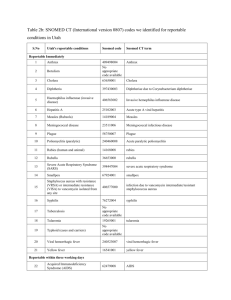
Patient Infection Report Form - Healthcare Documentation
advertisement

AGENCY NAME / LOGO PATIENT INFECTION REPORT Patient Name: Acct # DOB: MR# SOC Date: Age: ROC Date (if applic): Diagnosis(es): Has patient been in a health care facility within the last 30 days? If yes, please indicate facility: ____Hospital* Yes ____Nursing Home* No. Other* (*Specify facility: ) Infection Present on SOC date? Yes No New infection/ symptoms identified on (date). Description: ________________________________________________________________________________________ TYPE/DESCRIPTION OF INFECTION Vital Signs: T Surgical Site/Surgical Wound Peripheral IV IVAD PICC Tunneled Catheter Temporary Central Line R BP URINARY (Catheter related only) Indwelling (Foley) Supra-Pubic Intermittent by HV staff Intermittent by patient/family Location: Dysuria Discharge Blood Odor Cloudy Other Redness: Drainage: Blisters: Skin tear/break: Rash: Cording: Other: Culture done? P Yes No Type: Drainage Urine Blood Catheter tip Results: REPORTABLE/ RESISTANT DISEASES: (If yes, Please Specify using list on back of page) Is a resistant organism known or suspected (Circle one)? Yes No: Organism: Is a reportable disease known or suspected (Circle one)? Yes No: Disease: Physician Notified? No (Reason: Yes (Date: Name of Physician ); ) Phone # Patient/Family teaching (Specify what was taught): Reported By (Please Print) : Date: Ext. ROUTING: Please submit completed form to Director of Performance Improvement Dept. within 24 hrs. of identifying infection. For any questions about completion of this form, phone P.I. Dept. Thank-you. AGENCY NAME Patient Infection Report RESISTANT ORGANISMS: MRSA (Methycillin Resistant Staphylococcus Aureus) VRE (Vancomycin Resistant E. Coli) ORSA (Oxycillin Resistant Staphylococcus Aureus) OTHERS (Please specify organism on front) and Bold Type NY STATE REPORTABLE DISEASES: indicate need for phone reporting within 24 hours. (Please submit written report to Performance Improvement ASAP and we will make phone call to Dept. of Health.) Amebiasis Histoplasmosis Poliomyelitis Animal bites Hospital associated infection (s) Psittacosis Anthrax Increased incidence/outbreak Babesiosis Staph/strep in newborns Kawasaki syndrome Botulism Legionellosis Brucellosis Leprosy Camphylobacteriosis Chancroid Cholera Rabies Reye’s Syndrome Rocky Mountain Spotted Fever Rubella Leptospirosis Salmonellaosis Listeriosis Shigellosis Lyme Disease Streptococcal Infections* Cryptosporidiosis Lymphogranuloma venereum (invasive disease due to Group A Diphtheria Malaria E. Coli 0157:H7 infection Measles Syphilis Encephalitis Meningitis Tetanus beta hemolytic strep) Foodborne illness (specify agent) Aseptic Toxic Shock Syndrome Giardiasis Haemophilus Trichinosis Gonococcal infection Meningiococcal Granuloma inguinale Haemophilus influenzae (Invasive Disease) Other (specify type) Meningiococcemia Mumps Hantavirus Disease Hemolytic Uremic Syndrome Pertussis (whooping Cough) Hepatitis A Plague Hepatitis B Pneumococcal infections* Hepatitis C (invasive disease due to antibiotic Hepatitis non-A, non-B resistant streptococcus pneumoniae) Tuberculosis Tularemia Typhoid Typhus Yellow fever Yersiniosis *Report only cases with positive cultures from blood, CSF, joint, peritoneal, or pleural fluids OTHER REPORTABLE infection related diseases for Agency follow-up: C. Difficile Adult conjunctivitis E. Coli Any Strep. infection Herpes Any death due to known or suspected communicable disease Pediculosis Any hospitalization due to known or suspected communicable disease