Chapter 16 The Reproductive System
advertisement

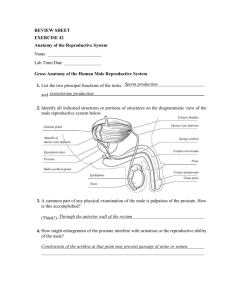
Chapter 16 The Reproductive System Most organ systems of the body function almost continuously to maintain the wellbeing of the individual. The reproductive system, however, appears to "slumber" until puberty. The primary sex organs, or gonads, are the testes in males and the ovaries in females. The gonads produce sex cells, or gametes, and secrete sex hormones. The remaining reproductive system structures are accessory reproductive organs. Although male and female reproductive systems are quite different, their joint purpose is to produce offspring. Anatomy of the Male Reproductive System Discuss the common purpose of the reproductive system organs. o Although the male and female reproductive systems are quite different, their joint purpose of to produce offspring o The primary sex organs, or gonads, are the testes in males and the ovaries in females The gonads produce sex cells, or gametes, and secrete sex hormones The reproductive role of the male is to manufacture male gametes called sperm and deliver them to the female reproductive tract while the reproductive role of the female is to produce female gametes called ova, or eggs and if the time is suitable, the sperm and egg fuse to produce a fertilized egg called a zygote The female uterus provides a protective environment in which the embryo, later called the fetus, develops until birth The remaining reproductive system structures are accessory reproductive organs When provided with a model or diagram, identify the organs of the male reproductive system and discuss the general function of each. o See figure 16.1 on page 505 o Testes – male gonads – have both an exocrine (sperm producing) and an endocrine (testosterone-producing) function Seminiferous tubules – actual sperm-forming factories Interstitial cells – produce androgens – mostly testosterone o Duct system – the accessory organs forming the male duct system that transports sperm from the body Epididymis – the first part of the male duct system and provides a temporary storage site for the immature sperm that enter it from the testis – sperm take 20 days to travel along the duct – they mature and gain the ability to swim along the way Ductus deferens – or vas deferens – runs from the Epididymis into the pelvic cavity and arches over the superior aspect of the bladder - enclosed in a connective tissue sheath called the spermatic cord – the end of the ductus deference empties into the ejaculatory duct, which passes through the prostate gland to merge with the urethra – function is to propel live sperm from their storage sites into the urethra At the moment of ejaculation, the thick layers of smooth muscle in its walls create peristaltic waves that rapidly squeeze the sperm forward Urethra – prostatic urethra is surrounded by the prostate gland, the membranous urethra spans the distance from the prostatic urethra to the penis and the spongy (penile) urethra runs within the length of the penis – carries both urine and sperm to the body exterior (never at the same time because the bladder sphincter constricts to prevent urine from entering the urethra and sperm from entering the urinary bladder) o Accessory glands and semen Seminal vesicles – produce 60% of the fluid volume of semen – thick, yellowish secretion is rich in sugar (fructose), vitamin C, prostaglandins which nourish and activate sperm passing through the tract Prostate gland – produces a milky fluid that plays a role in activating sperm that is released during ejaculation Bulbourethral glands – produces a thick, clear mucus that drains into the penile urethra and is the first to pass down the urethra – believed to cleanse the urethra of traces of urine and serve as a lubricant during sexual intercourse o External genitalia – scrotum and penis Scrotum – provides the testes with a temperature that is 3°C below body temperature so viable sperm can be produced – can change surface area in order to maintain a temperature that favors viable sperm production Penis – designed to deliver sperm into the female reproductive tract Name the endocrine and exocrine products of the testes. o Endocrine – testosterone o Exocrine – sperm Discuss the composition of semen and name the glands that produce it. o Semen is a milky white, somewhat sticky mixture of sperm and accessory gland secretions The liquid provides a transport medium and nutrients and contains chemicals that protect the sperm and aid their movement Fructose – provides all the energy fuel for the sperm Seminal plasmin – chemical that inhibits bacterial multiplication Relaxin – hormone Certain enzymes that enhance sperm motility Semen also dilutes sperm to maintain mobility Trace the pathway followed by a sperm from the testis to the body exterior. o Testis (Seminiferous tubules) rete testis Epididymis ductus deferens ejaculatory duct membranous urethra spongy (penile) urethra female reproductive tract Define erection, ejaculation, and circumcision. o Erection – when the three elongated areas of erectile tissue, the spongy tissue, fills with blood during sexual excitement causes the penis to enlarge and become rigid to help the penis to serve as a penetrating organ to deliver semen into the female’s reproductive tract o Ejaculation – the sudden ejection of semen from the penis o Circumcision – surgical removal of the foreskin, or prepuce, of the penis Male Reproductive Functions Define meiosis and spermatogenesis. o Meiosis – a special type of nuclear division that occurs only in the gonads and consists of two successive divisions of the nucleus and results in four daughter cells, or gametes, which have half the genetic material (23 chromosomes rather than 46 found in body cells) o Spermatogenesis – sperm production begins with spermatogonia (primitive stem cells), which go through rapid mitotic divisions to build up the stem cell line – produce two types of stem cells = type A daughter cells that remain at the tubule periphery to maintain the stem cell population and type B daughter cells get pushed toward the tubule lumen where they become primary spermatocytes destined to undergo meiosis and form four spermatids, non-motile cells that are not functional sperm Spermiogenesis – the spermatids slough off all excess cytoplasm and what remains is compacted into the three regions of the mature sperm – the head, midpiece, and tail o Process takes 64 – 72 days – spermatids are unable to “swim” until they reach the Epididymis where they undergo further maturation, which results in increased motility and fertilizing power Describe the structure of a sperm and relate its structure to its function. o Mature sperm have three regions – the head, midpiece, and tail Greatly streamlined cells equipped with a high rate of metabolism and a means of propelling itself o Head contains DNA – the nucleus of the spermatid Anterior to the nucleus is the helmet-like acrosome, which is similar to a large lysosome, which breaks down when the sperm reaches an oocyte to help the sperm penetrate through the follicle cells that surround the egg o Tail contains filaments that arise from centrioles in the midpiece Mitochondria wrapped tightly around these filaments provides the ATP needed for the whip-like movements of the tail Describe the effect of FSH and LH on testis functioning. o FSH – follicle-stimulating hormone – released by the anterior pituitary gland – stimulates the seminiferous tubules to produce sperm o LH – luteinizing hormone – interstitial cell-stimulating hormone (ICSH) – released by the anterior pituitary gland activates interstitial cells o Anatomy of the Female Reproductive System When provided with an appropriate model or diagram, identify the organs of the female reproductive system and discuss the general function of each. o See figure 16.8 on page 513 o Ovaries – paired structures containing many tiny saclike structures called ovarian follicles – each follicle consists of an immature egg, oocyte, surrounded by one or more layers of follicle cells o Duct system – fallopian tubes, uterus, vagina Uterine (fallopian) tubes – initial part of the duct system that receives the ovulated oocyte and provides a site where fertilization can occur Not connected to the ovaries – the distal end of each uterine tube expands as the funnel-shaped infundibulum, which has fingerlike projections called fimbriae that partially surround the ovary As an oocyte is expelled from the ovary, the waving fimbriae create fluid currents that carry the oocyte into the uterine tube – movement of the oocyte after it enters is via peristalsis and beating of cilia Uterus – functions to receive, retain, and nourish a fertilized egg (zygote) Vagina – birth canal – provides a passageway for the delivery of the infant and for the menstrual flow to leave the body – also receives the penis during sexual intercourse making it the female organ of copulation o External genitalia – located external to the vagina and called the vulva Mons pubis and the labia majora are hair-covered folds Labia minora and the vestibule are hairless folds – the vestibule contains the external openings of the urethra followed posteriorly by that if the vagina Greater vestibular glands – secrete lubricants during intercourse Clitoris – anterior to the vestibule and is composed of sensitive erectile tissue that become swollen with blood during sexual excitement similar to the male penis but it lacks a reproductive duct Perineum – the diamond-shaped region between the anterior end of the labial folds, the anus posteriorly, and the ischial tuberosities laterally Describe the functions of the vesicular follicle and corpus luteum of the ovary. o Vesicular (Graafian) follicle – a mature follicle with developing egg inside that is ready to be ejected from the ovary during ovulation o Corpus luteum – the ruptured follicle is transformed into a very different looking structure (yellow body) that eventually degenerates – what’s left of the follicle The corpus luteum produces progesterone that makes the lining of the uterus thick for implantation and is necessary to sustain a healthy pregnancy. Define endometrium, myometrium, and ovulation. o Endometrium – the inner layer or mucosa of the uterus wall – sloughs off periodically during menses when a woman is not pregnant – after fertilization, the fertilized egg burrows into this layer in the process called implantation o Myometrium – the bulky middle layer of the uterus composed of interlacing bundles of smooth muscle that contract during labor to force the baby out o Perimetrium – outermost serous layer of the uterus – visceral peritoneum o Ovulation – when an mature oocyte is ejected from the ovary Indicate the location of the following regions of the female uterus: cervix, fundus, body. o Body – the major portion of the uterus o Fundus – the superior rounded region above the entrance of the uterine tubes o Cervix – the narrow outlet which protrudes into the vagina below Female Reproductive Functions and Cycles Define oogenesis. o The process during which the female gametes, or sex cells, are produced – the beginning of an egg Oogonia – female stem cells multiply rapidly to increase their numbers in the developing female fetus – no longer exist by birth Primary oocytes – daughter cells of oogonia – push into the ovary connective tissue where they become surrounded by a single layer of cells to form the primary follicles At birth, the female’s lifetime supply of primary oocytes is already in place in the ovarian follicles awaiting the chance to undergo meiosis to produce functional eggs Remain in a state of suspended animation all through childhood – until puberty As a follicle is stimulated by FSH grows larger, it accumulates fluid in the central chamber called the antrum and the primary oocyte begins meiosis I resulting in two cells of dissimilar size – a large secondary oocyte and a tiny polar body Mature (vesicular follicle) stage – contains a secondary oocyte and protrudes from the external surface of the ovary – is released then luteinizing hormone (LH) is released by the anterior pituitary Still surrounded by its follicle-cell capsule called the corona radiate (radiating crown) If the ovulated secondary oocyte is penetrated by a sperm, its nucleus undergoes meiosis II that produces another polar body and the ovum nucleus, which is then combined with the sperm nucleus to form the fertilized egg (zygote) Describe the influence of FSH and LH on ovarian function. o FSH – hormone released by the anterior pituitary gland that stimulates a small number of primary follicles to grow larger and accumulate fluid in the central chamber called the antrum and to begin meiosis I and mature each month – results in a cyclic change that occurs monthly in the ovary called the ovarian cycle o LH – luteinizing hormone – hormone released by the anterior pituitary gland stimulates the release of a mature follicle into the peritoneal cavity (space between the ovary and the uterine tube) in a process called ovulation – also causes the ruptured follicle to change into the corpus luteum Describe the phases and controls of the menstrual cycle. o Menses – Days 1-5 – the functional layer of the thick endometrial lining of the uterus is sloughed off – accompanied by bleeding for 3-5 days – by day 5, growing ovarian follicles are beginning to produce more estrogen o Proliferative stage – Days 6-14 – rising estrogen levels produced by the follicles of the ovaries, the basal layer of the endometrium regenerates the functional layer, glands are formed in it, and the endometrial blood supply is increased Ovulation occurs in the ovary at the end of this stage due to the sudden surge of LH in the blood o Secretory stage – Days 15-28 – rising levels of progesterone production by the corpus luteum of the ovary act on the estrogen-primed endometrium and increase its blood supply even more – progesterone also causes the endometrial glands to increase in size and to begin secreting nutrients into the uterine cavity If fertilization does occur – the embryo produces a hormone similar to LH that causes the corpus luteum to continue producing hormones If fertilization does not occur – the corpus luteum begins to degenerate toward the end of this period as LH levels decline – lack of ovarian hormones in the blood cause the blood vessels supplying the functional layer of the endometrium to go into spasms and kink depriving the endometrial cells of oxygen and nutrients and causing them to die, which sets the stage for menses to begin again Mammary Glands Describe the structure and function of the mammary glands. o Present in both males and females but only functional in females after reproduction has been accomplished – function is to nourish a newborn baby o Developmentally, the mammary glands are modified sweat glands that are actually part of the skin – each is contained within a rounded skin-covered breast anterior to the pectoral muscles of the thorax o Areola – pigmented area slightly below the center of each breast and surrounds a central protruding nipple o Internally, each consists of 15-25 lobes which radiate around the nipple – lobes are padded and separated from each other by connective tissue and fat Within each lobe are smaller chambers called lobules, which contain clusters of alveolar glands that produce milk when a woman is lactating (producing milk) The alveolar glands of each lobule pass the milk into the lactiferous ducts, which open to the outside at the nipple Survey of Pregnancy and Embryonic Development Define fertilization and zygote. o Fertilization – occurs at the moment the genetic material of a sperm combines with that of an ovum to form a fertilized egg, or zygote o Zygote – the first cell of the new individual Describe implantation. When the young embryo burrows into the endometrium of the uterus and resides there for the rest of its development Distinguish between an embryo and a fetus. o Embryo – early stage of development – development stage until ninth week o Fetus – beginning at the ninth week the embryo is called a fetus until it is born List the major functions of the placenta. o By the third week – functions to deliver nutrients and oxygen to and remove wastes from the embryonic blood o By the end of the second month – becomes an endocrine organ and is producing estrogen, progesterone, and other hormones that help maintain the pregnancy Indicate several ways that pregnancy alters or modifies the functioning of the mother's body. o Anatomical changes Enlargement of the uterus Center of gravity changes – accentuated lumbar curvature (lordosis), often accompanied by backaches Pelvic ligaments and the pubic symphysis relax, widen, and become more flexible due to production of the hormone relaxin by the placenta Weight gain – an additional 300 calories per day is necessary for proper fetal growth o Physiological changes Gastrointestinal system Morning sickness – nausea during the first few months until system adjusts to elevated levels of progesterone and estrogens Heartburn – the growing uterus crowds the stomach and displaces the esophagus, which favors reflux of stomach acid into the esophagus Constipation – motility of the digestive tract declines Urinary system Kidneys – have additional burden of disposing of fetal metabolic wastes and produce more urine Bladder – compression by the uterus causes urination to be more frequent, more urgent, and sometimes uncontrollable – stress incontinence Respiratory system Nasal mucosa – increased levels of estrogen cause them to swell and become congested causing nasal stuffiness and occasional nosebleeds Vital capacity and respiratory rate increase but residual volume declines – dyspnea (difficulty breathing) may occur during later stages of pregnancy Cardiovascular system Blood pressure and pulse rise and cardiac output increases due to greater blood volume and total body water increase Varicose veins – the uterus presses on pelvic blood vessels and venous return from lower limbs may be impaired Describe how labor is initiated and briefly discuss the three stages of labor. o Initiation – during last few weeks of pregnancy, estrogens reach highest levels causing the myometrium to form abundant oxytocin receptors so it becomes more sensitive to the hormone and it interferes with progesterone’s quieting influence on the uterine muscle causing weak, irregular uterine contractions called Braxton Hicks contractions to begin (false labor) o Stage 1 – dilation stage – from the appearance of true contractions until the cervix is fully dilated by baby’s head – regular but weak contractions begin in the upper part of the uterus and move downward toward the vagina and gradually become more vigorous and rapid as o the infant’s head is forced against the cervix, the cervix softens, becomes thinner (effaces) and dilates – the amnion ruptures releasing the amniotic fluid (breaking the water) o Stage 2 – expulsion stage – period from full dilation to delivery of the infant – mother experiences increasing urge to push, or bear down, with abdominal muscles until the infant passes through the cervix and vagina to the outside of the body o Stage 3 – placental stage – delivery of the placenta usually takes place within 15 minutes after the birth of the infant – strong uterine contractions continue after birth compress uterine blood vessels, limiting bleeding and cause the placenta to detach from the uterine wall Afterbirth – the placenta and its attached fetal membranes List several agents that can interfere with normal fetal development. o Alcohol, nicotine, drugs such as anticoagulants, antihypertensives, sedatives, some antibiotics, maternal infections such as German measles Developmental Aspects of the Reproductive System Describe the importance of the presence/absence of testosterone during embryonic development of the reproductive system organs. o Indifferent stage – embryonic reproductive structures of males and females are identical After the gonads have formed, development of the accessory structures and external genitalia begins and whether male of female structures form depends entirely on whether testosterone is present or absent If testosterone is present – the development of the male duct system and external genitalia follows If testosterone is absent – the female ducts and external genitalia result Define menarche and menopause. o Menarche – the first menstrual period o Menopause – when ovulation and menses cease, ending childbearing ability List common reproductive system problems seen in adult and aging males and females. o Females Adult – vaginal infections are common such as Escherichia coli, sexually transmitted microorganisms such as gonorrhea, syphilis, and herpes virus, and fungal infections (yeast) – untreated infections may spread throughout the female reproductive tract causing pelvic inflammatory disease and sterility Aging – estrogen levels drop after menopause causing the atrophy of reproductive organs and breasts – vagina becomes dry leading to frequent vaginal infections – mood changes – intense vasodilation of the skin’s blood vessels which causes hot flashes – gradual thinning of the skin and loss of bone mass – slowly rising blood cholesterol levels o Males Adult – common inflammatory conditions in males are urethritis, prostatitis, and epididymitis, all of which follow sexual contacts in which sexually transmitted disease (STD) microorganisms are transmitted – orchiditis, inflammation of the testes can cause sterility and also follows STD or mumps Aging – no equivalent of menopause for males – although aging men exhibit a steady decline in testosterone secretion, their reproductive capabilities seems unending and healthy men of all ages are able to father offspring