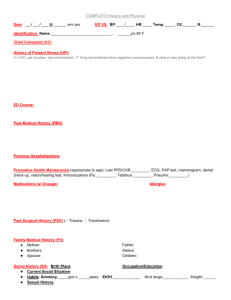
AGNP/FNP H&P Guidelines: Nursing Assessment Template
advertisement
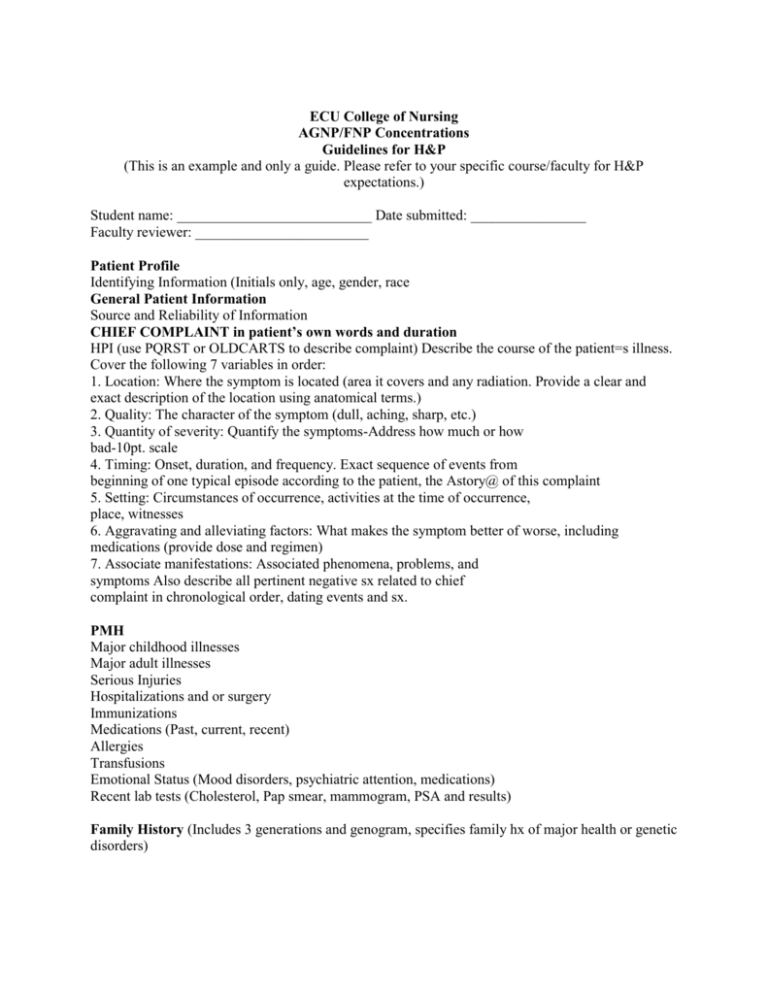
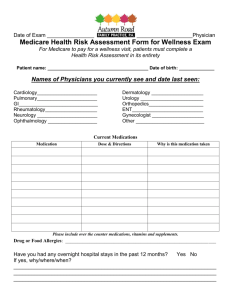
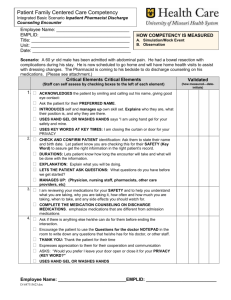
ECU College of Nursing AGNP/FNP Concentrations Guidelines for H&P (This is an example and only a guide. Please refer to your specific course/faculty for H&P expectations.) Student name: ___________________________ Date submitted: ________________ Faculty reviewer: ________________________ Patient Profile Identifying Information (Initials only, age, gender, race General Patient Information Source and Reliability of Information CHIEF COMPLAINT in patient’s own words and duration HPI (use PQRST or OLDCARTS to describe complaint) Describe the course of the patient=s illness. Cover the following 7 variables in order: 1. Location: Where the symptom is located (area it covers and any radiation. Provide a clear and exact description of the location using anatomical terms.) 2. Quality: The character of the symptom (dull, aching, sharp, etc.) 3. Quantity of severity: Quantify the symptoms-Address how much or how bad-10pt. scale 4. Timing: Onset, duration, and frequency. Exact sequence of events from beginning of one typical episode according to the patient, the Astory@ of this complaint 5. Setting: Circumstances of occurrence, activities at the time of occurrence, place, witnesses 6. Aggravating and alleviating factors: What makes the symptom better of worse, including medications (provide dose and regimen) 7. Associate manifestations: Associated phenomena, problems, and symptoms Also describe all pertinent negative sx related to chief complaint in chronological order, dating events and sx. PMH Major childhood illnesses Major adult illnesses Serious Injuries Hospitalizations and or surgery Immunizations Medications (Past, current, recent) Allergies Transfusions Emotional Status (Mood disorders, psychiatric attention, medications) Recent lab tests (Cholesterol, Pap smear, mammogram, PSA and results) Family History (Includes 3 generations and genogram, specifies family hx of major health or genetic disorders) Personal and Social History Cultural background and practices Home conditions/social situation Occupation (includes exposure to heat & cold, industrial toxins, protective devices required and used, military service) Current health Habits/risk factors (exercise, smoking, obesity/weight control, alcohol intake, recreational drugs, etc.) Exposure to chemicals, toxins, poisons, asbestos, radioactive material, caffeine) Sexual activity (Contraception, barriers, past STI’s, screening for STIs including HIV and Syphilis along with treatment) Concerns about health care Review of Systems General Constitutional Diet (Appetite, preferences, restrictions, supplements, caffeine, food diary or 24 hr recall Skin, hair and nails Head and Neck Eyes (visual acuity, blurring, double vision, use of glasses, eye drops, medications, hx trauma or family hx eye disease Ears (hearing loss, pain, discharge, tinnitus, vertigo) Nose (smell, colds, obstruction, nosebleeds, post nasal discharge, sinus pain) Throat and Mouth (Hoarseness or change in voice; freq sore throats, bleeding or swelling of the gums, recent abscesses, soreness of the tongue, ulcers, disturbances of taste) Endocrine (Thyroid enlargement or tenderness, heat or cold intolerance, unexplained weight change, polydipsia, polyuria, changes in facial or body hair, increased hat /glove size, skin striae) Males: Puberty onset, erections, emissions, testicular pain, libido, infertility Females: Menarche, regularity, duration, and amount of flow, dysmenorrheal, LMP, intermenstrual discharge or bleeding, itching, date of last Pap, age at menopause, libido, frequency of intercourse, sexual difficulties, infertility, gravidity and parity, number and duration of each pregnancy, delivery method, complications of pregnancy or postpartum period, use of contraceptives Breasts (Pain, tenderness, discharge, lumps, galactorrhea, mammograms, frequency of BSE) Chest and Lungs (Pain with respiration, dyspnea, cyanosis, wheezing, cough, sputum character/quantity, hemoptysis, night sweats, Tb exposure, last chest x-ray) Heart &Blood vessels (Chest pain or distress, precipitating causes, timing and duration, relieving factors, palpitations, dyspnea, orthopnea, edema, claudication, hypertension, previous MI, exercise tolerance, past cardiac tests) Hematologic (Anemia, bruising/bleeding tendency, thromboses, thrombophlebitis, blood disorders, transfusions) Lymphatic (Enlargement, tenderness, suppuration) GI (Appetite, digestion, food intolerance, dysphagia, heartburn, nausea, vomiting, hematemasis, bowel regularity, constipation, diarrhea, change in stool color or contents, flatulence, hemorrhoids, hepatitis, jaundice, dark urine, ulcer history, gallstones, polyps, tumor, previous studies) GU (Dysuria, flank or suprapubic pain, urgency, frequency, nocturia, hematuria, polyuria, hesitancy, dribbling, loss in force of stream, passage of stone, facial edema, stress incontinence, hernias, STD’s) Musculoskeletal (Joint stiffness, pain, restriction of motion, swelling, redness, heat, bony deformity) Neurologic (Syncope, seizures, weakness, paralysis, problems with sensation or coordination, tremors) Psychiatric (Depression, mood changes, difficulty concentrating, nervousness, tension, suicidal thoughts, irritability, sleep disturbances) Objective: Physical Examination General (age, race, sex, general appearance, Height, weight, BMI, vital signs. Mental Status (Physical appearance/behavior, LOC, response to questions Skin ( Color, uniformity, integrity, texture, temperature, turgor, hygiene, tattoos, scars, edema, moisture, excessive perspiration, unusual odor, mobility, lesions, parasites, trauma, hair, nails) Head (Size and contour, symmetry, facial features, edema, temporal arteries) Eyes (visual acuity, orbits, EOM’s, Pupils, fundiscopic) Ears (Configuration, position, alignment of auricles, otoscopic findings, hearing) Nose (External appearance, patency, discharge, crusting, flaring, turbinates, septum, sinus tenderness, swelling, smell) Throat and Mouth (Number, occlusion and condition of teeth, missing teeth, presence of dental appliances, lips, tongue, buccal/oral mucosa, floor of mouth, appearance of oropharynx, tonsils, palate, tongue symmetry/movement, soft palate, uvula, gag reflex, taste discrimination) Neck (fullness, mobility, strength, trachea, thyroid) Chest (Size and shape, AP/Transverse diam, symmetry with respiration, retractions, accessory muscles, diaphragmatic excursion) Lungs (Respiratory rate, depth, regularity, quietness/ease of respiration, symmetry and quality of tactile fremitus, quality & symmetry of percussion note, breath sounds, cough characteristics, presence of friction rub, egophony, bronchophony, whispered pectoriloquy, vocal resonance) Breasts (Size, contour, symmetry, consistency, masses, scars, thickening, retractions, dimpling, nipples, areola, discharge) Heart (PMI, rate, rhythm, thrills, heaves, lifts, S1,S2, murmurs, rubs, gallops, extra heart sounds) Blood Vessels (amplitude/symmetry pulses, jugular vein pulsations, bruits, temperature, color, hair distribution, appearance of extremities, edema, venous distention varicosities, Homan’s sign Abdomen (Shape, contour, visible pulsations, bowel sounds, palpation findings, percussion findings, liver span, CVA tenderness) Male genitalia (external genitalia, urethral discharge, pubic hair, testes, hernia/scrotal swelling) Female genitalia (external genitalia, vaginal mucosa, cervix, discharge, odor, bimanual findings, rectovaginal exam, urinary incontinence with valsalva) Anus and Rectum (Sphincter tone, hemorrhoids, fissures, rectal wall contour, tenderness, prostate size contour, consistency, stool color/consistency) Lymphatics ( lymph nodes in head, neck, clavicular, epitrochlear, axillary, inguinal areas, redness, streaks) Musculoskeletal (posture, symmetry of muscle mass, tone, strength, fasiculations, spasms, active/passive ROM, pain with movement) Neurologic (Cranial nerves, gait, balance, coordination, sensory function, superficial and DTR’s ASSESSMENT AND PLAN: You will include your actual diagnoses, numbers 1, 2, 3, etc based on priority and then detail your plan for each diagnoses. You will note the differentials that you ruled out and why you ruled them out. You will include all medications, therapeutic interventions, interprofessional referrals/other professionals that need to be involved with recommendations, advanced care planning, follow-up plan and patient/family education. Include anticipatory guidance, health promotion and health maintenance. Support your decisions with evidence-based guidelines and cite your references in correct APA format.