Communicable Diseases
advertisement

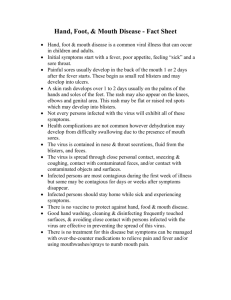
Communicable Diseases What does communicable disease mean? A disease that can be transmitted from one person to another Definitions Epidemic- disease that spreads rapidly Endemic- a continued incidence of a disease in a certain environment or area Pandemic- high incidence of a disease in a large area (can be worldwide) Infectious Agent- causes disease Incubation period- a period of time between the invasion of organism and onset of symptoms Prodromal period- 1st stage of disease Carrier- one who carries the disease Host- provides nourishment 9ex. Tick feeds off mammals Fomites- contaminated objects (bedrails, toys) Mode of Transmission Direct Contact- touch infected person Indirect contact- touching contaminated surface Droplet- cough, sneeze, flu Airborne- chicken pox Fecal-oral (contaminated food/water) Vector- (tick) animal or insect that spreads disease Host Resistance Intact Skin Phagocytes Immune system Transmission of Disease Causative Agent Immune Host Conducive Environment Immunity Natural Immunity (Innate)- naturally exists without a response, protected by chemical/physical barriers Active Immunity- naturally or artificially acquired Naturally acquired- obtain the disease Artificially Acquired- immunization Passive Immunity- injection of antibodies Immune globulin, gamma globulin (artificially acquired passive immunity) Naturally Acquired passive immunity Neonates received antibodies from the mother Contracting Disease How do we get infection? Must have a portal of entry- cut in the skin, mouth, eyes, ears, nose, etc. Some organisms can pass through unbroken skin Childhood Prevention How do we help prevent childhood diseases? Immunizations Route of administration: oral, subcutaneous, and IM Can prevent the disease Use correct storage Contraindications for Immunizations with live virus: Immunocomprimised, steroid therapy Pregnancy Bacteremia, Acute illness with or without fever Meningitis History of high fevers or severe reaction after previous immunization 2 month old 15 month old 4-6 years Allergies to Vaccines MMR, IPV, varicella- ask if allergic to Neomycin MMR- report allergy to eggs, gelatin Recombinant hepatitis B- ask if allergic to baker’s yeast Have Epi on hand in case of reaction Vaccines Do not give a TB test within 6 weeks of MMR or varicella vaccine, will give a false reading Give varicella and MMR the same day. If given MMR, must give varicella within 28 days Inform female clients to refrain from getting pregnant for 3 months after receiving Rubella vaccine. Nursing Responsibilities Reduce pain at injection site- use sprays or creams to numb the area prior to the injection Give injection properly Vaccine Reactions Mild fever- use Tylenol or Motrin Irritable Redness and tenderness at the site Severe Reaction High pitched cry, consistent high fever (104), seizures, increased sleep, unresponsive Rashes First sign of infection Erythema- redness Macule- reddened circular area Papule- raised reddened circular area Vesicle- raised reddened circular area that contains fluid Pustule- raised reddened circular area that contains pus Salmonella Infection Transmission- Bacteria from mishandled raw poultry, can obtain from reptiles and pets Causes: gastroenteritis, meningitis, osteomyelitis Gastroenteritis is most common Symptoms start about 12-72 hours after infected and last 3-7 days Symptoms: NVD , cramping and fever Will resolve within a week in a healthy child Dx: stool specimen and history and physical Treatment: antibiotics, hydration Shigellosis Bacteria ingested by fecal/oral route Symptoms can occur as early as 2-4 days after infection, but can take up to a week. Last for several days-weeks. Symptoms: Fever, N/V, severe diarrhea with blood/mucous stools, stomach cramps Dx: Stool specimen, Hx Treated: antibiotics, fluids Shigellosis and Salmonella Decrease solid food intake Clear fluids, fruit juice, jello Avoid carbonated drinks/caffeinated drinks Encourage pedialyte Meningococcal Meningitis Patho: infection of the covering of the brain and spine (meninges) Enters the body indirectly into the blood stream- teeth, sinuses, tonsils, lungs, ears, skull fx. Bacteria attacks the meninges once in the blood stream Blood brain barrier broken Symptoms Under 3 months old- fever, vomiting, decreased fluid intake, irritable, lethargic Children 1 yr and older- headache, fever, nausea, vomiting, light sensitivity, neck stiffness or neck pain, seizures Brudzinkski’s sign- involuntary flexion of the arm, hip, knee when neck is passively flexed Kernig’s sign- inability to completely extend the leg out when the thigh is flexed to the abdomen when in a seated or supine position Dx: spinal fluid is cloudy, has increased WBC’s/protein, decreased glucose, increased CSF pressure Treatment: antibiotics, fluids, isolation 24 hours after antibiotics is started, seizure meds Nursing Care: decrease stimuli, dim lit room, decrease noise, use soft voice/touch(seizures) Report STAT- slowed pulse rate, irregular respirations, and increased blood pressure (Increased ICP) Fever: give antipyretics, sponge bath, hypothermia mattress Observe for slight change in LOC and for twitching, observe for joint pain If patient has a seizure, maintain patent airway. Remove any sharp objects. Observe seizure. Prevention: teach family to wash hands, may need to take prophylactic antibiotics if not fully vaccinated for Hib Diphtheria Patho: bacteria causes toxins, destroys the myelin sheath which causes improper function of the nervous system Toxins produce a pseudomembrane (false membrane) in the throat Incubation: 2-5 days Symptoms: upper respiratory infection with sore throat, fever, fatigue, “bull neck” in severe cases, fast heart rate Spreads by direct contact or breathing in secretions from infected person Eradicated in developed countries due to vaccines Treatment: diphtheria antitoxins given, antibiotics, bed rest, hydration, adequate diet Nursing care: Isolate patient, watch for difficulty breathing, eating and swallowing Pertussis Whooping cough- starts as a mild respiratory infection, the cough develops with an inspiratory whoop (high pitched crowing) sound Infected person starts to have coughing fits that can cause vomiting and appears person cannot catch their breath. Incubation: 2 days Spread by airborne discharges from the mucous membranes and direct contact Treatment: antibiotic shortness illness time period, bed rest, adequate fluid/nutrition intake, IV therapy, IV therapy, O2, maintain patent airway Tetanus Neurotoxin (most deadly toxin) lives in dead tissue, soil, and intestinal tract of cows and horses Patho: neurotoxin enters the body through a wound, cut or bloodstream Incubation: 3-21 days Symptoms: Irritability, headache, spasms to the muscles causing lockjaw, eventually every muscle is affected. Treatment: Maintain airway, antitoxin as prescribed ASAP, may need to be sedated and ventilated. Prevention: Cleansing and debridement of the wound, booster shot of tetanus toxoid if previously immunized, tetanus immune globulin for those not immunized. Who would be at high risk and need to be given a tetanus shot? Burn victims, accident victims, children Typhoid Fever Patho: contaminated food or water with feces of infected person, the bacteria invades the macrophages and becomes resistant to the immune response. Spreads through the lymph system and the organs Incubation: lasts up to 60 days Symptoms: High fever (104.0), non-bloody diarrhea, profuse sweating, gastroenteritis Diagnosis: blood test, bone marrow, or stool cultures Treated: antibiotics Most cases are nonfatal Nursing Care: sponge bath for fever, hand washing a must, do not allow infected person to handle food others will eat, hydration Measles (Rubeola) Caused by a virus, spread airborne through the respiratory system by cough, nose, or mouth of infected person Incubation: 7-14 days Symptoms: fever, cough, conjunctivitis, Koplik’s spots which appear before the rash, photophobia Dx: Koplik’s spots, blood work Koplik’s spots are found on the mucosa, they are red with blue/white center 1-2 days after spots in mouth rash appears first on the face (macule-papules) red/blotchy appearance Complications Diarrhea Pneumonia Encephalitis Death (higher- underdeveloped countries) Nursing Considerations Bed rest, isolation, antipyretics, calamine lotion, dispose of contaminated tissues properly, teach that the skin will shed (desquamation) after the rash starts fading Prevention: immunization at age 12-15 months Rubella (German measles) Rubella- viral disease, very contagious Spreads by droplet Incubation: 12-23 days Symptoms: mild upper respiratory infection, lymph nodes enlarged, fine red maculopapular rash, arthralgia Treatment: no special treatment, will last about 2-3 days Chicken Pox (Varicella) Patho: highly contagious viral infection, caused by herpes virus (varicella) Starts as macules---papules---vesicles Vesicles have clear liquid inside, break and become crusted Transmission- contact and droplet Dx: physical exam and culture of vesicles Incubation: 2-3 weeks, followed by fever, headache, malaise Lasts for a few days t weeks Symptoms: pruritic vesicular eruptions on the skin, usually on the back and chest, arms, neck, face. Treatment: bed rest, antipyretics, calamine lotion, antihistamines Mumps Viral diseases- swelling of the salivary (parotid) glands Incidence- higher in the winter and early spring Virus lives in the saliva 6 days prior t glands swelling and 9 days after swelling Transmission: direct contact, droplet Diagnosis- symptoms, antibody tests Symptoms- enlarge neck from salivary glands swelling, painful, headache, low grade fever Treatment: isolation, antipyretics, analgesics, hydration, may need IV therapy if client can’t swallow Complications: Sterility in men- orchitis (inflammation of the testicles) Meningitis Hearing loss Inflammation of the ovaries, does not affect sterility Rabies (hydrophobia) Virus found in wild animals that effects the central nervous system Transmission: spread by saliva, usually from a bite, can obtain by infected blood or tissue Animals: skunks, bats, dogs, raccoons, squirrels, fox After a bite, the virus travels through the nerve pathway and then to organs Incubation: 10 days up to 1 year Symptoms: fever, malaise, headache, paresthesia, myalgia If not treated early will lead to encephalitis, paralysis, coma, death Most cases are not fatal No treatment if virus reaches the nervous system Cleanse wounds, take immune globulin (given the day of exposure, day 3,7,14,28, 90) Prevention: get animals vaccinated for rabies and don’t touch wild animals Infectious Mononucleosis (Kissing Disease) Patho: infection of the Epstein-Barr Virus Incubation: up to 8 weeks and spread through saliva Dx: blood work shows large irregular nuclei and symptoms Symptoms: Fever Fatigue Weight Loss Pharyngeal Inflammation Petechiae Lymphadenopathy, spleenomegaly Treatment: rest and relief of symptoms Contact sports and strenuous activity should be avoided for one month Fifth Disease (erythema infectiosum) Caused by erythrovirus Bright red cheeks, rash to arms and legs Rash lasts for a few days to a couple weeks Treatment: none Rocky Mountain spotted fever (bacteria) Patho: caused by (Rickettsia rickettsii) Ticks obtain the disease while feeding on a host and pass it while feeding on a host. Male ticks transfer the disease to female ticks Rash occurs 2-5 days after the onset of fever Sixth day after symptoms a petechial rash will occur on the palms and soles of the feet. Vectors: American dog tick, Rocky Mountain wood tick Early Symptoms: Fever N/v Severe headache and muscle pain Late Symptoms Abdominal pain Joint pain Maculopapular rash Petechial rash Treatment Doxycycline- antibiotic immediately or can be deadly Hydration, rest Malaria Patho: vector-borne disease with protozoan parasites Infected mosquito transmits by feeding on host Theses parasites replicate in the red blood cells Mostly common in South and Central America, Africa, and Asia Symptoms: Anemia, tachycardia, SOB Fever Chills Nausea No vaccine Antimalarials- Aralen is drug of choice Prevention: wear insect repellant, use of netting, get rid of swamp areas Drug resistant protozoa is a concern Pinworms (Enterobiasis) Look like white thread and lives in the intestines, comes out of anus at night to lay eggs. Spread within large groups. Children ingest the eggs into their mouth. Notice child scratching rectum, irritable, weight loss, restless at night, vaginitis in girls Dx: Scotch Tape test Treatment: Anthelmintics Vermox- single dose, chewable tablet (pregnant women shouldn’t take) Povan- single dose, teach parents that it turns stools red and will stain clothing Nursing considerations: Teach children to wash their hands Keep nails trimmed Soothing ointment applied to rectum Roundworms (Ascariasis) (Trichinella) Live well in warm climates Caused by unsanitary disposal of human waste and poor hygiene Patho: eggs turn into larvae in the intestines, enter into the liver, circulate to the lungs/heart No symptoms until larvae gets into the glottis Eggs live a long time in the soil Children play outside and touch this contaminated soil Chronic cough and fever Diagnosis by stool specimen Treatment is the same as for Pinworms Syphilis Patho: caused by a spirochete, transmitted by sexual contact Can be transmitted by saliva or bodily fluids Incubation: 20-30 days Spreads through the blood and lymphatic system Clinical Stages: Primary Painless ulcer (chancre) at the inoculation site Regional lymph nodes swollen Highly infectious Chancre appears abut 3-4 weeks after contact Secondary From 2 weeks- 6 months skin rash will appear after chancre has resolved Flu-like symptoms Alopecia General lymphadenopathy Will disappear in 2-6 weeks Latent Can last up to 50 years No symptoms Unable to transmit disease Tertiary 2 different forms Benign Late syphilis- localized infiltrating tumors in skin, bones, and liver Diffuse inflammatory response- involvement of the nervous system Both can be treated Diffuse response- cardiovascular and nervous system damage is irreversible Diagnostic Test VDRL and RPR- positive in 4-6 weeks FTA-ABS- confirm VDRL, RPR Treatment PCN-G intramuscular If allergic to PCN, oral doxycycline given Teach client prevention measures Tests for other STD’s needed Congenital Syphilis Transferred to the fetus via placenta Gonorrhea Known as “clap” Most common communicable disease Patho: Neisseria gonorrhoeae- gram negative bacteria Incubation: 2-8 days Transmission: sexual contact and delivery of neonates Cervix and male urethra are targeted, disease will spread to other organs Males- inflammation of prostate, epididymis, and periurethral glands Women- PID, endometritis, salpingites (fallopian tubes), and pelvic peritionitis Symptoms: Males No symptoms Dysuria Serous to purulent urethral damage Regional lymphadenopathy Females No symptoms Dysuria Urinary frequency Abnormal vaginal discharge Diagnostic Tests Men- smear of urethral discharge Women- culture of cervical discharge Treatment starts before culture results obtained Teach: Abstain from sexual contact Both client and partners are to be treated Use condoms for future sexual contact Follow up 4-7 days for recheck at the MD’s office Treatment: Penicillin Genital Herpes 45 million people in the US have contracted genital herpes Cause: herpes simplex virus type 2 Herpes simples virus type 1---cold sores High in teens and young adults Symptoms go unnoticed or has no symptoms Patho: the virus spreads through sexual contact Incubation: 3-7 days Week after exposure: painful red papules appear in the genital area Papules form blisters (clear fluid filled) Blisters break, shed virus-become ulcers Ulcers last up t 6 weeks or longer Autoinoculation- if you touch the ulcers they can spread to anywhere on the body First episode infection- first outbreak Subsequent outbreaks- recurrent infections Latency- period between outbreaks, lays dormant in the nerve fibers Prodromal symptoms of outbreaks (warning signs) Burning Itching Tingling Throbbing at common lesion area Pain radiation to the legs, thighs, groin or buttocks Can infect others during the prodromal symptoms Can transmit at birth Higher risk for cervical cancer in women Rare- herpes encephalitis, life threatening No cure Dx: symptoms, H/P Prevent spread of disease- abstinence or condoms Relieve symptoms Treatment Antivirals- acyclovir (Zovirax), famciclovir (Famvir) Acyclovir can be given IV, PO, or topical cream Valtrex given PO Creams accelerates healing time PO meds minimizes the number of outbreaks Nosocomial Infections What is a Nosocomial infection? Hospital acquired 2 million patients are affected each year Most common site: UTI’s Invasive procedures More than 2 million clients a year obtain a Nosocomial infection About 4-6% nationally affected **** Centers for Disease Control and prevention monitors nosocomial infection rates Risk factors: Chronic diseases- AIDS, Renal, DM Morbid obesity Major surgery Invasive procedures Burns length of hospital stay Very young, very old Invasive procedures Prosthetic devices History of frequent antibiotic use Infections in other sites Burns Length of hospital Sites for Nosocomial Infections Urinary due to catheterization or urological procedures UTI’s number one nosocomial infection Surgical wounds- staph aureus Respiratory tract Bloodstream Prevention Hand washing is the #1 way to prevent transmission of nosocomial infection Wash hands before and after putting gloves on Autoclaving- ensures destruction of all pathogens Hospitals/Facilities- policies and procedures for infection control issues Pathogens Escherichia Coli- in the gut/intestines Staphylococcus Aureus- in nose, on skin Group A streptococci- starts in the throat or skin then further disease to lung, blood Enterococcus- lives in feces- UTI’s, Bacteremia, wound infections Staphylococcal infection Toxins can live in food and on dry surfaces Food poison- improper storage of food Wound infections- contact precautions Toxic shock syndrome- blood stream MRSA- resistive staph, contact precautions Infections When barriers are broken, the host becomes susceptible to infection of staph Treatment: Bed rest Analgesics Antibiotics Surgical Incision and Drainage MRSA Methicillin Resistant Staphylococcus aureus Staph that is resistant to the treatment of Methicillin (broad spectrum antibiotics) Exist in the hospital and community Carriers have colonized bacteria in their nose Cause: Staph lives in the nose and on skin (colonized in healthy people) Colonized people can show no symptoms but can spread the disease Bacteria enters the body through cut, wound Occurs in older patients and immunocompromised We are responsible for the resistant staph antibiotic resistance Using too many antibiotics Livestock are being fed antibiotics Germ mutation, drug companies can’t keep up Risk factors: Children- immune system not fully developed Participating in contact sports Sharing towels, equipment Weakened immune system Living in crowded areas/unsanitary Healthcare workers Recent hospitalization- surgical wounds, long inpatient stay, older adults, weak immune system Long term care facilities Recent antibiotic use Invasive devices- feeding tubes, catheters, etc. Healthcare workers transmit with their hands Lives on hands for more than 3 hours New resistant strains: VRSA- vancomycin resistant S. aureus VISA- intermediate- vancomycin- intermediate s. aureus Symptoms Skin infections- small, red bumps that look like a pimple Pimples can turn into deep, painful infection (surgical drainage) Can penetrate into the body causing life threatening infections (bone, bloodstream, heart valves, etc.) Diagnostic test: culture of wounds or nares Treatment- Vancomycin IV Adverse reactions- kidney and hearing damage, red man syndrome, petechial hemorrhages Red Man syndrome- red face, flushed, rash to face neck, upper torso (infuse slowly) Prevention Wash hands Use alcohol based sanitizer Use sterile technique and aseptic technique Don’t share personal items Take all antibiotics as prescribed Shower after contact sports or working out at a gym Tuberculosis Organism- Mycobacterium bacteria Diagnostic test- sputum culture, TB test, or CXR Symptoms: prolonged productive cough, hemoptysis (blood stained sputum), fever, chills, night sweats Transmission: cough/speak/sneeze (airborne) Site of infection: Lung most common, can spread to other organs Diagnostics: Mantoux test, CXR, sputum culture (5mm of induration Mantoux test +) Treatment: rifampicin, isoniazid, 6-12 months for treatment Prevention: immunization for children, isolation of client, teach client to cover nose/mouth when sneezing and coughing Streptococcal Infection Strep Throat Streptococcal bacterial infection to the pharynx, sometimes to the pharynx, sometimes the larynx and tonsils Transmission: close contact Incubation: 2-5 days Signs and Symptoms Severe sore throat Fever Yellow/white patches in the back of the throat Difficulty swallowing Dx: Rapid strep test or culture Treatment Ibuprofen or Tylenol for fever No aspirin for kids Oral or IM penicillin Complications Scarlet fever Fever- rash 12-48 hours after fever Strawberry red tongue Sore throat Dx: blood work, throat culture may + for strep Treatment: same as strep Acute rheumatic fever- heart disease Glomerulonephritis- kidney failure, antibodies against Strep lodge in the kidney Hepatitis A Patho: liver inflammation from the Hepatitis A virus Most common of the three: A, B, C 1 in 3 people in the US have been exposed, have the antibody, did not get sick Virus found in infected person’s stool Transmission: improper hand washing and handling of food Symptoms: N/V/D, low grade fever, jaundice, urine dark brown color Dx: antibody test, liver function test Treatment: no treatment, will resolve. If exposed may take immune globulin Hepatitis B Patho: inflammation of the liver by the Hepatitis B virus 350,000 in the US are chronic carriers 250,000 die each year Blood borne virus, exchange of body fluids Dx: liver function test, blood test Treatment: hydration, anti-viral, Interferon Infection Control Prevention of the spread of organisms Aseptic technique during procedures Standard precautions Hand washing Urinary bags below the bladder at all times Encourage to turn, deep breathe, and cough Tier 1 Universal Precautions Tier 2 Transmission based precautions Airborne precautions Measles Varicella Tuberculosis Droplet precautions Meningitis Pneumonia Epiglottitis Sepsis Diphtheria Pertussis Mumps Rubella Contact precautions MRSA E Coli Shigellosis Hep A RSV Herpes Isolation Principles Touches floor- clean it or get a new one Items brought into isolation must stay in the room Don’t touch your face or eyes when in a room Hand washing Keep water pitcher and cups in the room Immunizations (per Peds book) 2 months- Dtap , Hib, IPV, Pneumococcal, Hep B 15 months- Hep B, DTap, Hib, IPV, MMR, Varicella, PCV, Influenza, Hep A 4-6 years- Dtap, IPV, MMR, MpSV4 , PPV, Influenza, Hep A Dtap- Diphtheria, Pertussis, Tetanus Hib- Influenza group b IPV- polio MMR- Measles, mumps, rubella Varicella- chicken pox PCV- pneumonia carinii MPSV4- meningitis