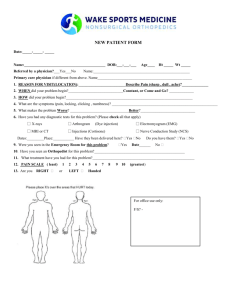
NEW PATIENT MEDICAL HISTORY
advertisement

PATIENT NAME: ______________________________________ NEW PATIENT MEDICAL HISTORY AGE: Occupation: ___________________________ ___________________________ CHIEF COMPLAINT: (WHAT IS THE REASON FOR YOUR VISIT TODAY?) ______________________________________________________________________________________________________________________________ ______________________________________________________________________________________________________________________________ HISTORY OF PRESENT ILLNESS: LOCATION: (WHERE IS THE PROBLEMLOCATED?)________________________________________________________ DURATION: (HOW LONG HAVE YOU HAD THE PROBLEM?) _______________________________________________________ CONTEXT: (HOW DID YOUR PROBLEM START?)_____________________________________________________________________ TIMING: (DO YOU HAVE PAIN?) No Yes IF YES, IS THE PAIN CONSTANT (HURTS ALL THE TIME) OR INTERMITTENT (COMES AND GOES)? QUALITY: (DESCRIBE YOUR PAIN BY CHECKING ALL THAT APPLY BELOW) ACHING BURNING THROBBING STABBING SHOOTING LOCKING CLICKING CATCHING TENDER INSTABILITY BACK PAIN LEG/FOOT NUMBNESS LEG/FOOT PINS AND NEEDLES SHARP WEAK CRAMPING SIGNS/SYMPTOMS:DESCRIBE ANY SPECIFICSIGNS OR SYMPTOMS _____________________________________________________________________________________________________________________________ _______________________________________________________________________________________________________________________________ WHAT MAKES YOUR PROBLEM BETTER? ______________________________________________________________ ICE ACTIVITY CESSATION BRACE REST NSAID’S (IBUPROFEN, NAPROXEN, CELEBREX, ETC.) WHAT MAKES YOUR PROBLEM WORSE? ______________________________________________________________ WALKINGUP/DOWN STAIRS SQUATTING PIVOTING RUNNING ALLERGIES: (LIST ALL KNOWN ALLERGIES AND REACTIONS) NO KNOWN ALLERGIES LATEX / RUBBER TAPE FOOD (LIST): IODINE CIRCLE THE NUMBER THAT BEST DESCRIBES YOUR CURRENT PAIN LEVEL . ______________________________________________________________________________________ MEDICATIONS (LIST): ______________________________________________________________________________________ OTHER: (LIST): _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ Page 1 of 7 Ver. NPHx-10- 2012 Bay Area Bone & Joint Center PATIENT NAME: ______________________________________ PAST MEDICAL & SURGICAL HISTORY PAST MEDICAL HISTORY TAKING MEDICATIONS FOR THE PROBLEM CURRENT MEDICAL PROBLEMS YES NO COMMENTS SURGICAL HISTORY COMPLICATIONS PAST SURGICAL HISTORY (ORTHOPAEDIC) YES NO COMMENTS SURGICAL HISTORY COMPLICATIONS PAST SURGICAL HISTORY FAMILY HISTORY YES NO COMMENTS FAMILY & SOCIAL HISTORY YES NO WHICH RELATIVE OR ANY PERTINENT COMMENTS Cancer Diabetes Type I: _____ Type II: ____ Heart Disease Hypertension Kidney Disease Lung Disease Mental Illness Seizures Page 2 of 7 Ver. NPHx-10- 2012 Bay Area Bone & Joint Center PATIENT NAME: ______________________________________ Stroke Thyroid Problems Tuberculosis SOCIAL HISTORY Substance Abuse NO YES | DESCRIBE: Alcohol Use: NEVER RARELY MODERATE DAILY Tobacco Use: NEVER FORMER LESS THAN 1 PACK PER DAY GREATER THAN 1 PACK PER DAY | YEARS: Smokeless Tobacco: NEVER RARELY MODERATE DAILY Caffeine Use: NEVER PREVIOUSLY CURRENTLY | TYPE / FREQUENCY: Illicit Drug Use: NEVER PREVIOUSLY CURRENTLY | TYPE / FREQUENCY: Occupation: Marital Status SINGLE MARRIED SEPARATED DIVORCED WIDOWED OTHER: Children NO YES | IF YES, HOW MANY: Cultural, Religious or Language Concerns that may affect your care: Do family and friends provide help when needed? NO YES Transportation Concerns (able to drive, etc.)?: Able to Care for Self (dressing, bathing, etc.)? NO YES If “No”, explain : Do you currently have Home Care or Hospice? NO YES If “Yes”, explain : ADVANCED DIRECTIVES & INSTRUCTIONS: (CHECK ALL THAT APPLY) I HAVE AN ADVANCE DIRECTIVE I HAVE A LIVING WILL I HAVE A DURABLE POWER OF ATTORNEY FOR HEALTHCARE ADVANCE DIRECTIVE MATERIALS WERE PROVIDED TO ME I HAVE A COPY OF MY LIVING WILL FOR THE HOSPITAL I DO NOT WANT TO BE RESUSCITATED MEDICATIONS - - WRITE ON BACK IF MORE ROOM NEEDED [PLEASE LIST ALL MEDICINES YOU ARE CURRENTLY TAKING - - INCLUDE OVER THE COUNTER, HERBAL & VITAMIN SUPPLEMENTS] MEDICATIONS AMOUNT / DOSAGE HOW OFTEN GENERAL NOTES Page 3 of 7 Ver. NPHx-10- 2012 Bay Area Bone & Joint Center PATIENT NAME: ______________________________________ PATIENT SIGNATURE: _________________________________________ DATE: _______________ TIME: __________ (OR LEGAL GUARDIAN/POA) I HAVE REVIEWED THE NEW PATIENT MEDICAL HISTORY WITH THE PATIENT / CAREGIVER AS PART OF THE INITIAL NURSING ASSESSMENT. NURSE SIGNATURE: ___________________________________________ DATE: _______________ TIME: __________ Page 4 of 7 Ver. NPHx-10- 2012 Bay Area Bone & Joint Center





![Intelitech Solutions Pvt. Limited [ A Div. of ITSPL Group ]](http://s3.studylib.net/store/data/009586270_1-33c9076cff34230b5ecd51680c993086-300x300.png)