Appendix 1
advertisement

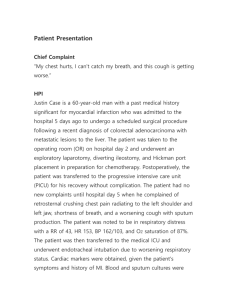
Appendix 1. Individual cases included in the survey. 1. Case A GD is a 45F with a history of COPD who presented to the emergency room overnight with altered mental status and hypercapnic respiratory failure. She was unable to be managed on NIPPV and was intubated in the emergency room and transferred to the ICU. Chest x-ray was initially read as clear. At 18 hours post intubation, with a clinical concern for aspiration during intubation, she has a new infiltrate on her chest x-ray in the right lower lobe, an increase in thick sputum production, a new leukocytosis and a fever to 101 degrees F. Culture data continues to be negative. Would your institution classify this as a VAP? 2. Case B RB is a 55M admitted to the ICU with necrotizing pancreatitis secondary to chronic alcohol abuse. His course is complicated by hypoxemic respiratory failure secondary to ARDS requiring intubation. After 8 days in the ICU, the patient was weaned from the ventilator, extubated, and transferred to the general medical service. Thirty six hours post extubation, while the patient was on the medicine floor, he developed a new increase in his oxygen requirement, a right lower lobe infiltrate on chest xray, increase in sputum production, leukocytosis, and fever to 101 degrees F. Would your institution classify this as a VAP? 3. Case C CP is a 42 otherwise healthy woman was transferred from an outside hospital in multi-organ system failure in the setting of toxic shock syndrome from a skin lesion on her upper arm. At the outside hospital, she presented with a small, erythematous lesion on her arm, fever and fatigue. Blood cultures were obtained and she was started on vancomycin. Unfortunately, she rapidly worsened, developing hypotension, ARDS and renal failure and was transferred for more aggressive management. Blood cultures from the outside hospital grow pansensitive GAS and she is switched to PCN and clindamycin and begins to improve. At hour 48 in this hospital, however, she develops a new infiltrate on her chest x-ray in the right lower lobe, an increase in purulent sputum production, an increase in her FiO2 requirement and a new fever to 101 degrees F. Blood, sputum and urine cultures remain negative throughout the hospitalization. Would your institution classify this as a VAP? Appendix 1. Individual cases included in the survey. 4. Case D MR is a 67M with diabetes and known coronary artery disease presents with chest pain, shortness of breath, new ST elevations in his anterolateral leads. He is taken emergently to the cardiac catheterization lab but found to have a severe proximal left main occlusion of 95%. During the procedure, he has several runs of unstable ventricular tachycardia, during which he is shocked, and worsening hypoxia, for which he is intubated, and is stabilized with an intraaortic balloon pump. On arrival to the cardiac intensive care unit, he is noted on his chest x-ray to have bilateral lower lobe infiltrates, rales on exam, copious secretions from his ETT and a fever and leukocytosis. No microbiologic data is obtained. Would your institution classify this as a VAP? 5. Case E CS is a 20F with severe asthma poorly controlled at home who presents to the emergency room in significant respiratory distress. She fails to improve with stacked nebulizers and is intubated as she is tiring and transferred to the ICU. On her third day in the ICU, the develops a new right lower lobe infiltrate, an increase in sputum production with multiple polys on gram stain, worsening rales on exam, an increase in her FiO2 requirements, a new fever and leukocystosis. Her sputum culture grows out ESBL-resistant e. coli. Would your institution classify this as a VAP? 6. Case F AS is an 87M transferred from a nursing home with altered mental status and hypotension. In the emergency department, he is initially confused and combative but rapidly declines and becomes unresponsive. He is intubated, central venous access is obtained, fluid resuscitation is initiated and he is started on broad spectrum antibiotics. Microbiology data obtained on arrival show a urine culture with >100,000 colonies of e.coli and initial chest x-ray is clear. After 48 hours, he develops a new left lower lobe infiltrate, purulent sputum in his ETT, a fever to 100.5 and leukocytosis. ET aspirate is positive for MRSA. A BAL is performed but remains culture negative. Would your institution classify this as a VAP?