Diving Medicine
advertisement
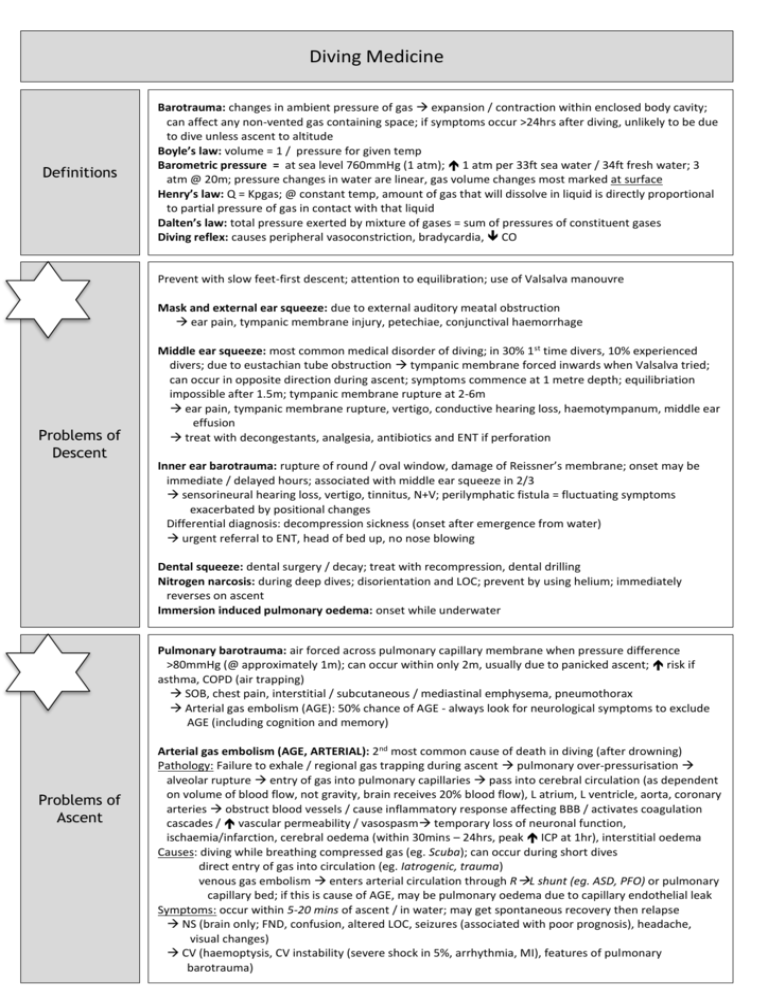
Diving Medicine Definitions Barotrauma: changes in ambient pressure of gas expansion / contraction within enclosed body cavity; can affect any non-vented gas containing space; if symptoms occur >24hrs after diving, unlikely to be due to dive unless ascent to altitude Boyle’s law: volume = 1 / pressure for given temp Barometric pressure = at sea level 760mmHg (1 atm); 1 atm per 33ft sea water / 34ft fresh water; 3 atm @ 20m; pressure changes in water are linear, gas volume changes most marked at surface Henry’s law: Q = Kpgas; @ constant temp, amount of gas that will dissolve in liquid is directly proportional to partial pressure of gas in contact with that liquid Dalten’s law: total pressure exerted by mixture of gases = sum of pressures of constituent gases Diving reflex: causes peripheral vasoconstriction, bradycardia, CO Prevent with slow feet-first descent; attention to equilibration; use of Valsalva manouvre Mask and external ear squeeze: due to external auditory meatal obstruction ear pain, tympanic membrane injury, petechiae, conjunctival haemorrhage Problems of Descent Middle ear squeeze: most common medical disorder of diving; in 30% 1st time divers, 10% experienced divers; due to eustachian tube obstruction tympanic membrane forced inwards when Valsalva tried; can occur in opposite direction during ascent; symptoms commence at 1 metre depth; equilibriation impossible after 1.5m; tympanic membrane rupture at 2-6m ear pain, tympanic membrane rupture, vertigo, conductive hearing loss, haemotympanum, middle ear effusion treat with decongestants, analgesia, antibiotics and ENT if perforation Inner ear barotrauma: rupture of round / oval window, damage of Reissner’s membrane; onset may be immediate / delayed hours; associated with middle ear squeeze in 2/3 sensorineural hearing loss, vertigo, tinnitus, N+V; perilymphatic fistula = fluctuating symptoms exacerbated by positional changes Differential diagnosis: decompression sickness (onset after emergence from water) urgent referral to ENT, head of bed up, no nose blowing Dental squeeze: dental surgery / decay; treat with recompression, dental drilling Nitrogen narcosis: during deep dives; disorientation and LOC; prevent by using helium; immediately reverses on ascent Immersion induced pulmonary oedema: onset while underwater Pulmonary barotrauma: air forced across pulmonary capillary membrane when pressure difference >80mmHg (@ approximately 1m); can occur within only 2m, usually due to panicked ascent; risk if asthma, COPD (air trapping) SOB, chest pain, interstitial / subcutaneous / mediastinal emphysema, pneumothorax Arterial gas embolism (AGE): 50% chance of AGE - always look for neurological symptoms to exclude AGE (including cognition and memory) Problems of Ascent Arterial gas embolism (AGE, ARTERIAL): 2nd most common cause of death in diving (after drowning) Pathology: Failure to exhale / regional gas trapping during ascent pulmonary over-pressurisation alveolar rupture entry of gas into pulmonary capillaries pass into cerebral circulation (as dependent on volume of blood flow, not gravity, brain receives 20% blood flow), L atrium, L ventricle, aorta, coronary arteries obstruct blood vessels / cause inflammatory response affecting BBB / activates coagulation cascades / vascular permeability / vasospasm temporary loss of neuronal function, ischaemia/infarction, cerebral oedema (within 30mins – 24hrs, peak ICP at 1hr), interstitial oedema Causes: diving while breathing compressed gas (eg. Scuba); can occur during short dives direct entry of gas into circulation (eg. Iatrogenic, trauma) venous gas embolism enters arterial circulation through RL shunt (eg. ASD, PFO) or pulmonary capillary bed; if this is cause of AGE, may be pulmonary oedema due to capillary endothelial leak Symptoms: occur within 5-20 mins of ascent / in water; may get spontaneous recovery then relapse NS (brain only; FND, confusion, altered LOC, seizures (associated with poor prognosis), headache, visual changes) CV (haemoptysis, CV instability (severe shock in 5%, arrhythmia, MI), features of pulmonary barotrauma) Investigations: Diagnosis is clinical; CXR may show intravascular air, CT/MRI may show changes, CK may be marker of severity, degree of haemoconcentration, marker of neurological outcome Problems of Ascent (cntd) Sinus squeeze: less common than ear; usually frontal / maxillary; facial pain; epistaxis on ascent, infraorbital nerve paraesthesia; treat with decongestants, valsalva Alternobaric vertigo: unequal ear equalisation; vertigo during ascent (can occur on descent), duration secsmins; no hearing loss Shallow water blackout: syncope secondary to hypoxia after hyperventilating off CO2; LOC during ascent Decompression illness = decompression sickness or AGE Decompression Illness / Sickness Decompression sickness (DCS, VENOUS): injury due to bubble formation in blood and tissues; incidence in recreational scuba divers 2-3/10,000 dives Risk factors = obese, smoker, ETOH, exercise, cold, dehydration, previous joint injury, old, binge drinking night before, other medical illness, female, aerobic capacity, local physical injury; dive duration / depth (>18 metres), multiple dives, rate of ascent, no decompression stops, ascent to altitude soon after diving, cold water Pathology: inert gas (especially nitrogen) dissolved dissolved nitrogen forms bubbles on ascent (in veins, lymphatics, tissues) tissue injury by same mechanism as AGE lungs act as filter (off-gassing), preventing bubble entry to systemic circulation symptoms occur if: pulmonary circulation overwhelmed (usually self limiting but indicates large bubble load) RL shunt (eg. PFO, ASD) AGE Pulmonary barotrauma so severe that bubbles enter pulmonary circulation Symptoms: onset may be delayed - 50% onset within 1 hour, 90% within 6 hours (occasionally longer); may be progressive, stable, relapsing and remitting, minor, Severe Type I (non-systemic, musculoskeletal): joint pain, rash (skin marbling; usually resolves in 12-24hrs), itching; maybe transient symptoms, poorly localised; may be no signs of inflammation; most common shoulder / elbow / knees; usually single joint; relieved by pressure Type II (neurological / systemic): affects NS (SC (in 60%) or CNS) NS: starts with feeling of truncal constriction numb feet, dizziness, weakness, gait probs, ascending paralysis, autonomic; maybe patchy and multiple sites; spinal cord symptoms, distended bladder; poor prognosis if sphincter involvement / psychiatric; associated with aching pain Vestibular (the staggers): symptoms after emergence (as opposed to inner ear barotrauma) vertigo, nystagmus, tinnitus, N+V Pulmonary (the chokes): rare; due to massive pulmonary gas embolism CP, cough, SOB, haemoptysis, CV collapse Type III: DCS + AGE = type II + stroke symptoms Supine position (no leg elevation; head down position may gas bubbles to coronary arteries) B: 100% O2 (even if not hypoxic; enhances inert gas elimination and bubble resolution, symptoms may resolve but frequently recur) C: IVF (maintain hydration to prevent 2Y ischaemic insult, avoid dextrose as may worsen neurological injury); Treat arrhythmias (usually refractory to standard treatment) D: Mannitol if impending cerebral herniation E: Transport at sea level (or at least <1000ft or pressurised aircraft) Lignocaine may improve outcome if treatment delayed (give for 48 hours) Not useful: anticoagulation ( risk of spinal cord haemorrhage), steroids, aspirin Management Hyperbaric Oxygen: 100% O2 at 2.8atm (18m, p O2 2000mmHg, 13x room air); usually require 1-2 treatment of 1 hour; early in type I, immediate in type II; reduces bubble volume, promotes nitrogen reabsorption and excretion, inhibits secondary inflammation and reperfusion injury, improves oxygenation of tissue, reduces ICP, improves brain metabolism; effectiveness in barotrauma strongly supported by research; place chest drain 1st if pneumothorax; early treatment = better outcome; requires close neurological monitoring in chamber; NSAIDs may number of sessions needed Indications: decompression illness / AGE: if any symptoms (even if become asymptomatic with 1st aid) and no contraindications; best if started within 72 hours; 55% resolve with 1 treatment, 75% with all treatments; if symptoms not responding significantly within 10-20 minutes, go deeper/longer; extend treatment if symptom recurrence during treatment CO poisoning: COHb >20, CV / NS signs; lower threshold if respiratory disease / pregnancy Other: cyanide, H2S, CCl4, clostridial infection Side Effects: O2 toxicity (formation of O2 free radicals cerebral toxicity (muscle twitching, apprehension, vertigo, visual problems, nausea, confusion, dizziness, seizures), pulmonary toxicity (cough, retrosternal pain, vital capacity); middle ear barotrauma, claustrophobia Prognosis Decompression Sickness: complete recovery possible despite severe symptoms; residual deficit 25% (more likely if delayed treatment); worse outcome if spinal cord symptoms Flying after diving: delay at least 12 hours after single non-decompression dive At least 18 hours after multiple dives / multiple days of diving >>18 hours for any decompression dives At least 1/52 if treatment for decompression illness More diving: congestion of tympani membrane 1-3/7 off diving Tympanic membrane haemorrhage 1/52 off diving Haemotympanum 6/52 off diving