Physiology Ch. 39 p485-494 [4-25
advertisement
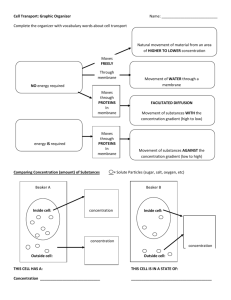
Physiology Ch. 39 p485-494 Physical Principles of Gas Exchange -After the alveoli have been filled with air, oxygen diffuses into pulmonary blood and CO2 diffuses out Molecular Basis of Gas Diffusion – kinetic motion of molecules provides energy for diffusion -Net diffusion of a gas in one direction is due to a high concentration of a gas in one chamber and low concentration at the other end. -There are more molecules at high concentration to diffuse than at low concentration, rates different Gas Pressures in a Mixture of Gases – pressure is caused by multiple impacts of gases on a surface. Pressure of gas on surface of respiratory passage and alveoli is proportional to summated force of impact of all molecules of gas striking surface at any given instant. -pressure is directly proportional to concentration of gas molecules -oxygen, nitrogen, and CO2 mixtures are found in respiratory system. -rate of diffusion of each is directly proportional to pressure caused by that gas alone (partial pressure) Pressures of Gases Dissolved in H2O and Tissues – when gas dissolved in fluid encounters a surface such as a membrane, it exerts its own partial pressure the same way as if they were in gas state. These partial pressures are called PO2, PCO2, PN2, PHe, etc… -partial pressure of gas in solution is determined by its concentration as well as solubility coefficient – some times of molecules have an affinity for water better than others, whereas some are repelled -Attracted molecules can dissolve better without excess pressure, repelled molecules build pressure in solution and develop a HIGH partial pressure: Henry’s Law = Conc. Dissolved Gas / Solubility Coefficient -CO2 is 20x as soluble as O2, so the PCO2 is 20x less than PO2 Diffusion of Gases between Gas Phase in Alveoli and Dissolved Phase in Pulmonary Blood – PP of gases in respiratory mixture push molecules into solution in the blood of alveolar capillaries -rate at which molecules bounce back and escape into alveoli is proportional to PP in blood -Net Diffusion – determined by difference between two PP -if PP in gas is greater in alveoli, as is for O2, molecules will diffuse into blood -if PP of gas is greater in blood, as is for CO2, molecules will diffuse toward gas phase in alveoli Vapor Pressure of H2O – nonhumidified air breathed in will cause water evaporation from surfaces of respiratory passage to humidify it because H2O is constantly escaping into gas phase (vapor pressure) -depends entirely on temperature of H2O -most important value to remember is VP at body temperature is 47 mm Hg at 100 degrees celcius Diffusion of Gases Through Fluids – Pressure Difference Causes Net Diffusion – overall net diffusion is the number of molecules bouncing in the forward direction MINUS molecules bouncing back, this is called the PRSSURE DIFFERENCE FOR CAUSING DIFFUSION Factors that Affect Rate of Diffusion in a Fluid – solubility, cross sectional area of fluid, distance through which gas must diffuse, molecular weight of gas, and temperature of fluid -greater CS area = greater diffusion -greater distance molecules travel = LESS diffusion -greater the velocity (related to molecular weight) the greater the diffusion -All of these factors contribute to the Diffusion Coefficient of Gas = S/root(MW) Diffusion of Gases through tissues – gases soluble in lipids and cell membranes, limiting factor is diffusion through tissue water and not membrane -therefore, diffusion through tissues and respiratory membrane is = to diffusion of gases in water Compositions of Alveolar Air and Atmospheric Air are Different -concentrations of gases in the air and in alveoli are different -alveolar air is only partially replaced by atmospheric air with each breath and oxygen is constantly being absorbed into pulmonary blood and CO2 is diffusing from blood into alveoli -dry atmospheric air is humidified before reaching alveoli Humidification of Air in Respiratory Passage – the total pressure in alveoli cannot rise above atmospheric pressure, and so the water vapor dilutes all other gases in the inspired air, meaning humidified air has less PP of gas than in atmospheric air Rate at Which Alveolar Air is Renewed by Atmospheric Air – function residual capacity is a lot higher than inspired air of each breath, therefore many breaths required to exchange most of alveolar air -1/2 of the gas is removed in 17 seconds-- if ventilation ½ of normal, it takes 34s for removal of air -it is important that alveolar air is removed SLOWLY to prevent sudden changes in gas concentration in blood, helps prevent increases and decreases in tissue oxygenation, CO2, and tissue pH Oxygen Concentration and Partial Pressure in Alveoli – the more rapidly O2 is absorbed, the lower the alveolar concentration, and the same is true conversely. Therefore controlled by: 1. Rate of absorption of O2 into blood 2. Rate of entry of new oxygen into lungs by ventilation -an extreme increase in ventilation will not increase alveolar PO2 above 149mmHg due to maximal PO2 humidification CO2 Concentration and PP in Alveoli – CO2 is being formed in body and carried to alveoli for removal. -Alveolar PCO2 increases directly in proportion to the rate of CO2 excretion -Alveolar PCO2 decreases in inverse proportion to alveolar ventilation -Therefore, concentrations of O2 and CO2 dependent on rates of absorption and excretion and amount of ventilation Expired Air is a Combination of Dead Space Air and Alveolar Air – overall composition of expired air determined by amount of air in dead space and alveolar air. -As more and alveolar air is mixed with dead space air, dead space air is washed out and only alveolar air is expired at the end of expiration -Collecting alveolar air only requires collecting the expired air at the end of a forceful expiration Diffusion of Gases Through Respiratory Membrane – 1. Respiratory Unit – also called respiratory lobule and is composed of bronchiole, alveolar ducts, atria, and alveoli. 300 mil alveoli in lungs, and they are thin, having network of capillaries around them. Flow of blood described as being a sheet. a. Gas exchange can occur at terminal portions of lungs and not just alveoli through a membrane called the respiratory or pulmonary membrane 2. Respiratory Membrane – membrane through which gas exchange occurs between the alveolus and the red blood cell. It has a number of different layers associated with it: a. Layer of fluid lining alveolus containing surfactant to reduce surface tension b. Alveolar epithelium of thin epithelial cells c. Epithelial basement membrane d. Thin interstitial space between alveolar epithelium and capillary membrane e. Capillary basement membrane that can fuse with alveolar epi. Basement membrane f. Capillary endothelial membrane -thickness is just up to 0.6um, and RBC squeezes through capillary touching walls, increasing diffusion Factors that Affect the Rate of Gas Diffusion Through the Respiratory Membrane – thickness of the membrane, surface area of the membrane, diffusion coefficient, partial pressure difference of the gas between both sides of membrane 1. Thickness of membrane can increase like in edema fluid in interstitial space of membrane and alveoli, causing gases to have to diffuse through fluid as well 2. Surface area can decrease in conditions with lobectomy or emphysema, impedes gas exchange 3. Diffusion Coefficient depends on gas’s solubility in the membrane and on the square root of its molecular weight. CO2 diffuses 20x as rapidly as O2, and O2 twice as rapidly as N2 4. Pressure Difference across the membrane is the difference of partial pressure of gas in alveoli and partial pressure of gas in pulmonary blood. Net difference is a measure of Net Tendency to move through the membrane a. If PP of gas is > in alveoli than blood, the gas moves into the blood, and conversely. Diffusing Capacity of the Respiratory Membrane – expressed in quantitative terms by membrane’s diffusing capacity, which is the volume of a gas that will diffuse through membrane each minute for a partial pressure difference of 1mmHg. DIFFUSING CAPACITY = V/min/ 1mmHg Diffusing Capacity for Oxygen – average diffusing capacity of oxygen is 21mL/min/mmHg which is equal to the rate at which resting body uses oxygen -Diffusing capacity of oxygen increases during strenuous exercise, max of 65mL/min/mmHg, three times the resting diffusing capacity. Caused by multiple factors: 1. Opening up of many dormant pulmonary capillaries or extra dilation of already open capillaries 2. Better match between ventilation of alveoli and perfusion of alveolar capillaries with blood, called the ventilation-perfusion ratio. Diffusing Capacity of CO2 – never been measured because CO2 diffuses through respiratory membrane very rapidly such that PCO2 in blood is not far from PCO2 in alveoli, but other gases show that -diffusing capacity of gases varies directly with diffusion coefficient -because CO2 has coefficient 20x that of O2, it would also have a capacity higher as well Measurement of Diffusing Capacity – PO2 diffusing capacity is more difficult to measure, so physiologists use diffusing capacity of Carbon Monoxide (CO) instead. -small CO is breathed into alveoli, and PP of CO in alveoli is measured from alveolar samples -CO pressure in blood is 0 because hemoglobin combines very rapidly with CO -Measure volume of CO absorbed and dividing by alveolar CO partial pressure gives CO diffusing capacity -Multiply CO diffusing capacity by 1.23 to get the O2 diffusing capacity Effect of Ventilation-Perfusion Ratio on Alveolar Gas Concentration – some areas of the lung normally have almost no blood flow, whereas others have excellent blood flow but no ventilation. -gas exchange at respiratory membrane is impaired, and person suffers respiratory distress -ventilation/perfusion ratio helps us understand respiratory exchange when there is imbalance between alveolar ventilation and alveolar blood flow. -Ventilation-Perfusion Ratio = Va/Q where Va is alveolar ventilation and Q is blood flow -when Va is 0 but Q still persists, Va/Q = 0 -When Va persists but Q = 0, ratio is infinity -at a ratio of 0 or infinity, no gas exchange occurs across respiratory membrane Alveolar O2 and Co2 Partial Pressures when Va/Q = 0 -if Va/Q = 0, air in alveolus is in equilibrium with blood O2 and CO2 because these gases diffuse between the blood and alveolar air Alveolar O2 and CO2 Partial Pressures when Va/Q = Infinity -when Va/Q = infinity, there is no capillary blood flow to carry O2 away or bring CO2 toward alveoli. Instead of alveolar gases coming to equilibrium with venous blood, alveolar air becomes equal to humidified inspired air -Gas exchange and alveolar PP when Va/Q is normal causes optimal O2 and CO2 exchange across respiratory membrane -There exists a PO2-PCO2 diagram for expressing Va/Q. Look at it. Concept of Physiologic Shunt when Va/Q is Below Normal – if Va/Q is below normal, inadequate ventilation to provide oxygen needed to fully oxygenate the blood in capillaries -some venous blood passing through will not get oxygenated (Shunted Blood) -Total amount of shunted blood per minute is called the physiologic shunt – -The greater the physiologic shunt, the greater amount of blood fails to be oxygenated as it passes through the lungs Concept of Physiologic Dead Space when Va/Q is Greater than Normal – if ventilation of alveoli is great but blood flow is low, there is more O2 available in alveoli that can be transported away by blood. Thus the ventilation of these alveoli is said to be wasted. -Sum of anatomical dead space in respiratory passageways and the wasted O2 is called the physiologic dead space -when physiologic dead space is great, much of work of ventilation is wasted effort because O2 doesn’t reach lungs Abnormalities of Ventilation-Perfusion Ratio – pulmonary capillary flow and ventilation are lower in upper part of lung than in lower part, but blood flow is decreased considerably more than ventilation -at top of lung, Va/Q is 2.5x greater than ideal value, causes some physiologic dead space in this area. -in contrast, bottom part of lung there is too little ventilation per blood flow, causes physiologic shunt Abnormal Va/Q in Chronic Obstructive Lung Disease – Most people who smoke for many years develop chronic obstruction, could lead to emphysema, can cause Va/Q to shift in many ways to cause physiologic shunt or physiologic dead space in many areas of the lung