Section Editor: Knott, Jonathan Comments to the Author: Thank
advertisement

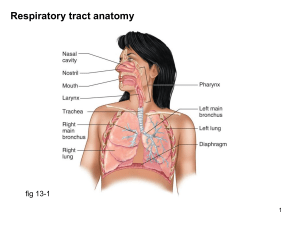
Section Editor: Knott, Jonathan Comments to the Author: Thank-you for submitting this paper to EMA for publication. The response from peer review is that whilst there is merit in this study and the data acquired, the paper as it stands is not ready for publication. Each one of the individual comments will need to be addressed (see below). All 3 reviewers (each with substantial experience in this field) found the paper difficult to read, thus I would anticipate too that our EMA readers would also struggle with this manuscript, as it stands. Please do resubmit this paper, but it will require a significant rewrite in terms of clarity, as well as needing to address all the individual points that have been raised by the reviewers. EMA woill be happy to re-evaluate that submission as soon as it is received back. Reviewers' Comments to Author: Prof. Anne-Maree Kelly, Dr. Anthony Cross, Dr. Grant Cave Reviewer: 1 Comments to the Author Thankyou for asking me to review this interesting manuscript. I like the scientific basis and approach and there are interesting results here. However, there are some factors that seriously threaten the validity/ publishability of this paper. 1. Inclusion of cardiac arrest and intubated patients [see below] 2. Inconsistencies between stated objectives, methods, outcomes of interest and results. It should possible to make a grid where each specific objective lines up with a specific method, outcome of interest and result. It is not acceptable to report results that ‘work’ if they are not defined outcomes of interest. I would strongly suggest: 1. Re-analysis, but excluding cardiac arrest and intubated patients. 2. Better definition of the outcomes of interest, and reporting against these. 3. Attention to overall consistency as described above. This means reporting against all stated outcomes of interest, not just those that have significant or interesting results. General comments: There are minor grammatical issues throughout the manuscript. Specific comments: 1. Abstract: The usual format is Aim/ objective, methods, results and conclusion. The Objective can include a brief statement regarding background or relevance. As presented, some of the material in Objective belongs in Methods. I would like a bit more detail in methods. Eg convenience sample? data were collected and from where? Define outcomes of interest. What State how analyses were performed. There appears to be a training and validation set, but this is not well described. In Results, I prefer the term ‘defined outcomes’ rather than ‘worse outcomes’, even though this may be semantic. There should be a p value related to the AUC comparison. I would like 95% CI around the reported sensitivity and the inclusion of specificity. 2. Introduction Page 4, last paragraph, line 2. There are a lot of brackets here that make readability difficult. This should be stated more clearly in words / prose without resorting to brackets. VD/VT ratio should be defined again. The Introduction is too long and most of it belongs in the Discussion. I would prefer the abstract to concentrate on why is this area of study important, what is the current state of knowledge and where are the gaps followed by a statement of your aim. Page 5, para 1, 4th last line: do you mean physiological or alveolar dead space rather than anatomical? 3. Methods: • Was this a consecutive or convenience sample? • Who decided SOB was the primary reason for ABG? Were they blinded to the study hypothesis? • Were treated doctors blinded to the CO2 gap? • The outcomes could be better defined. At what point after ED attendance was outcome defined. eg assisted anytime during admission a defined outcome, or just within 24 hours or just within ED? Same for death. I would like more justification for the admission to CCU/HDU/ICU endpoints. These are ‘softer’ and most subject to local practice differences. • I would have preferred hard outcomes [death and assisted ventilation within eg 24 hours] as the primary analysis and with the softer endpoints included as a secondary analysis. 4. Results: With an ED mortality of 4% and an assisted ventilation rate of 30%, this is clearly a very high risk SOB cohort rather than a broad SOB cohort. Is this due to local practices re use/ non-use of ABG? This should be addressed in the discussion section. I note that a significant proportion of your sample were in cardiac or respiratory arrest. This is a serious threat to your findings as most people would NOT consider this to be ‘shortness of breath’. Your results compare performance of CO2 GAP, a-A gradient, VD/VT but you do not describe this in your methods. This should be listed as an outcome of interest. C statistics [AUC] numbers with 95% CI are required for each comparison, along with p value for comparison of AUCs. Looking at the ROC curves, there is not a statistically significant difference between CO2 gap, CO2 gradient and VD/VT. This should be reported in the text, preferably with p values for the comparison. Suggested diagnostic cut-offs are chosen from the training set and this should be described in the body of the paper. These cut-offs are then tested on the validation set and performance reported. Table 1 is not needed, but I would like a table summarising demographics, clinical features [RR, BP, pulse, O2 sat] and diagnosis in training and validation sets. This would also replace table 2. In methods you say you will analyse against a composite outcome [assisted ventilation, ICU admission, death] and then in results you report a different analysis. You need to be consistent. Inclusion of ventilated patients also challenges your findings as one of the outcomes was need for assisted ventilation. I would have excluded this group. Discussion See comments above in Introduction. Reviewer: 2 Comments to the Author P5 line 20: glossary not clearly set out - suggest tabulate No definition for PETCO2 A new abbreviation (AAG) for A-a gradient is really not needed or helpful. P6 line28: should be "when cardiovascular and metabolic parameters are stable" p6 line30: "the (a-ET) PCO2 (CO2 GAP)" what is this? Is this a typesetting error? p7 line27: correct bracket position p8 line16-18: correct sentence construction P9: Equipment - 2 devices to measure ABG's and 3 to measure ETCO2 leads to concern that any findings are influenced by difference in device measurement of CO2 p11 line29: change "and onto" to "or" P12 line25: Age and gender are the only baseline demographics given. How "sick" were the patients (in terms of vital signs, ABG's or APACHE etc)? p17 line 13: given the aim of the study is to "predict need for assisted ventilation" you cannot include 27 intubated patients - the analysis should be repeated with those patients excluded. Reviewer: 3 Comments to the Author The authors present the perfomance of a relatively novel marker of the function of the cardiorespiratory axis, the CO2 gap, as a predictor of the need for assisted ventilation and mortality. Based on the initial and subsequent validation datasets at a CO2 gap of 10.5% had 100% sensitivity with acceptable specificity. This is a methodologically sound and intellectually stimulating paper. The dataset could make a valuable contribution to the literature, which could potentially translate into clinical practice. My main concern is that, as presented, the paper leans towards increased alveolar dead space secondary to reduced cardiac output as being the main cause of increased CO2 gap. This will be the case for the trauma cohort in the cited paper, but is less likely to be so for all of those in this study. As I am sure the authors are aware, in settings of reduced ventilation with normal perfusion, less ventilated alveoli contribute proportionately less and later in the expiratory phase to the expired gas flow - this being the explanation for the capnography "ramping" seen in asthma and COPD exacerbations. Inspiration begins before equilibration of these less ventilated alveolar units - thus it will give rise to a CO2 gap. In these settings A-a gradient is a less important variable, and clinical decisions on assisted ventilation are often based on arterial pCO2 along with clinical assessment. For me, in this subgroup (asthma, CAL and possibly pulmonary oedema) the performance of CO2 gap vs PaCO2 to predict assisted ventilation and mortality would be of particular interest. Minor points: I have had a moderate amount of statistical education but I do not understand the power sentence in the methods at all. This needs to be fixed up. Suggest get advice if you can not express this coherently. What were the characteristics of the 275 potentially enrollable but not included - were there any systematic differences that could have led to a biased study? I think the first paragraph of the discussion is the place to make your point rather than build towards an argument - I'd restate the main results with some expansion on potential application. p10, line 32 "the overall mortality was 17" needs to be fixed.