File - Jessica Pitzer
advertisement

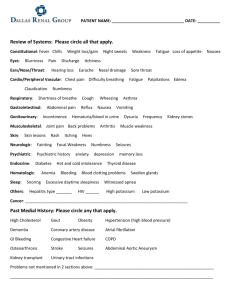
Diet Instruction Jessica Pitzer KNH 413 Renal Diet for Dialysis Description of patient and diagnosis Client: 45 years old white male, Mark Manning. He was diagnosed with stage 5 chronic kidney diseases one year ago. Mark was diagnosed with type 2 diabetes at age 40. His doctors then ordered him to be on a renal diet for dialysis. Mark is an accountant that works at a big corporation. Mark lives in Phoenix, Arizona with his two children and wife. Being recently ordered to kidney dialysis, the doctor requested that Mark see a dietician to aid with his hemodialysis. Mark works out 2 times a week and is always on the run with his children. Anthropometric Measurement: BMI: 24kg/m2 (Normal) Weight 180lb Height: 5’10 BP: 118/89 Activity level: Active Discussion of the disease Chronic kidney disease (CKD) is permanent, progress loss of kidney function characterized by a decline in glomerular filtration rate. It includes conditions that damage your kidneys and decrease its ability to keep you healthy by doing the jobs listed. If kidney disease gets worse, waste can build to high levels in your blood and make you sick. You may develop complication like high blood pressure, anemia, weak bones, poor nutritional health and nerve damage. When kidney disease progresses, it may eventually lead to kidney failure, which requires dialysis or a kidney transplant to maintain life. The National Kidney Foundation Kidney Disease Outcome Quality Initiative classified CKD into five stages based on GFR level. At stage 5, dialysis is needed to support life. Two simple tests can detect chronic kidney disease. Blood pressure, urine albumin and serum creatinine are the easiest tests to run to detect CKD. Etiology (5 points) The two main causes of chronic kidney disease are diabetes and high blood pressure, which are responsible for up to two-thirds of the cases. Diabetes happens when your blood sugar is too high, causing damage to many organs in your body, including the kidney and hear, as well as blood vessels, nerves and eyes. High blood pressure, or hypertension, occurs when the pressure of your blood against the walls of blood vessels increases. If uncontrolled, or poorly controlled, high blood pressure can be a leading cause of heart attacks, strokes and chronic kidney disease. There are also causes where chronic kidney disease actually causes high blood pressure. Glomerulonephritis is a group of diseases that causes inflammation and damage to the kidney’s filtering units. These disorders are the thirst most common type of kidney disease. Inherited disease, such as polycystic kidney disease, which causes large cysts to form in the kidneys and can damage the surrounding tissue causing CKD. Malformations that occur as a baby develops in its mother’s womb can cause kidney problems. For example, a narrowing may occur that prevents normal outflow of urine and causes urine to flow back up into the kidney causing infection and damage. Minor problems such as kidney stones, repeated urinary infections, tumors, or an enlarged prostate gland in men can cause an obstruction leading to possible kidney damage. Diagnostic Measures To determine whether chronic kidney disease, there are a few different tests that can be done. Blood pressure, urine albumin and serum creatinine are the easiest tests to run to detect CKD. Blood tests of kidney function look for the level of waste products, such as creatinine and urea in the blood. Analyzing a sample of urine may reveal abnormalities that point to chronic kidney failure and help identify the cause of chronic kidney disease. Image tests may be used in some cases. Doctors may use ultrasound to asses kidney’s structure and size. Lastly, the doctor can do a biopsy to remove a sample of the kidney tissue. Kidney biopsy is often done with local anesthesia using a long, thin needle that’s inserted through your skin and into your kidney. (Mayo Clinic) Treatment A lot of the time chronic kidney disease cannot be treated, but depending on the underlying cause, some types of kidney disease can be treated. In general, treatment consists of measures to help control signs and symptoms, reduce complications, and slow progression of the disease. If kidneys become severely damaged, treatment may be needed for end-stage kidney disease. If kidneys can’t keep up with waste and fluid clearance on their own and near-complete kidney failure is reached, you have end-stage kidney disease. At that point, dialysis or a kidney transplant is needed. Dialysis artificially removes waste products and extra fluid from your blood when your kidneys can no longer do this. In hemodialysis, a machine filters waste and excess fluids from your blood. In peritoneal dialysis, a thin tube (catheter) inserted into your abdomen fills your abdominal cavity with a dialysis solution that absorbs waste and excess fluids. After a period of time, the dialysis solution drains from your body, carrying the waste with it. A kidney transplant involves surgically placing a healthy kidney from a donor into your body. Transplanted kidneys can come from deceased or living donors. You'll need to take medications for the rest of your life to keep your body from rejecting the new organ. (Mayo Clinic) Medical, surgical and/or psychological treatment As stated above, many times chronic kidney disease cannot be treated. Surgical procedures can be done such as a kidney replacement or hemodialysis. The most commonly used procedure for renal replacement therapy is hemodialysis. This procedure is performed at a dialysis center or at home. In-center hemodialysis is usually done for approximately 4 hours, three times a week, depending on residual renal function and body weight. Home hemodialysis can be done on a schedule similar to traditional incenter hemodialysis or as a short daily treatment (2 hours, five to six times a week) or a nocturnal treatment (6 to 8 hours, six times a week). The amount of dialysis prescribed is based on the elimination of urea. The dialysis treatment requires access to the circulatory system by a catheter, fistula, or graft. The dialysis process involves a filtering mechanism that has varying degrees of permeability. Fluid removal and reduction in serum electrolytes and toxin concentrations occur across a semipermeable membrane called the dialyzer. Both ultrafiltration and diffusion are performed during a typical hemodialysis session. The goal of the nutrition therapy for hemodialysis is to maintain optimal nutrition while limiting the buildup of waste products between hemodialysis treatments. Exercising can also help to improve the side effects from kidney disease. It can help maintain blood glucose and lower blood pressure. (Mayo Clinic) Medical Nutrition Therapy The purpose of medical nutrition therapy for chronic kidney disease is to maintain good nutritional status, slow progression, and to treat complications. Mr. Manning is ordered to a renal diet for hemodialysis. Malnutrition is a major concern with maintenance dialysis. Adequate dietary protein and energy intakes are needed to maintain protein balance and body composition and to reduce the risk for protein-energy malnutrition. A sodium and fluid restriction is recommended in maintenance dialysis to avoid large interdialytic weight gains (>4% of estimated dry weight), hypertension, edema, pleural effusion and congestive heart failure. A low-potassium diet in addition to maintaining optimal blood glucose control and treatment of constipation are indicated as needed to avoid hyperkalemia (the diet may be adjusted in accordance with serum potassium levels). Patients undergoing maintenance dialysis must also decrease phosphorus intake to avoid hyperphosphatemia. Phosphate binders are usually required to decrease intestinal absorption of phosphorus found in most foods. Foods higher in protein (and also higher in phosphorus) may be needed to maintain adequate protein stores, thus increasing the need for phosphorus binding therapies. Patients who are using calcium containing phosphate binders are instructed to limit total daily calcium intake from food and medications to <2000 mg per day to avoid hypercalcemia, which can cause hypertension and calcification of blood vessels, soft tissue, and organs, leading ultimately to calcific uremic areteriolopathy. Harris Benedict= 66.5+ (13.75 x wt in kg)+ (5 x height in cm)- (6.78 x age) 66.5+ (13.75 x 82 in kg)+ (5 x 178cm)- (6.78 x 45)= 1,779 kcals Protein: 98 grams Carbohydrate: 935 kcals Fat: 425 kcals Protein >1.2 g/kg of body weight, >50% HBV protein Energy < 60 yrs of age: kg of body weightx35kcal; >60 yrs of age:kg of body weight x 30 kcal/kg to 35kcal/kg Sodium less than 2.4g/day Potassium less than 2.4g/day Phosphorus 800 mg/day to 1,000 mg/day or 10-12mg phosphorus per gram of protein when serum phosphorus >5.5 mg/dL or intact PTH is elevated Calcium total elemental intake (including dietary calcium, calcium supplementation and calcium-based binders) should not exceed 2 g/day Fluid: Urine output plus 1,000 cc Vitamins/Minerals: o Vitamin C: 60 mg/day to 100 mg/day o Vitamin B-6: 2 mg/day o Folate: 1-5mg/day (McCann 2009) o Vitamin B-12: 3 mcg/day o DRI for all other water-soluble vitamins o Vitamin E: 15 international units/day o Zinc: 15 mg/day o Iron: IV supplementation recommended if serum ferritin below 200 ng per ml and TSAT below 20% o Vitamin D: It is suggested that 25-hydroxyvitamin D levels might be measured with deficiency or insufficiency being corrected using treatment strategies recommended for general population (Nutrition Care Manual) Prognosis Many people are not diagnosed with chronic kidney disease until they have lost most of their kidney function. There is no cure for chronic kidney disease. If it worsens to endstage renal disease, and how quickly, depends on the cause of the kidney disease and how well you take care of yourself. Kidney failure is the last stage of chronic kidney disease. This is when your kidneys can no longer support the body’s needs. Even people who are waiting for a kidney transplant may need dialysis while waiting for a transplant. If the transplant is not received in time then dialysis will be needed to replace all of kidney’s function. If the patient does not take care of himself or herself the disease can lead to death. (Medline Plus) References: About Chronic Kidney Disease. (n.d.). Retrieved March 10, 2015, from https://www.kidney.org/kidneydisease/aboutckd American Association for Kidney Patients. Suggested Foods for Dialysis Patients. (n.d.). Retrieved March 10, 2015, from https://www.aakp.org/education/resourcelibrary/ckdresources/item/foods-for-dialysis-patients.html Fresenius Medical Care. Meal Planning. (n.d.). Retrieved March 10, 2015, from http://www.ultracare-dialysis.com/HealthyLifestyles/EatHealthy/MealPlanning.aspx Mayo Clinic. Chronic kidney disease. (n.d.). Retrieved March 10, 2015, from http://www.mayoclinic.org/diseases-conditions/kidney-disease/basics/testsdiagnosis/con-20026778 Medline Plus. Chronic kidney disease: MedlinePlus Medical Encyclopedia. (n.d.). Retrieved March 10, 2015, from http://www.nlm.nih.gov/medlineplus/ency/article/000471.htm National Kidney and Urologic Diseases Information Clearinghouse (NKUDIC). (n.d.). Retrieved March 10, 2015, from http://kidney.niddk.nih.gov/KUDISEASES/pubs/eatright/index.aspx NCM Nutrition Care Manual eat right. (n.d.). Retrieved March 10, 2015, from https://www.nutritioncaremanual.org/topic.cfm?ncm_category_id=1&lv1=5537&lv2=25 5347&ncm_toc_id=255666&ncm_heading=Nutrition Care Nephrology Physicians LLC. Kidney Dialysis Food Lists - Nephrology Physicians, LLC. (n.d.). Retrieved March 10, 2015, from https://www.nephinc.com/food-lists.asp The Hemodialysis Diet. (n.d.). Retrieved March 10, 2015, from http://www.davita.com/kidney-disease/diet-andnutrition/diet-basics/the-hemodialysisdiet/e/5314 UNC Kidney Center. (n.d.). Retrieved March 10, 2015, from http://www.unckidneycenter.org/kidneyhealthlibrary/CKD/Dietary Guide for CKD Patients.pdf