Heather Schultz February Case Study February 24, 2012 External
advertisement
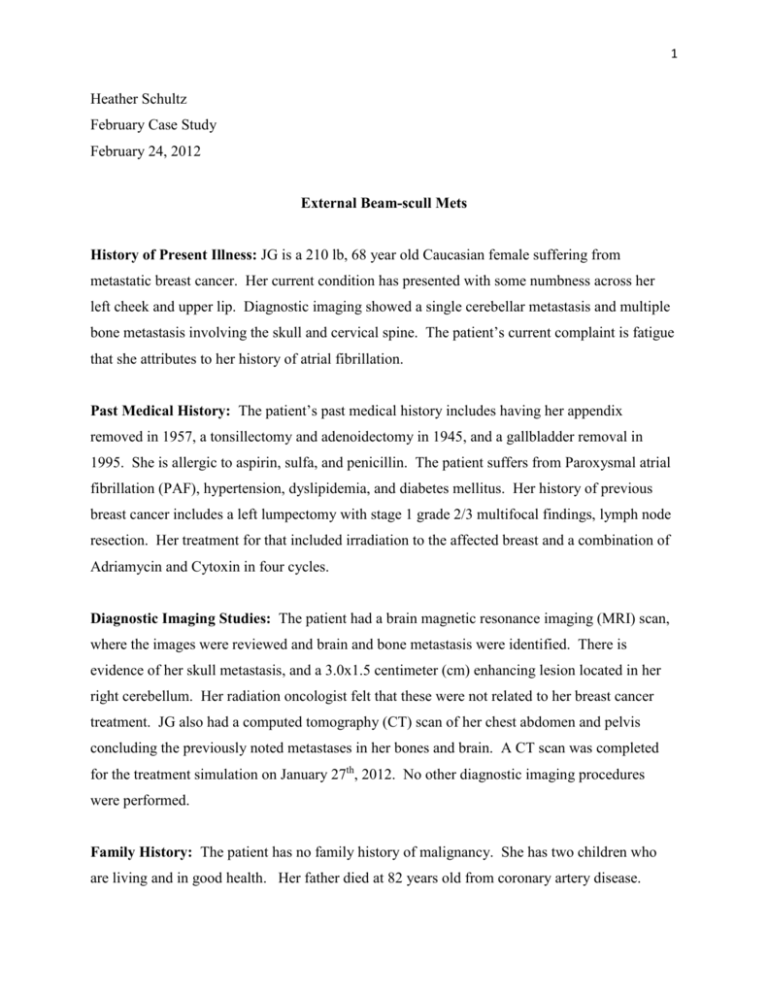
1 Heather Schultz February Case Study February 24, 2012 External Beam-scull Mets History of Present Illness: JG is a 210 lb, 68 year old Caucasian female suffering from metastatic breast cancer. Her current condition has presented with some numbness across her left cheek and upper lip. Diagnostic imaging showed a single cerebellar metastasis and multiple bone metastasis involving the skull and cervical spine. The patient’s current complaint is fatigue that she attributes to her history of atrial fibrillation. Past Medical History: The patient’s past medical history includes having her appendix removed in 1957, a tonsillectomy and adenoidectomy in 1945, and a gallbladder removal in 1995. She is allergic to aspirin, sulfa, and penicillin. The patient suffers from Paroxysmal atrial fibrillation (PAF), hypertension, dyslipidemia, and diabetes mellitus. Her history of previous breast cancer includes a left lumpectomy with stage 1 grade 2/3 multifocal findings, lymph node resection. Her treatment for that included irradiation to the affected breast and a combination of Adriamycin and Cytoxin in four cycles. Diagnostic Imaging Studies: The patient had a brain magnetic resonance imaging (MRI) scan, where the images were reviewed and brain and bone metastasis were identified. There is evidence of her skull metastasis, and a 3.0x1.5 centimeter (cm) enhancing lesion located in her right cerebellum. Her radiation oncologist felt that these were not related to her breast cancer treatment. JG also had a computed tomography (CT) scan of her chest abdomen and pelvis concluding the previously noted metastases in her bones and brain. A CT scan was completed for the treatment simulation on January 27th, 2012. No other diagnostic imaging procedures were performed. Family History: The patient has no family history of malignancy. She has two children who are living and in good health. Her father died at 82 years old from coronary artery disease. 2 Social History: The patient is married and lives in with her spouse. She has two children and five grandchildren. She is a former smoker who quit in 1988, and drinks alcohol occasionally. Medications: The patient is on Tomoxifen, and feels that this is partially the reason why she is unable to lose weight. The patient has previously been on chemotherapy for her breast cancer in 2006, including Adrimyacin and cytoxin. Recommendations: The recommendation for treatment was no surgical intervention, and stereotactic radio surgery at the St. Paul Cancer Center was to be considered. The patient was to obtain a biopsy to delineate whether these were metastases from her previous breast cancer. From there, the patient’s Warfarin was held for diagnosis to see if her elevated calcium blood levels were due to her bony metastases. The patient opted for radiation treatments to her symptomatic skull metastases. The Plan (Prescription): The plan is for the patient to receive a total of 30 Gray (Gy), ten fractions, 300 centigray (cGy) per fraction to her whole brain and skull. The plan is an external beam treatment technique consisting of left anterior obliques and right anterior obliques. The prescription is also scheduled for the patient to be treated once per day, and five fractions per week, for a total of ten fractions. The patient was simulated on a Friday, and the plan was created that same day so she could receive her first treatment that same day. She was also treated on that Saturday. Patient Setup/Immobilization: The patient was simulated in the supine position. Set up for the table included a head frame for the face mask to be mounted, and an Accuform mold for her headrest. Her feet rest atop a bolster, and her toes are held in a toe band. Her arms are on her stomach holding the foam ring. An aquaplast mask was used for head immobilization. Because the treatment is focused to her skull, there is the need to create a bolus to bring the dose to the level of her skull. A therapist and I used Sivco plastic bolus, as depicted in figure 1, and heated it in a water bath until it was pliable. The patient still has her hair, we were concerned with whether the bolus would shrink upon removal from the patient’s head and it cooled. To compensate for this, her hair will act as a spacer, as well as a mesh stretch fabric we used to 3 create a sort of head covering to also protect the patient’s hair from sticking to the bolus. We pieced the bolus around JG’s head and trimmed any excess, which is illustrated in figure 2. The bolus skull cap will be separate from the aquaplast mask in order for the patient to get the cap to fit properly. The bolus cap will be worn daily until her treatment is complete. The doctor will also be consistently re-evaluating in order to detect any skin breakdown. If the patient experiences this issue, she will then be re-simulated to account for treatments without the bolus and to plan for any differences in the mask fitting. JG was evaluated around treatment five, and it was determined that the bolus would not need to be discontinued for her future treatments. For treatment setup, radiation therapists would setup three-point to marks on the mask that have been placed with the coordinates of the isocenter according to what is calculated within the radiation treatment plan. Anatomical Contouring: Anatomical contouring included eyes and lenses, the brain, external body, and the skull. The scan was done with everything in treatment position, including the bolus. Beam Isocenter/Arrangement: The collimators were at zero for all four fields and so was the couch angle. The isocenter for all fields was set by the doctor after the three dimensional computed tomography (3D CT) scan through the Advantage Simulation Program. This location was transferred over to the treatment planning system: Eclipse. The isocenter and calculation reference point for all four total beams are at location x:0, y:0, z:0, and the energy was set at 6 MV (megavoltage) for all four beams as well. Treatment Planning: The plan consisted of four beams, two right anterior obliques (RAO) and two left anterior obliques (LAO). One complication with this treatment plan was that the dose needed to fully cover the entire skull. With regular whole brain treatments, there is the buildup region before the dose maximum is reached, and for this treatment we need the dose maximum to be falling in the skull. This was accounted for by utilizing the skull cap bolus. The beams incorporated multi-leaf collimator (MLC) blocks to avoid dose to the eyes and lenses, and field in field set ups to eliminate hot spots. The patient will be treated on Varian’s EX Clinac Linac with all fields at the energy of 6MV. The field sizes and properties are listed in figure 3. 4 Monitor Unit (MU) Check: RadCalc was used to check the doses by computer. The information for Source to Skin Distance (SSD) and the equivalent path length was entered per field, and the method for calculating scatter was selected. Because there is a certain amount of air and field irregularity, the Blocked Equivalent Square method was used. The deviation percentages from actual planned MU’s are evaluated by showing how accurate the reading is. At the St. Paul Cancer Center, percentages over +/-5% are unacceptable for treatments. Quality Assurance Check: For the quality assurance checks, the Physicist and Junior Physicist calculated what the monitor units (MU’s) should be per field, and then the plan was run on phantoms on a linear accelerator where the output per field was taken. This value was then compared to the expected MU values, ensuring that the plan is safe for treatment. Conclusion: I have had the unique opportunity to witness another rare treatment setup and plan. I chose this case due to its rarity and the amount of hands on I had in the patient’s simulation. I had only seen setups like this treated a couple of times through my radiation therapy internship, but the bolus was usually located on top of the aquaplast mask, and for this case the bolus was formed to be worn under the mask. The concept of bringing the dose at depth maximum (dmax) closer to the surface in order to adequately treat the skull was something that was very interesting to see, especially while being planned. I thought it would be a good case study to evaluate and delve further into the details, since effectively moving the dmax is a common concept in radiation treatment planning. This was a challenge for me in that I was lacking previous experience in planning a case similar to this. I was able to watch the initial CT simulation and the resimulation, along with the treatment machine simulation to trace the steps from planning simulation to treatment. I feel that I have learned a lot from working on this plan. This case also illustrated how important the simulation is in creating a successful and effective treatment plan, and to ensure patient comfort. I was able to see concepts put into actual treatment planning, and to critically evaluate these concepts. This was another case that I had a great opportunity to witness and be involved in. Cases like these are effective in maintaining my adaptability and application of book concepts. I hope to be able to use concepts like these in future cases. 5 Figure 1: Sivco plastic bolus prior to being heated up for molding. 6 Figure 2: Picture documenting the fit and structure of the bolus skull cap. The patient’s face has been removed to maintain her confidentiality. Figure 3: Field sizes and parameters for all four fields.