Topics 11-13 Genetic & Molecular Basis for Variation in Cancer
advertisement

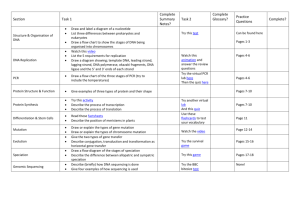
Topic 11-13: Genetic & Molecular Basis for Variation in Cancer Organisation of Eukaryotic Genome Genome: The entire set of genetic material for all the proteins and RNA that the organism will ever synthesise to direct the development and maintenance of that organism. *DNA present in a haploid set* 1. Genes are carried on chromosomes, the vehicles of inheritance. Each gene resides in a gene locus. 2. The majority of eukaryotic genes are distributed among a species-specific number of linear chromosomes. 3. Every eukaryotic cell has a complete copy of the nuclear genome. A eukaryotic cell with a hybrid genome or a complete genome comprises of a haploid set of linear chromosomes, mitochondrial genome and chloroplast genome 4. The human genome is distributed over 22 pairs of different autosomes and one of the two sex chromosomes X/Y. 5. In general, more complex organisms tend to have larger genome sizes; there is a correlation between an organism’s genome size and its apparent biological complexity because more genes and gene products are required to direct the development and maintenance of more complex organisms. 6. Generally, gene size is also larger in more complex organisms due to the increase in the proportion of regulatory sequences needed for more complex control of gene expression. 7. However, there is no correlation between biological complexity and number of genes in organisms 8. Genome size is not necessarily proportional to number of genes in the genome 9. Prokaryotic genomes have much higher gene densities than that of eukaryotes 10. More complex eukaryotes generally have lower gene density than lower eukaryotes; decreased gene density is principally attributed to the large proportion of non-coding intergenic DNA relative to genes present in their genomes 11. A eukaryotic gene includes not only the coding sequence, but also regulatory nucleotide sequences required for proper expression of the gene 12. The total number of genes represented in the human genome is ~1.5%; the remaining is allocated to non-coding DNA 13. Genome = (non-coding DNA regulatory sequences) + (Exons + introns = transcription unit) 14. Exon: I. Interrupted by introns II. Described as discontinuous coding DNA sequences 15. Intron: I. Not represented in amino acid sequence II. Number and size per gene varies III. Generally longer than exons Types of eukaryotic genes Solitary genes Features Genes that are present in only one copy per haploid set of chromosomes (eg. Chicken lysozyme gene) Topic 11-13: Genetic & Molecular Basis for Variation in Cancer Mutigene families Tandem Dispersed Multiple copies of an (almost) identical gene sequence are clustered together in tandem to form a tandem repeated array Encode for identical or nearly identical proteins or functional RNAs Gene products are usually required in heavy demand within the cell Allows for some RNAs and proteins to be produced in large quantities Consists of genes with very similar by non-identical DNA sequences Members can be located within 5-50kb of one another, forming a cluster on the same chromosome, or they may be dispersed on different chromosomes Encode for proteins with close but non-identical amino acid sequences, and which usually have related or even identical functions These proteins are closely-related and typically constitute a protein family (eg. α/β-globin of haemoglobin) Members of a gene family encode gene products that may be expressed at different times in development or in different tissues/cell types Repetitive DNA Features Sequences present in multiple copies in a genome Tandemly repeated DNA/tandem arrays consist of DNA sequences repeated multiple times and arranged adjacent to one another in a head-to-tail fashion Tandemly repeated Regular 14-500 bp genes: Satellite DNA satellite DNA Very large clusters of hundreds to thousands of kb – mostly consists of More common, major constituent of centromeric DNA relatively short Minisatellite 10-100 bp sequences repeated Sizeable clusters of 0.1 to hundreds of kb many times in More frequently located towards ends of chromosomes, tandem to form long including telomeric DNA array/ cluster in a Microsatellite Small clusters of <150 bp localised area of the Evenly distributed along the length of chromosomes genome Regulatory sequences: Regions of DNA sequence where gene regulatory proteins bind to control the rate of assembly of protein complexes required for gene expression Non-coding DNA Gene Intron Promoter Intergenic Promoterproximal centromere untranslated regions Telomere Distal control elements Topic 11-13: Genetic & Molecular Basis for Variation in Cancer Structure Function Intron DNA sequences interrupting exons, exons are thus discontinuous DNA sequences Regulatory sequences may exist Allows for alternative splicing, so that different combination of exons may give rise to different protein products 5’ Untranslated regions 5’ UTR starts at the +1 position on DNA template strand where transcription begins and ends one nucleotide before the triplet base which codes for the start codon of the coding region Contains DNA sequence which is transcribed into a ribosome binding site on mRNA for proteins which regulate the mRNA’s stability or translation 3’ Untranslated regions 3’ UTR starts after the triplet base on DNA template strand which codes for a stop codon Contains the triplet base on which codes for a stop codon Contains DNA sequences which is transcribed into a polyadenylation signal on mRNA, which is needed for termination of transcription Replicative cell senescence: the period in which a cell withdraws permanently from the cell cycle and hence stops dividing after reaching Hayflick limit when it has divided for 25 to 50 cell divisions End Replication Problem: 1. The end-replication problem occurs in linear chromosomes as the standard DNA replication machinery is incapable of completely replication all the way to the ends of a linear chromosome, leading to shortening of telomeres with each successive cell division 2. Each time a cell with linear chromosomes divide, a small section at the extreme 3’ end of the parental strand does not undergo DNA replication due to the lack of an upstream DNA polymerase that can fill in the gap generated by the removal of the final Okazaki primer. 3. Hence, the telomeres shrink by approximately 100 base pairs with every successive cell division. This represents about 16 tandem repeats of TTAGGG. 4. Without telomeres, vital genetic information that is needed to sustain a cell’s activities will be lost. Centromere Structure Consists of satellite DNA (alpha satellite DNA in humans) that consists of short, AT-rich sequences that are repeated thousands of times in tandem Centromeres are embedded in a very large stretch of centric heterochromatin: centromeric DNA in centric heterochromatin is bound by Telomere Consists of specialised nucleoprotein which are complexes composed of telomeric DNA bound by specific proteins Telomeric DNA consists of long stretches of hundreds to thousands of tandem repeats of a short nucleotide sequence with high G content Topic 11-13: Genetic & Molecular Basis for Variation in Cancer Function specialised nucleosomes containing a centromere-specific histone and other centromere-specific proteins that compact the nucleosomes into dense arrangements Folding of DNA into these specialised nucleosomes facilitates the assembly of other centromere-binding proteins to form the kinetochore that associates the centromere to the mitotic spindle 1. Sister chromatid adhesion: centromere is the region of a linear chromosome where the 2 sister chromatids join 2. Kinetochore formation: centromere is the site of assembly of the kinetochore that attaches to the microtubules of the mitotic/meiotic spindle. The sister chromatids are in turn joined via the centromere to the spindle microtubules. 3. Proper chromosome segregation: centromeres are essential for the correct segregation of daughter chromosomes after DNA replication, so that each copy goes to each of the 2 daughter cell during cell division. The presence of only one centromere on each chromosome is critical so that each kinetochore binds to kinetochore spindle fibres and is pulled towards one pole of the cell during cell division. In absence of a centromere, the chromosomes will segregate randomly, leading to loss of duplication of chromosomes in daughter cells Contains hundreds to as many as 2000 tandem repeats of the sequence 5’ – TTAGGG – 3’ 3’ end of the G-rich strand extends 12 to 16 nucleotides beyond the 4’ end of the complementary C-rich strand, forming a 3’ single-stranded overhang, which folds back on itself to form a hairpin loop called telomere loop (tloop) 1. Protective function: the t-loop forms a cap with telomere-specific proteins that protect the 5’ ends and 3’ overhangs of linear chromosomes from degradation by cellular exonucleases. The unique structure also protects it from being recognised by bell’s repair machinery as a damaged DNA molecule. 2. Maintaining stability: it confers stability to linear chromosomes as the tloops prevent the chromosome tips from fusing spontaneously 3. preventing loos of genes: telomeres protect organism’s genes from being eroded as the linear chromosome end shortens with each successive round of DNA replication due to the endreplication problem, ensuring DNA replication can occur without loss of important coding sequences 4. regulating replicative cell senescence: after the telomeres shorten to a critical length, the cell reaches Hayflick’s limit and enters a period of replicative cell senescence Action of Telomerase Telomerase does not prevent the end replication problem; it does not stop the shortening of chromosomal ends during replication It only lengthens and thereby maintains, the chromosomal ends after the end replication problem has occurred Generally found in stem cells, diploid germline cells and cancer cells A ribonucleoprotein (protein-RNA) complex that is made up of: RNA sequence template 3’ AAUCCC 5’ that is complementary to the telomere repeat sequence 5’ TTAGGG 3’ & Telomere Reverse Transcriptase (TERT), a reverse transcriptase enzyme that provides catalytic action whereby DNA is synthesised from an RNA template Topic 11-13: Genetic & Molecular Basis for Variation in Cancer telomerase RNA binds complementarily to the 3' overhang of the parental DNA strand telomerase extends the 3' overhang of the parental DNA strand in the 5' to 3' direction by adding sequence repeats of 5' TTAGGG 3' via complementary base-pairing by lengthening the 3' overhang, the synthesis of the shorter daughter strand can be extended during the next round of DNA replication, resulting in a longer telomere the action of telomerase thus helps maintain the number of repeats at the telomerase, delaying the senescence of cells and enabling them to proliferate indefintely 1. Telomerase enzyme recognises and binds to the G-rich telomere sequence at the 3’ overhang on the parental strand. The 3’ nucleotides are base paired to the 5’ UAA 3’ sequence in the RNA template of the telomerase. 2. Through its reverse transcriptase activity, telomerase adds nucleotides to the 3’ end of the overhang using the bound RNA as template, thereby extending the 3’ end of the parental strand. The sequence 5’ GGGTTA 3’ is added one nucleotide at a time. 3. The telomerase is translocated to the end of the extended overhang. The result is that the telomere is extended in a 5’ to 3’ direction, over repeated cycles of elongation and translocation. 4. Replication of the incomplete lagging daughter strand is completed by using these extensions as a template for synthesis of the complementary strand by DNA polymerase, leaving a 3’ overhang Topic 11-13: Genetic & Molecular Basis for Variation in Cancer Gene and Chromosomal Mutations Gene Nucleotide (point) substitution mutations Chromosomal aberrations Nucleotide insertion/deletion In multiples of 3 Not in multiples of 3 Nonsense mutation Missense mutation Frameshift Mutation: Extensive missense mutation Neutral mutation Silent mutation Changes in Changes in chromosome number chromosomal Aneuploidy Euploidy eg. polyploidy structure Deletion Lose/ gain one or Autoploidy more chromosomes (extra set from same species) Duplication Inversion Alloploidy (extra set from different species) Translocation Gene mutation: involves chemical changes that affect the DNA sequence of just one gene; an alteration to an organism’s characteristics that is inherited, due to a change in the genetic material of a cell, and it can destroy an organism if it occurs in a vital position in the DNA sequence. Sickle cell Anaemia Involves a mutation in the β-globin gene, which encodes one of the polypeptide subunits that make up haemoglobin. Genetic and molecular basis: Single-base substitution of a thymine for an adenine at one position in the haemoglobin gene which results in a missense mutation Sixth amino acid residue changed from a glutamate (hydrophilic) to a valine (hydrophobic) Specific 3D conformation and function of the protein is altered The substitution creates a hydrophobic spot on the outside of the protein structure that sticks to the hydrophobic region of an adjacent β chain Mutant haemoglobin subunits tend to stick to one another when the oxygen concentration is low, particularly in capillaries and veins The aggregated proteins form fibre-like structures within the red blood cells At high oxygen concentration, haemoglobin resumes globular haemoglobin structure Physiological effects: Fibre-like structures cause the rbc cells to lose their normal morphology and become sickle-shaped Sickle-shaped rbc are less able to move through capillaries and can block blood flow, resulting in severe pain and cell death of surrounding tissue due to shortage in oxygen Sickled rbc are also fragile and easily destroyed, further decreasing the oxygen carrying capacity of blood Topic 11-13: Genetic & Molecular Basis for Variation in Cancer Causes of Gene mutations Spontaneous Mutations Mutations that occur naturally; may be the result of errors that occur during DNA replication, recombination or repair DNA replication and repair DNA slippage DNA polymerase sometimes insert the wrong nucleotide or Daughter or parental DNA too many or too few nucleotides into DNA sequence strand slips during DNA replication followed by folding Some mistakes are corrected immediately during back of the strand due to replication through proofreading, and some are corrected transient dissociation and after replication in mismatch repair misaligned reannealing During proofreading, DNA polymerase enzymes recognise Hence, there is a mispairing mistakes and replace the incorrectly inserted nucleotide between the daughter DNA so that replication can continue strand and the parental After replication, mismatch repair reduces the final error template strand rate even further as incorrectly paired nucleotides cause This causes parts of the DNA deformaties in the secondary structure of the final DNA which are folded back to be molecule copied more than once During mismatch repair, enzymes recognise and fix these deformities by removing the incorrectly paired nucleotide If it corresponds to a gene, it will result in gene duplication and replacing it with the correct nucleotide Some errors fail to be recognised and are passed down from one cellular generation to the next Induced Mutation Physical agents Chemical agents X-rays Results in the production Base Molecular structures that are similar to the analogues of free radicals of water bases normally found in DNA may be which are chemically incorporated into DNA in place of the reactive normal bases during DNA replication, hence producing base substitutions Free radicals interact with BaseDNA to produce double Modify the chemical structure and stranded breaks leading to modifying properties of bases leads to mispairing agents chromosomal during DNA replication and hence base rearrangements and substitution deletions Transfer alkyl groups to bases, modifying their chemical structure UV-rays Absorbed by bases of DNA Intercalat- Flat molecules with multiple ring ing agents structures insert themselves (intercalate) This may result in the btw adjacent bases in one or both strands production of a covalent of the DNA helix attachment btw adjacent pyrimidines in one strand, Leads to insertions or deletions during usually thymine dimmers DNA synthesis and hence frameshift mutations Or bp substitutions, insertions and deletions These can block transcription and DNA replication and are lethal if not repaired Topic 11-13: Genetic & Molecular Basis for Variation in Cancer Molecular Basis of Cancer Ten Hallmarks of Cancer 1. Genome instability & Increased rate of accumulation of mutations mutation Instability occurring at the chromosomal level due to accelerated rate of chromosomal mutations Results in gains or losses of whole chromosomes as well as alterations to chromosome structure eg. Inversions, deletions, duplication, translocations of larger chromosomal segments Instability occurring at the gene level due to faulty repair pathways, resulting in single nucleotide substitutions, insertions and deletions 2. Sustaining Tumour cells are able to proliferate without the presence of proliferative signalling extracellular growth factors, unlike normal cells 3. Evading growth In normal tissue, stability of cell numbers is maintained by a host of suppressors signals and factors inhibiting cell proliferation and differentiation In cancer cells, mutations in genes critical for cell cycle control render the cells insensitive/non-sensitive to the growth-inhibitory signals Results in: o Loss of anchorage dependence (anchorage-independence growth) o Lack of contact inhibition and density-density inhibition o Tumour cells continue diving after contact with neighbouring cells, growing over adjacent cells in disordered, multilayered patterns 4. Resisting cell death By evading apoptosis, malignant cells will generally live for an by apoptosis indefinite number of cell divisions, provided the right nutrients and growth factors are present 5. Enabling replicative An uncoupling of a cell’s growth programme for signals in its immortality environment, leading to excessive cell division is not sufficient for the formation of cancer For a tumour cell population to expand, there needs to be an additional disruption to the cell replication limit Cancer cells express the enzyme telomerase, that adds telomere repeats sequences to the 3’ ends of DNA, thus escaping Hayflick’s limit, maintain telomere lengths and develop unlimited replicative potential Enabling them to divide indefinitely, gaining “immortality” 6. Deregulating cellular Tumour cells adjust their energy metabolism to consume energetics abnormally large amounts of glucose to provide ATP to proliferate uncontrollably Tumour cells also increase the expression of glucose transporters to ensure an increased uptake of glucose molecules 7. Inducing angiogenesis Angiogenesis (vascularisation): the process by which new blood vessels are formed (not an inherent property of most cells in small, localised tumours) To develop into larger, potentially metastatic tumours, a growing tumour stimulates the formation of new blood vessels that allow for Topic 11-13: Genetic & Molecular Basis for Variation in Cancer 8. Activating invasion & metastasis 9. Avoiding immune destruction 10. Tumour-promoting inflammation Characteristics Nuclear size N:C ratio Nuclear shape an increased blood flow to the tumour, hence supplying nutrients and oxygen and removing toxic waste products Tumour cells release angiogenesis-activating proteins eg. Vascular endothelial growth factor and fibroblast growth factor that attract endothelial cells and promote their proliferation, to stimulate the formation of new blood vessels Metastasis: a process where the primary tumours cells invade local tissues and blood vessels, and establish secondary tumours called metastases at distant sites Ability to metastasise marks its transformation to a malignant tumour Steps: o Cancer cells invade surrounding tissues and penetrate through the walls of lymphatic and blood vessel, thereby gaining access to the bloodstream o Cancer cells are transported by the circulatory system throughout the body o Cancer cells leave the bloodstream and enter particular organs, where they establish new secondary tumours at distant sites from the primary tumour A small percentage can evade immune destruction by disabling components of the immune system that have been dispatched to eliminate them When tumour cells swell and lyse, they release cellular contents to the extracellular environment, which release proinflammatory signals to attract inflammatory cells Inflammatory cells may be tumour promoting as they may: o Release growth factors, indirectly inducing tumour growth o Trigger angiogenesis to aid in tumour growth o Release protein factors that limit cellular death o Release enzymes to facilitate angiogenesis, invasion and metastasis Benign tumour Small and uniform in all cells Low Regular shape that does not vary between cells Usually none or just one Malignant tumour Large and usually vary between cells High Irregular shapes (pleomorphic) that vary between cells Nucleolus Prominent, large and usually >1 to number signify extensive protein synthesis Nucleolus shape Usually round Irregular shapes Rate of mitosis Low and few as benign tumour cells High as malignant tumour cells divide divide less frequently than malignant rapidly tumour cells Differentiation Well-differentiated, resembles Poorly differentiated and does not parental cells. They will still have resemble parental cells. Malignant cells most of the structural features of the may display varying stages of cells from which they originated differentiation as de-differentiation may Topic 11-13: Genetic & Molecular Basis for Variation in Cancer Tumour boundary Treatment Well-defined. Tumour cells remain clustered together in a single mass in a localised region. They grow slowly, with a well-defined perimeter and may be surrounded by a layer of connective tissue Complete cure can usually be achieved by removing the mass surgically have occurred Poorly-defined. Tumour cells may or may not cluster together, as they have acquired the ability to invade surrounding tissues and may form secondary tumours, called metastases, at distant sites in body Systemic treatment like radiation or chemotherapy is required in conjunction with surgery to ensure complete eradication of all tumour cells Causative factors of Cancer: 1. Lifestyle & Diet a. Cigarette and tobacco smoking: polycylic aromatic hydrocarbon (PAHs) bind to DNA of cells to form a physical complex known as adduct, causing DNA damage b. Exposure to carcinogens: charred meat containing heterocyclic amines (HCAs) and PAHs 2. Radiation Exposure a. Ionising radiation: form OH radicals in water b. DNA damaging UVB rays: form Thymine dimers 3. Age: accumulation of mutations 4. Genetic Predisposition: inherited mutant cancer-critical gene 5. Loss of Immunity: loss of T cells to destroy abnormal cells 6. Viral Infections: transforming viruses e.g. Human Papillomavirus (HPV) may lead to cervical cancer Oncogene: a gene that encodes for proteins promoting the loss of growth control and the conversion of a cell to a malignant state. Cell-cycle Checkpoints: critical control points where stop and go-ahead signals can regulate the cycle. Help ensure the orderly progression of the cell cycle. Proto-oncogenes A family of genes that usually encode gene products promoting normal cell growth. Function Growth factors: external signals that stimulate cells to divide Growth factor receptors: membrane proteins that find to GFs Protein kinases: enzymes that modify other proteins by chemically adding phosphate groups to them. The addition of a phosphate group usually results in the activation of a protein Inhibitors of apoptosis: proteins that inhibit the process of apoptosis and hence result in a reduced rate of cell death Transcriptional factors: proteins that bind to DNA to control the rate of transcription Topic 11-13: Genetic & Molecular Basis for Variation in Cancer Gain-in-function mutation Much less common than loss-of-function mutations Confer an abnormal new or enhanced activity of a protein Acts in a dominant manner Mutation of either copy of a proto-oncogene to an oncogene is sufficient to cause abnormal cell proliferation Causes genes to gain function, such as being over-expressed, or to encode for a hyperactive protein Ras Mutation Normal: when activated, relays signals from a growth factor receptor to a gene series of protein kinases known as the phosphorylation cascade Last protein kinase of the signal transduction pathway activates transcription of genes encoding proteins stimulating the cell cycle Activation of ras signalling causes cell proliferation Mutated: changes in the 3D conformation of the ras protein, causeing GTP to remain donded to the ras protein as a ras-GTP complex and thus stay in a constant “active” state, even in absence of growth factor Results in an increase in cell signalling, transcription and consequently stimulates the cell cycle Effects Quantitative change: tumour formation is induced by an increase in the absolute number of normal ras protein or by its production in inappropriate cell types Causes: Translocation or transposition - gene moved to new locus, under new controls Gene amplification: multiple copies of the gene Point mutation within a control element: up regulation of transcription Qualitative change: conversion of proto-oncogene via changes in the nucleotide sequence which are responsible for the ras protein becoming hyperactive Causes: point mutation within the gene – hyperactive or degradation-resistant protein Tumour Suppressor Genes (tsg) A family of normal genes that code for proteins to prevent inappropriate cell cycle progression by suppressing cell growth and proliferation. The loss of such proteins allows a cell to grow and divide in an uncontrolled fashion. Function Repression of genes that are essential for the continuation of the cell cycle Take part in cell-signalling pathways to inhibit the cell cycle Halt cell division if DNA is damaged Trigger DNA repair mechanisms, preventing cells from accumulating DNA damage Initiate apoptosis if DNA damage cannot be repaired Maintain cell adhesion Loss-of-function mutation Defined as one that results in reduced or abolished protein function If only one copy is lost, cell cycle activity remains normal, as the other copy of the gene is still produces the normal gene product Both copies of tsg must be mutated so that no functional gene product can be produced Act in a recessive manner p53 Mutation Normal: commonly known as “Guardian of the Genome” A transcription factor that bind to DNA to trigger transcription of genes involved in cell cycle inhibition Topic 11-13: Genetic & Molecular Basis for Variation in Cancer Activated protein binds to specific DNA control elements and promotes transcription for the relevant genes eg. P21 gene, whose proteins stop the cell cycle by binding to proteins that are involved in cell cycle progression eg. Cyclin-dependent kinases Ensures that damaged DNA is not replicated and gives time for the cell to repair the DNA damage Concurrently, p53 protein also stimulates DNA repair mechanisms to rectify the damage If damage is irreparable, p53 activate suicide genes to produce proteins that initiate apoptosis Mutant cell becomes able to proliferate uncontrollably and evade apoptosis Genetic instability, characterised by accumulation of further cancerpromoting mutation due to loss of ability to repair DNA Quantitative change: tumour formation is induced by a decrease in the absolute number of p53 proteins Qualitative change: tumour formation is induced by production of inactivated, non-functional p53 proteins Consequences Angiogenesis formation of new blood vessles Accumulation of mutations Tumourigenesis: Activation of telomerase Multi-step model of cancer progression Metastasis acquiring the capacity to invade tissues Development of a malignant tumour Multi-step process, characterised by a progression of permanent alterations in a single cell lineage Tumour cells are clonal Selection of tumour cells that proliferate more aggressively Accumulation of Mutations A single mutation is not enough to convert a healthy cell into a cancer cell Genesis of cancer typically requires several independent mutations in cancer-critical genes in the lineage of a single cell including both the activation of proto-oncogenes to oncogenes and inactivation of tumour suppressor genes Render the cells increasingly less responsive to the body’s normal regulatory machinery and better able to invade normal tissues Case Study - Familial Adenomatous Polyposis (FAP) All required mutations (at 2 tumour suppressor gene mutations and one oncogene) must occur in a single cell lineage in order for the cancer to develop. Topic 11-13: Genetic & Molecular Basis for Variation in Cancer 1. Loss of tsg APC 8. A malignant carcinoma develops 2. A polyp forms on the colon wall 7. Loss of tsg p53 3. Activation of ras gene 6. A class III benign adenoma grows 4. A class II benign adenoma grows 5. Loss of tsg DCC 9. other changes; loss of antimetastasis gene Mutation 1: tsg APC gene (controls proliferation, maturation, cell-tocell contact and growth inhibition) Individuals inherit one mutant copy of APC (adenomatous 10. cancer polyposis coli) gene located on metastasises chromosome 5 The presence of a heterozygous APC mutation causes the epithelial cells of the colon to partially escape cell cycle control, and the cell divides to form a small cluster of cells called a polyp/ adenoma In most cases, the 2nd APC allele becomes mutant in a later stage of cancer development Mutation 2: ras gene (proto-oncogene – stimulates cell growth and division by transmitting growth signals from the cell surface to the nucleus) Gain-of-function mutation of the ras proto-oncogene results in it becoming a ras oncogene, producing a hyperactive ras protein Results in the ras protein being permanently activated leading to continual signalling of the cell cycle to proceed into cell division This allows an escape of the cell cycle control and epithelial cells divide uncontrollably Combined APC ad ras gene mutations trigger the development of intermediate (class II) adenomas These adenomas have defects in normal cell differentiation and will grow in culture, in absence of contact with other cells and hence are transformed Mutation 3: tsg DCC gene (involved in cell adhesion and differentiation) Loss of function of both alleles of the DCC gene Result in formation of late stage (class III) adenomas with a number of finger-like outgrowths called villi Mutation 4: tsg p53 gene (arrests cell cycle in response to DNA damage) In order for late adenomas to progress to cancerous adenomas, cells need to lose both functional copies of p53 genes Results in high mutation rates throughout the genome and loss of cell proliferation control Accumulation of mutations in an unknown number of genes associated with metastasis leads to malignancy