Facilitator - Activity 3 - NHS Education for Scotland
advertisement

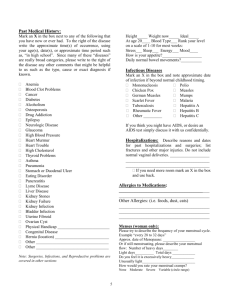
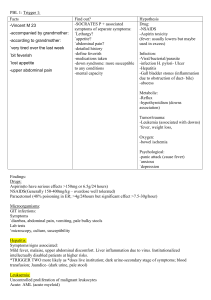
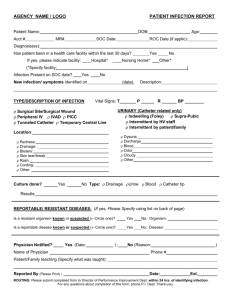
Activity 3-Giving Results-Facilitators Copy Case 1 John is a 24 year old patient in your practice. He injects heroin 3 or 4 times per day, on most days. He was tested for BBVs using DBS as part of your work up whilst referring him to the local drug service. Currently he is homeless and spends nights on the floors of various friends. There are some nights where he sleeps rough. He has a partner who lives with her parents. He occasionally sells sex to fund his drug use. Result HCV antibody positive HCV PCR positive HIV antibody test negative Hep B core antibody positive Hep B surface antigen negative What do his results show? What will you say to John about his test results? What else would you want to know from him? Does he require any further tests? Facilitators Notes Results show that John has active Hepatitis C infection and that he has had Hepatitis B infection but does not have evidence of current infection on this blood test, nor does he have evidence of HIV on this blood test. However he is at very high risk of BBV infection due to ongoing injecting behaviour and sexual risk so he will be in the window period for HIV infection and will require repeat testing. You will want to know more about his injecting behaviour especially sharing of equipment and where he obtains supplies for injecting. Homeless people are at higher risk of injecting and sharing because they cannot store equipment safely and reliably. 1 He needs to be told that he has active Hepatitis C infection currently and that he has evidence of Hepatitis B infection in the past. It is likely that this infection is from his injecting drug use BUT you need to know more about his sexual activity – unprotected intercourse, especially anal intercourse, is a risk for Hepatitis C and Hepatitis A infection. He should be told that there is treatment for Hepatitis C which is potentially curative – that he needs specialist referral to assess his infection (genotype) and how his liver is. You need to ask a sexual history including his sexual activities with his sex work partners and with his female partner. He sounds as if he is at risk of STI and may require testing for other STI (syphyllis, gonorrhoea, chlamydia) – as he is MSM this may be best done at GUM (requires rectal and pharyngeal swabs) 2 What do you feel are the main issues for John in relation to blood born virus infections at the moment? What other help could you offer him? Who else might you involve? Facilitators Notes Main issues are probably around his chaotic drug use and poor social situation. Although these should not prevent referral for assessment of his Hep C infection they are likely to affect his chances of attending the clinic and certainly his ability to adhere to treatment. Addressing these issues as early as possible will help to improve his chances of successfully completing treatment. They also are putting him at very high risk of further infection with BBV – superinfection with anther strain of Hep C or with HIV. As well as referring to the Hepatitis C clinic (ASK PEOPLE WHO THEIR LOCAL CLINICS ARE) – he should be referred in for treatment of his drug problem urgently. A social work referral, especially to a specialist drug team, could be very useful to help with his housing and benefits – as Interferon treatment needs to kept in the fridge, stable housing is very important. Support may be available more readily in a specialist GP practice for the homeless where they will have attached drug workers, CPN, social work and BBV workers – but all of this should be available at specialist drugs agency, THESE OTHER REFERRALS SHOULD NOT DELAY REFERRAL TO THE HEP C CLINIC – but letting everyone know about concurrent referrals is helpful. Other agencies that could help are local Drugs agencies to help engage with drug treatment and also access to IEP and prevention advice. Hep C specialist voluntary organizations who can offer information and sometimes practical support in getting to appointments. GP unlikely to want to initiate treatment for his drug misuse but can refer and remain in touch for support if he is awaiting appointment to be seen. Can offer him prevention advice (see below) and also offer 3 support with telling friends and family –especially his partner who is going to need BBV testing for HIV, Hep B and Hep C (sexual risk – need to ask if she injects and shares too) 4 What prevention advice would you give John at this stage? Facilitators Notes Clearly he needs advice on safer injecting and directed to local IEP site, Also advice on safer ways of using drugs – smoking or UYB – and the referral to drug treatment asap. Safer injecting advice includes no sharing of any drug using paraphernalia, possibly advice on cleaning injecting equipment if he is not able to access new equipment. He needs advice on safer sex, consistent condom use and access to free condoms He should be offered Hep A immunization – as he is already immune to Hepatitis B. He should also have Tetanus booster if not up to date. 5 Activity 3-Giving Results Case 2 Sam is a 45 year old man who had abnormal LFTs on routine testing. An initial liver screen was carried out to investigate this which included screening for hepatitis B and C infection. He is married with two children. He was consented for the BBV tests but did not have a risk history taken before testing. Result HCV antibody positive HCV PCR (or antigen) positive Hep B core antibody negative Hep B surface antigen negative How would you discuss these results with Sam? Facilitators Notes Sam is likely to be shocked – it is good that he has been tested as his infection has been discovered but he will need a lot of support to cope with the diagnosis. Tell him the result quickly in the consultation- the tests have shown no evidence of Hepatitis B infection but have shown an active infection with Hepatitis C infection. Could ask him if he has heard of Hepatitis C infection and how it is acquired. If he has no knowledge or only partial knowledge tell him about Hepatitis C Important points are - it is a virus spread through blood to blood contact - the commonest route of spread is through injecting or snorting drugs, especially through sharing of equipment – even on one occasion 6 - - It can also be transmitted through unsterile medical treatment (especially in a high prevalence country) or tattooing/piercing or blood transfusion in the UK prior to screening it can be present in the body for many years with no symptoms or non-specific symptoms of malaise, poor concentration it infects the liver and can, after many years infection, cause liver damage and scarring. The tests already taken do not tell us how much the liver is damaged. AND MOST IMPORTANTLY IT IS TREATABLE WITH UP TO 95% CURE RATE. 7 What further information do you need from Sam at this stage and why? Does he require any further tests? Facilitators Notes After hearing about Hepatitis C ask Sam if he can identify a risk that he may be aware of that could have put him at risk. Some people cannot identify any risk – or may not want to tell you about it- and the most important thing is that the infection has been identified and he can access treatment. Recent risk eg drug use is important as he may be in the window period for Hep B infection. As he has one BBV the advice is that he should be tested for them all and that includes HIV. 8 Sam asks about treatment that is available to him – what are the main points that you would cover with him at this stage? Facilitators Notes He should be told that there is treatment for Hepatitis C which is potentially curative – that he needs specialist referral to assess his infection (genotype) and how his liver is. This will include more blood tests and scans of his liver but not usually a liver biopsy nowadays. He can be told success rate of treatment is up to 95% cure and that he could have to take treatment for 3-6 months. The treatment depends on the Genotype of the Hepatitis C virus that he has acquired and that will be determined by the tests taken at the specialist clinic. Treatment will involve the use of injectable interferon once weekly plus one or two types of oral medication depending if he has Genotype 1 or one of the other genotypes. Side-effects include malaise, flu-like symptoms, depression, skin rashes and blood problems such as anaemia, but these are all monitored and treatments for the side-effects are offered. People who start treatment manage to finish it in most cases. It will require regular monitoring and hospital attendance. 9 Sam asks what this means for his wife and family – what issues do you need to discuss with him? How could you support him with these issues? Facilitators Notes Although Hepatitis C infection has a low risk of heterosexual transmission (<5% lifetime incidence) and a very low risk of household transmission, the advice is that his wife and family should be offered testing for Hepatitis C and the other blood borne viruses. Risk of mother to child transmission is also very low. His wife may be very shocked and angry – these viruses and their routes of transmission can carry a high level of stigma. He may have to disclose drug use to her – now or in the past. It may be useful to offer to help to tell her about the diagnosis, with both of them present. You could also suggest a Hep C voluntary agency locally to help with this and the use of written materials ,eg from the British Liver Trust. They should be advised about not sharing razors, tooth brushes and clippers at home but that cups, toilet seats and cutlery are absolutely safe. How to deal with a blood spillage using gloves and bleach/Milton. Advice is that although sexual transmission is very low risk that they should practice safer sex with condoms. Kissing is fine. They should all be offered Hepatitis B immunization. 10 Activity 3-Giving Results Case 3 Precious is a 21 year old female who was born in Zimbabwe and moved to Scotland with her family. Precious was tested for BBVs when she came to the practice saying her partner had been diagnosed with ‘hepatitis’ When she comes back for the result she tells you that she has had a positive pregnancy test. Results Hep B surface antigen positive Hep C antibody negative What would you say to Precious about her test results? Does she require any further tests? Facilitators Notes The tests show that she has active Hepatitis B infection but no evidence of Hepatitis C infection. Hepatitis B is a sexually transmitted infection although the most common route of transmission is from mother to child. From the information that you have it is not possible to say that she acquired her infection from her husband – she may have given it to him or they may both have acquired it separately. These tests cannot tell how long she has had the infection and do not tell us if her liver is damaged significantly. She is infectious and can spread the infection to others sexually or through blood to blood contact. Her household and sexual contacts will need tested and immunized if not infected or immune. Hepatitis B is a notifiable condition and public health department will be informed about this diagnosis even if she does not give her consent, they will contact her to ask about contact tracing. 11 A risk assessment is important to try and determine if she could be at risk Hep C infection and is in the window period. She comes from a country of high HIV prevalence and had not had an HIV taken – she should have this done asap. She needs URGENT referral to the specialist unit (ASK WHICH THEY WOULD USE) – to assess for treatment. 12 Precious asks about the risks to her baby – what will you say to her about this? Facilitators Notes Important message is that her baby is at risk of infection but that this can be prevented by treatment for the baby. . Vertical transmission (mother to infant) of infection occurs in 90% of pregnancies where the mother is HBeAg-positive and in about 10% of HBsAg-positive, HBeAg-negative mothers. All babies born to infected mothers should receive a complete course of vaccine at birth, one month and 6 months of age. Babies born to highly infectious mothers (HBeAG) should receive HBIG (preferably given within 24 hours of delivery) as well as active immunisation HBIG may be given simultaneously with vaccine but at a different site. This reduces vertical transmission by 90%. Caesarean section is not required and immunised babies can be breast fed. There is some evidence that treating the mother in the last month of pregnancy with lamivudine may further reduce the transmission rate if she is highly infectious (HBVDNA> 1.2 x 10 9 geq/ml), but this needs to be further substantiated. Hepatitis B may exacerbate after the end of pregnancy. 13 Would you refer Precious to a specialist and, if so, who? Facilitators Notes She needs URGENT referral to the viral hepatitis specialist unit (ASK WHICH THEY WOULD USE) – to assess for treatment. Her pregnancy will influence the decision to treat at this stage but should not delay referral. The decision to treat depends on pattern of disease, HBVDNA level, and presence or absence of significant necro- inflammation and hepatic fibrosis. In addition she needs a medical referral to the Obstetricians so that they are aware of her diagnosis and can ensure that she and the baby are treated to prevent vertical transmission. A helpful resource around giving results can be accessed on utube on the link below:http://m.youtube.com/watch?v=1HWQxXdHMxg 14