 people to complete an assessment form. 2. … assessors must be consultant anaesthetists, … must be anaesthetic support staff, recovery or ITU nurses, … must be other trainee anaesthetists and one secretary. 3. Ensure that each assessor is given an assessment form, an addressed reply envelope and an instruction sheet. 4. All assessment forms should be all distributed 2 weeks prior to your appraisal date. Assessor 1. 2. 3. 4. 5. Thank you for completing this form Your comments will be fed back anonymously Please be honest and include good and bad points as necessary Please keep the assessment form confidential Please return the completed form in the attached envelope to Dr ……………………….., Educational Supervisor, Dept. of Anaesthesia. 85 The Royal College of Anaesthetists Multi Source Feedback (MSF) Assessment Form Please complete the question using a cross (x). Please use black ink and CAPITAL LETTERS Trainee’s surname Trainee’s forename(s) GMC number GMC NUMBER MUST BE COMPLETED Observed by Signature GMC/NMC/HPC number Date Role GMC/NMC/HPC NUMBER MUST BE COMPLETED Which clinical setting have you primarily observed the doctor in? Theatre ICU A&E How do you rate this doctor in their: Delivery Suite Good Pain Clinic Satisfactory Other Needs to improve Unacceptable Unable to comment Knowledge, skills, performance 1. Ability to diagnose patient problems 2. Ability to plan patient care 3. Awareness of their own limitations 4. Ability to keep up to date with knowledge and skills 5. Responds to pain and distress in patients appropriately 6. Technical skills [appropriate to grade] 7. Ability to multitask and work effectively in a complex environment 86 8. Ability to manage time effectively / prioritise 9. Able to cope under stress 10. Willingness and effectiveness when teaching / training colleagues 11. Ability to take leadership role when circumstances required 12. Keeps clear, accurate, legible records contemporaneously Safety and quality 13. Contributes constructively to audit, appraisal and clinical governance 14. Safeguards and protects patients wellbeing 15. Responds promptly to risks posed by patients Communication, partnership and teamwork 16. Communication with patients 17. Communication with carers and/or family 18. Verbal communication with colleagues 19. Written communication with colleagues 20. Ability to recognise and value the contribution of others 21. Accessibility / reliability Maintaining trust 22. Respect for patients privacy, right for confidentiality 23. Polite, considerate and honest to patients 87 24. Treats patients fairly and without discrimination 25. Treats colleagues fairly and without discrimination 26. Honest and objective when appraising and assessing colleagues Are there any concerns about this doctor’s probity or health? Yes No If yes, please provide details Please add any additional comments If any boxes were marked with minor or major concerns, please explain why Signature Date 88 The Royal College of Anaesthetists Multi Source Feedback (MSF) Summary Form Clinical settings of observation: (Enter number of raters) Theatre ICU A&E Delivery Suite Pain Clinic Other Summary of raters’ responses: How the doctor was rated in their: Good Satisfactory Needs to improve Unacceptable Unable to comment Knowledge, skills, performance 1. Ability to diagnose patient problems 2. Ability to plan patient care 3. Awareness of their own limitations 4. Ability to keep up to date with knowledge and skills 5. Responds to pain and distress in patients appropriately 6. Technical skills [appropriate to grade] 7. Ability to multitask and work effectively in a complex environment 8. Ability to manage time effectively / prioritise 9. Able to cope under stress 10. Willingness and effectiveness when teaching / training colleagues 11. Ability to take leadership role when circumstances required 89 Summary of raters’ responses: How the doctor was rated in their: Good Satisfactory Needs to improve Unacceptable Unable to comment 12. Keeps clear, accurate, legible records contemporaneously Safety and quality 13. Contributes constructively to audit, appraisal and clinical governance 14. Safeguards and protects patients wellbeing 15. Responds promptly to risks posed by patients Communication, partnership and teamwork 16. Communication with patients 17. Communication with carers and/or family 18. Verbal communication with colleagues 19. Written communication with colleagues 20. Ability to recognise and value the contribution of others 21. Accessibility / reliability Maintaining trust 22. Respect for patients privacy, right for confidentiality 23. Polite, considerate and honest to patients 24. Treats patients fairly and without discrimination 25. Treats colleagues fairly and without discrimination 90 Summary of raters’ responses: How the doctor was rated in their: Good Satisfactory Needs to improve Unacceptable Unable to comment 26. Honest and objective when appraising and assessing colleagues Were there any concerns about this doctor’s probity or health? Yes No Summary of details from those with concerns: Summary of raters’ general comments: Summary of raters’ explanations of minor or major concerns: Signature Date Trainee Educational Supervisor Trainee’s surname Trainee’s forename(s) 91 Intensive Care Medicine Paperwork Contents of this section: Structured Training Report form (to be completed at the end of the module) MSF / TAB form Logbook Summary DOPS form CEX form CbD form Information for Educational Supervisors: Competency Level Descriptors (for Ed Sup information) Training Progression Grid Recommended Reading / Useful Websites: The Oxford Handbook of Critical Care £25-£30, available on Amazon and elsewhere 92 Structured Training Report for Intensive Care Medicine Module The educational/modular supervisor must complete this STR, having reviewed the trainee’s learning portfolio and WPBAs. Current Placement Base Hospital/Department Dates Clinical supervisor WPBA in Current Placement Assessment Number Comments Mini-CEX (min 3 in 6 months) DOPs (min 6 in 6 months) List procedures included in DOPs and ensure they are signed off in Practical procedures CBD (min 4 in 6 months) MSF (1 per placement) 93 Experiential outcomes (please review evidence in learning portfolio) Practical Procedure WBA Date Outcome Demonstrates aseptic peripheral DOPS venous cannulation Demonstrates aseptic arterial DOPS cannulation (+ local anaesthetic) Obtains an arterial blood gas sample DOPS or safely, interprets results correctly M CEX Demonstrates aseptic placement of DOPS central venous catheter Connects mechanical ventilator and DOPS selects initial settings Describes Safe Use of Drugs to CBD Facilitate Mechanical Ventilation Describes Principles of Monitoring CBD Respiratory Function Describes the Assessment of the CBD patient with poor compliance during Ventilatory Support (‘fighting the ventilator’) Prescribes safe use of vasoactive M CEX drugs and electrolytes or CBD Delivers a fluid challenge safely to CBD an acutely unwell patient Describes actions required for CBD accidental displacement of ETT or tracheostomy Comments COMPETENCY DOMAINS SUCCESSFULLY ACHIEVED Competency Domain (at a level appropriate for ACCS) Signature 1. Resuscitation and initial management of the acutely ill patient 2. Diagnosis, Assessment, Investigation, Monitoring and Data Interpretation 3. Disease Management 4. Therapeutic interventions / Organ system support in single or multiple organ failure 5. Practical procedures 6. Perioperative care 94 7. Comfort and recovery 8. End of life care 9. Transport 10. Patient safety and health systems management 11. Professionalism Summary of Trainee Assessment Supervisor to complete. Please attach evidence if available to support opinions or give examples of behaviours. Strengths of Trainee I confirm that this is an accurate description/summary of this trainee’s learning portfolio and WPBA, covering the period from ………………..to ………………. Supervisor Name and Signature Trainee Signature 95 Suggestions improvement Weaknesses for of Trainee Date: Date: ICM Multi Source Feedback (MSF) Team Assessment of Behaviour (TAB) Please use a CROSS (X) for each question and complete this form in BLOCK CAPITALS and BLACK ink. Trainee’s surname Trainee’s forename(s) GMC Number GMC NUMBER MUST BE COMPLETED Observed by Signature Date 96 Major or Serious Concerns Minor Concerns Comments No Concerns Domain Please provide feedback on professional behaviour including areas of excellence and areas for improvement NB: Any concerns must be commented on to allow constructive feedback and planning for improvement 1. Maintaining trust/ professional relationships with patients Listens Is polite and caring Shows respect for patients’ opinions, privacy, dignity and is unprejudiced 2. Verbal communication skills Gives clear, understandable information Speaks good English at an appropriate level for patient or relative 3. Team working/ working with colleagues Respects others’ roles Works constructively within team Effective handover Delegates appropriately Supportive of colleagues 97 4. Accessibility Accessible to all staff Does not shirk duty Responds when called Arranges cover for planned absence, notifies of unplanned absence Do you have any concerns about this doctor’s probity or health? Yes No If yes please explain on additional sheet Additional comments on doctor’s professional behaviour: ICM logbook summary Please use a CROSS (X) for each question and complete this form in BLOCK CAPITALS and BLACK ink. Trainee’s surname Trainee’s forename(s) GMC Number GMC NUMBER MUST BE COMPLETED Hospital placement: Duration of placement: 98 Total beds: Level of training: Speciality: Level 2: Core General Level 3: Mixed 2/3: Step 1 Step 2 Step 3 Cardiac Neuro Paeds Total unit admissions during placement: Data can be obtained from ICNARC database Event Local supervision Distant supervision Teaching Ward review Admission Lead ward round Cardiac arrest Trauma team Intra-hospital transfer Inter-hospital transfer Discussion with relatives End of life care/donation ICM logbook summary Airway & Lungs Procedure Local supervision Distant supervision Teaching Emergency intubation Percutaneous tracheostomy Bronchoscopy 99 Chest drain – seldinger Chest drain – blunt dissection Lung ultrasound Arterial cannulation Cardiovascular Central venous access – IJ Central venous access – SC Central venous access – Femoral Pulmonary artery catheter Non-invasive CO monitoring Echocardiogram Abdomen Ascitic drain/tap Sengstaken tube placement Abdominal ultrasound/FAST CNS Lumbar puncture Brainstem death testing Procedures performed should be appropriate to level of training; Experience of the all the above procedures is desirable but NOT essential FICM DOPS Assessment Form Trainee’s Surname Trainee’s Forename(s) GMC Number GMC NUMBER MUST BE COMPLETED Procedure Code Number Observed by 100 GMC NUMBER MUST BE COMPLETED GMC Number Date Signature of observing doctor Assessment: Practice was satisfactory Practice was unsatisfactory Tick one Tick Assessor’s signature Assessor’s signature one Expand on areas of good practice. You MUST expand on areas for improvement for each unsatisfactory score given. Example of good practice were: Areas of practice requiring improvement were: Further learning and experience should focus on: FICM CEX Assessment FormPlease complete this form in BLOCK CAPITALS and BLACK ink Trainee’s Surname Trainee’s Forename(s) GMC Number GMC NUMBER MUST BE COMPLETED Observation Code Number Observed by GMC Number Date GMC NUMBER MUST BE COMPLETED 101 Performance YES NO Comments Understands indications and contraindications for the procedure Tick Tick Comments Explained procedure to patient Tick Tick Comments Understands relevant anatomy Tick Tick Comments Satisfactory preparation for procedure Tick Tick Comments Communicated appropriately with patient and staff Tick Tick Comments Full aseptic technique Tick Tick Comments Satisfactory technical performance of procedure Tick Tick Comments Adapted to unexpected problems during procedure Tick Tick Comments Demonstrated adequate skill and practical fluency Tick Tick Comments Maintained Safe practice Tick Tick Comments Completed procedure Tick Tick Comments Satisfactory documentation of procedure Tick Tick Comments Issued clear post-procedure instructions to patient and staff Tick Tick Comments Maintained professional demeanour throughout procedure Tick Tick Comments Signature of supervising doctor 102 Clinical Setting: ICU HDU ED Ward Transfer Other Assessment: Practice was satisfactory Tick one Assessor’s signature Practice was unsatisfactory Tick one Assessor’s signature Expand on areas of good practice. You MUST expand on areas for improvement for each unsatisfactory score given. Examples of good practice were: Areas of practice requiring improvement were: Satisfactory Unsatisfactory Further learning and experience should focus on: 1. History taking and information gathering Tick Tick 2. Assessment and differential diagnosis Tick Tick Please grade the following areas: (Please see Domain Descriptors) 103 3. Immediate management and stabilisation Tick Tick 4. Further management and clinical judgement Tick Tick 5. Identification of potential problems and difficulties Tick Tick 6. Maintain safe practice for patient, trainee & staff Tick Tick 7. Communication with patient, staff and colleagues Tick Tick 8. Record keeping Tick Tick 9. Overall clinical care Tick Tick FICM CbD Assessment FormPlease complete this form in BLOCK CAPITALS and BLACK ink Trainee’s Surname Trainee’s Forename(s) GMC Number GMC NUMBER MUST BE COMPLETED Observation Code Number Observed by GMC Number Date GMC NUMBER MUST BE COMPLETED 104 Signature of supervising doctor Clinical Setting: ICU HDU ED Ward Transfer Other Assessment: Practice was satisfactory Tick one Assessor’s signature Practice was unsatisfactory Tick one Assessor’s signature Expand on areas of good practice. You MUST expand on areas for improvement for each unsatisfactory score given. Examples of good practice were: Areas of practice requiring improvement were: Further learning and experience should focus on: Satisfactory Unsatisfactory Special Focus of Discussion: 1. History taking and information gathering Tick Tick 2. Assessment and differential diagnosis Tick Tick Please grade the following areas: (Please see Domain Descriptors) 105 3. Immediate management and stabilisation Tick Tick 4. Further management and clinical judgement Tick Tick 5. Identification of potential problems and difficulties Tick Tick 6. Communication with patient, staff and colleagues Tick Tick 7. Record keeping Tick Tick 8. Overall clinical care Tick Tick Tick Tick 9. Understanding of the issues surrounding the clinical focus chosen by the assessor 106 107 A Career in Intensive Care Medicine Dr Alison Ingham - ICM lead for ACCS Intensive Care Medicine (ICM) is an exciting and dynamic career choice (I’m biased of course!). Hopefully you will enjoy your ACCS ICM placement so much, you will be thinking about further training in ICM. If so, here is how you go about it. You can apply to enter ICM higher specialist training following ACCS or core anaesthesia (CAT) or core medical training (CMT). You can, of course, dual with a second specialty, but more about that later. The training is divided into 3 stages: Stage 1 training: Stage 1 training is 4 years. This includes ACCS (or CAT / CMT) core training and years ST3 and ST4 of higher training. By the end of ST4 you will need to have completed the following: 1 year of Anaesthesia 1 year of Medicine (including Emergency Medicine) 1 year of ICM For example, a trainee coming from CMT, would probably need 1 year of ICM and 1 year of Anaesthesia in their ST3 and ST4 years. If you have done 3 years of ACCS Anaesthesia, you are likely to need 6 months in ICM and the other 6 months could be in any of the specialties. You get the idea. Stage 2 training: Stage 2 training is 2 years, ST5 and ST6. ST5 consists of specialist rotations, with 3 months in neuro ICU, 3 months in paediatric (PICU) and 3 months in cardiac ICU. The remaining 3 month block in that year may be flexible. Trainees dualling with anaesthesia will gain most of their neuro, paediatric and cardiac competencies in theatres during this year, as it is also counted towards their anaesthetic training. Trainees dualling with Medicine or Emergency Medicine will be based on the specialist ICUs. ST6 is a “special skills” year and is only undertaken by ICM single CCT trainees. Dual trainees will spend this year in their partner specialty. The special skills year could include research, teaching and training or further time in a specialist ICU. During stage 2 training, you will also have to pass the FFICM exam. Stage 3 training: This is one year and is similar to the old “advanced ICM training year”. You will start working in a more senior role and learning the skills needed to become a consultant. Dual Training: You can dual train with the following specialties: Acute Medicine Emergency Medicine Anaesthesia Renal Medicine Respiratory Medicine Luckily, getting a dual CCT does not double your training time. Instead it increases it from 7 to 8.5 years. Parts of your training will count towards both specialities and your training programme will be tailored by the appropriate Training Programme Directors. Application is stepped. This means that although you can apply for both specialties at the same time, you can only hold one offer, so application for the second specialty will be needed the following year. It does not matter which specialty you accept first, but both must be in the same Deanery. 113 Unfortunately you will have to keep two portfolios, one for each specialty. You may also have to get used to being at different stages of training in your two specialties – for example you might have finished stage one training in ICM (ST4) but still be finishing your ST3 year in your partner specialty. So why chose Wales? Words from Dr Chris Thorpe – Regional Advisor for ICM Wales is a diverse country that will give you a great life style as you build your future career. Wales offers something for everyone, from cosmopolitan towns and cities to stunning coastal locations. With affordable housing and welcoming communities it is an ideal place to achieve a work-life balance. It even has its own language, although it is not necessary to learn it to pursue training, employment or to live here. Wales is covered by a single Deanery which puts high quality training at the heart of medical careers. The Wales Deanery also holds an award for being the “most family-friendly”. The ICM specialist training scheme in Wales is funded directly by the Deanery which allows us to choose posts which will best benefit the trainee. This enables us to provide excellent posts in Anaesthesia and Medicine as well as ICM. Currently hospitals training at ST3-4 level are in Swansea, Newport, Bangor and Wrexham, with the ST5 year based in Cardiff. Other hospitals also provide training and placements may take in other units depending on the trainee’s needs. The ST6 year will be tailored according to whether the trainee is dual or single accrediting and the ST7 year is likely to be mainly in South Wales. The Specialist Training Committee and Deanery make support of the trainee central to their business and you can look forward to a carefully developed scheme that allows you to grow in experience and confidence as the years go by. You will experience a variety of Intensive Care Units and will emerge from the scheme a rounded and mature professional with the ability to take on a consultant role in both large and small hospitals. 114 Further Information For further information on ICM training and dual training in particular, please also see Dr Thorpe’s article on page 31 of the summer 2013 edition of the FICM newsletter, “Critical Eye”. http://www.ficm.ac.uk/sites/default/files/Critical%20Eye%204%20%20website%20version.pdf If you would like to talk to someone in more detail about ICM training, please contact either Dr Thorpe or myself. There will also be an ICM Faculty Tutor at each hospital within Wales who provide ACCS training, who will be able to help you. Dr Alison Ingham Alison.ingham@wales.nhs.uk Dr Chris Thorpe Chris.Thorpe@wales.nhs.uk 115