File - CCFP-EM
advertisement
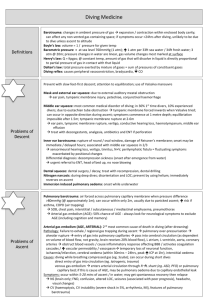
Decompression Illness & Barotrauma Richard Dionne MD Emergency Medicine – University of Ottawa March 2013 Decompression Illness & Barotrauma • Goals & Objectives • Comprehensive understanding of Boyle’s Law, Henry’s Law and Dalton’s Law of physics… • Comprehensive understanding of Dysbarism • Discuss the clinical presentation, prevention and interventions in DCI type 1 & 2 • Discuss the principles of Barotrauma and the principles of Hyperbarics • Discuss a differential diagnosis based on history alone Diving injuries Group of illnesses resulting from pressure changes… • Barotrauma • POPS • Alternobaric vertigo (ABV) • Decompressions Illness (DCI): – Decompression Sickness (DCS type 1 & 2) – Arterial Gas Embolism (AGE) – Nitrogen Narcosis Question Most of the diving injury related deaths are secondary to: a) Barodontalgia b) Stroke from an Arterial Gas Embolus c) Drowning d) Bends e) DCS type II Question Most of the diving injury related deaths are secondary to: a) Barodontalgia b) Stroke from an Arterial Gas Embolus c) Drowning d) Bends e) DCS type II Case A 25 y/o male taking his first SCUBA lesson at a local pool Once down at the bottom of the pool, he ascends in a panic … He starts feeling short of breath, coughing, & he mentions that he coughed up a little bit of blood... Barotrauma Going up or down? Name that Law! With depth ↑ pressure & ↓ gas volume… Boyle’s Law • Twice the pressure = ½ the volume • Holding breath during ascent = pulmonary barotrauma Boyle’s Law • Problem : Over pressurization on ascent Boyle’s Law • Tissue damage results when gas-filled space does not equalize its space with external pressure… Boyle’s Law • PV=K … or … P1V1 = P2V2 • P=pressure / V=volume / K= constant • As pressure increases/ decreases, volume decreases / increases Ottawa Base Hospital Program Boyle’s Law • PV = K • Physiology: – Sea level – Altitude 18 000 feet – Diving 33 feet – Diving 66 feet 1 Atm = volume gas 0,5 Atm = 2 X vol. gas 2 Atm = ½ X vol. gas 3 ATA = ⅓ X vol. gas Pulmonary Barotrauma • Closed glottis (no expiration) when surfaces… • Pneumothorax / Pneumomediastinum – “POPS” pulmonary over pressurization syndrome – Occurs at low depth (10 feet) • Arterial Gaseous Embolism ? – No, usually deeper and longer – Have to dissolve gas for this to occur Descent Barotrauma (Squeeze) • Compression of gas in enclosed space – – – – – Mask Squeeze Ear & Sinuses Lungs & airways GI tract Recent dental extraction, sockets / fillings • Severe, sharp pain, edema or hemorrhage Ear Barotrauma • Middle ear – Tympanic rupture / hemorrhage / vertigo • Internal ear – Round or oval window rupture with perilymph fistula – Hearing loss / tinnitus / vertigo etc. • Alternobaric Vertigo (ABV) – Change in pressure labyrinthe on ascent – Vertigo / nausea / vomiting / hearing loss Middle Ear Internal Ear Treatment • Pseudoephedrine pills or nasal spray – Prophylaxis before dive (60 mg) – No dive if < 2 weeks from URTI – Frenzel maneuver • Suspect Internal Ear Barotrauma – No Valsalva / no diving – Decongestant & NSAIDS for pain – Antibiotic prophylaxis if tympanic perforation – Consider Prednisone for Teed 3-4 – ENT consult & audiogram: urgent Teed 5 Tympanic Membrane : TEED Scale Teed 1 congestion around umbo Teed 2 congestion of entire TM Teed 3 Hemorrhage in middle ear Teed 4 Extensive middle ear hemorrhage with blood bubbles / TM rupture Teed 5 Entire middle ear is filled with dark deoxygenated blood Question Active divers can have a progressive hearing loss in the 4000 – 8000 Hz range. (Which is otherwise known as the “spouse’s voice” range…) a) True b) False Question Active divers can have a progressive hearing loss in the 4000 – 8000 Hz range. (Which is otherwise known as the “spouse’s voice” range…) a) True b)False Cochlea Decompression Illness (DCI) Decompression Sickness Type I & II Arterial Gas Embolism Case • 22 y/o recreational diver lost consciousness while ascending • Within 30 sec. started coughing pink, frothy sputum • The diver has left lung field diminished air entry… Complaints of left sided numbness … Question Which treatment is not indicated in primary care of a diving injury? a) Aspirin b) Trendelenburg position c) 100 % Oxygen d) IV fluids Question Which treatment is not indicated in primary care of a diving injury? a) Aspirin b)Trendelenburg position c) 100 % Oxygen d) IV fluids Dysbarism 1. Change volume / pressure in compartments containing gases … 2. partial pressure of dissolved gas… 3. Gas bubble formation in tissue & blood system … 4. CNS system changes with pressure Arterial Gaseous Embolism Air bubble forced through alveolar-capillary membrane and into circulation … distal embolism : limb / cerebral / coronary / etc. Presentation : < 10 min. in 90% Pulmonary symptoms in 25%-50% Treatment : Hyperbaric Chamber ... Arterial Gaseous Embolism • Expanding air on ascent forces air bubbles through alveolarcapillary membrane into circulation • Location, Location, Location – Distal embolism: limb / cerebral / coronary etc. • 90 % of pt’s present in < 10 min from surfacing • Pulmonary symptoms in 25 – 50 % • Major cause of death & disability among divers Nitrogen bubbles The formation of bubbles can harm the body by: a) b) c) d) Blocking vessels Causing localized swelling Tearing and rupturing vessels All of the above Nitrogen bubbles The formation of bubbles can harm the body by: a) b) c) d) Blocking vessels Causing localized swelling Tearing and rupturing vessels All of the above Physiology Dalton ’s Law... Pt = PO2 + PN2 + Px Total pressure exerted by a mixture of gases is equal to the sum of the partial pressure of each of the component gases… Henry ’s Law... Cx = Px X solubility Amount of gas that will disolve in a solution is directly proportionnal to the partial pressure of that gas… Increase partial pressure = more gas dissolved Decrease partial pressure = gas coming out of the solution Henry’s Law Solubility of a gas is directly proportional to the pressure exerted on this gas … Some gases have different solubility at different pressures ... • Problem: – Nitrogen is dissolved in tissues on descent, but needs to be released gradually on ascent. If too rapid, it stays trapped and forms gas bubbles within the tissue and bloodstream. Case • Sunday evening you are called for a 28 y/o with paresis & paresthesias both legs … • Gradual onset for the last 12-18h… • Patient has voiding difficulty… • Mentions a light headache, dizziness with joint pains… • He asks you could this be related to his dive 24hrs before? ? History • • • • • • • • Depth and length of dive ? Decompression stop times ? Dive computer used ? How many dives in last 72 hrs ? Delay from last dive to air travel ? Symptoms on descent or ascent ? Symptoms at surfacing or delayed ? Please remember to bring the equipment… Decompression Sickness «Pathophysiology» Nitrogen gas bubbles formation in tissue and vascular system … during ascent ... Increase in Nitrogen concentration in tissues as dive prolongs … Bubbles are formed as you surface Mecanical obstruction from bubbles Promotes platelet aggregation & thrombosis Nitrogen is liposoluble … CNS fragility Decompression Sickness (DCS) • 95% symptomatic < 24 h ... • DCS type I – « Bends » – Polyarticular pains / skin tightness • DCS type II – neurological & cardiovascular symptoms – headache / diplopia / confusion / ataxia / CVA / seizure / paresthesia / para-paresis (T12-L1…)) Decompression Sickness Recompression & 100% oxygen helps DCS by: a) b) c) d) Mechanically compressing bubbles Washing nitrogen out of the tissues Reducing swelling All of the above Decompression Sickness Recompression & 100% oxygen helps DCS by: a) b) c) d) Mechanically compressing bubbles Washing nitrogen out of the tissues Reducing swelling All of the above Decompression Sickness • Even in lower altitude – Commercial planes pressurized at 5000 ft • Plane after diving… – 12 hr after dive (< 2 hr) in last 48 hr – If multiple dives / unlimited … suggest 24 – 48 hr • Plane or diving after DCS – Type 1: after 7 days – Type 2: after 4 weeks Question Is it safe to fly a Decompression Illness patient, if the pilot maintains an altitude of less than 500 ft (152 m) above the departure point. a) True b) False Question Is it safe to fly a Decompression Illness patient, if the pilot maintains an altitude of less than 500 ft (152 m) above the departure point. a) True b) False Gas Toxicity Nitrogen Narcosis Diving breathing gas mixtures • Compressed air (common for dives < 130 feet) – Nitrogen (78%), Oxygen (21%), gases (1%) • Nitrox – mixture of oxygen (more than 21%) & air – Accelerates decompression – Decrease risk of DCS • Trimix – mixture of oxygen, nitrogen & helium – Technical / commercial diving at depth – Reduces nitrogen narcosis • Heliox, Heliair, Hydreliox, Neox … Nitrogen • Theoretical models help predict rate of nitrogen absorption • DCS can happen even in a perfectly planned dive • Absorption rate depends on: – Nitrogen partial pressure – Tissue perfusion – Tissue fat content Nitrogen Narcosis • Rapture of the deep • Deep or prolonged dive • Symptoms – Euphoria / Confusion / Disorientation – Change in judgement – Impaired motor function & Paresthesia Question Nitrogen is 5 x more soluble in fat tissue. That is why women are at increased risk for Decompression Sickness involving the Central Nervous System. a) True b) False Question Nitrogen is 5 x more soluble in fat tissue. That is why women are at increased risk for Decompression Sickness involving the Central Nervous System. a) True b) False Nitrogen Narcosis Treatment • • • • • • 100 % Oxygen Position: No trendelenburg ASA PO IV fluids Prevent hypothermia Hyperbaric Oxygen Toxicity • Breathing Oxygen enriched gases (ex. Nitrox) • Once the alveolar PO2 rises above a critical level • ↑ PO2 increase… ↑ toxicity • Hemoglobin-oxygen buffering mechanism fails • Brain is most sensitive to high oxygen pressure • Oxygen free radicals toxins • Seizures (at depth), nausea, dizziness, visual disturbances, disorientation … ARDS… Differential & Treatment Possible just with the history ! History • Depth and length of dive ? • Decompression stop times ? • Dive computer used ? • How many dives in last 72 hrs ? • Delay from last dive to air travel ? • Symptoms on descent or ascent ? • Symptoms at surfacing or delayed ? • Please remember to bring the equipment… Differential Rosen’s 5th Ed. P. 2027 Figure 137-2 Onset of symptoms? Descent Depth Middle Ear Barotrauma Internal Ear Barotrauma Facial Barotrauma Sinus Barotrauma Nitrogen Narcosis Hypothermia Contamination Oxygen toxicity Ascent Rapid Ascent ABV POPS AGE Pneumothorax Pneumomediastinum Pulmonary hemorrhage GI & Dental barotrauma Long / Deep Dive Profile DCS 1 & II Hyperbaric Chamber • Arterial gas embolism & Decompression Sickness • AGE , DCS • U.S. Navy Protocols… Table 5 & 6 • General protocol is: – Wear 100% cotton (highly flammable environ.) – Dive to 2.5 ATM (50 feet) – 3 – 30 min sessions in 100 % oxygen – 10 min air / breaks to prevent oxygen toxicity – 5 treatments usual, but more according to dx Hyperbaric Chamber … Diving Injuries Barotrauma Mask squeeze & Barosinusitis Middle & Internal Ear Barotrauma ABV - Alternobaric vertigo Pulmonary Barotrauma Intestinal Barotrauma Dysbarism Decompression Sickness : type I & II Arterial Gaseous Embolism Nitrogen Narcosis Take home ... History is very important … Increase in sport scuba divers ... Trendelenburg may increase risk of elevated ICP & coronary embolus = not indicated… Most diving injuries are self-limited … A.G.E. / D.C.S. I & II = « Hyperbaric » Aware of closest «Hyperbaric Facility» Take home ... History is very important … Increase in sport scuba divers ... Trendelenburg may increase risk of elevated ICP & coronary embolus = not indicated… Most diving injuries are self-limited … A.G.E. / D.C.S. I & II = « Hyperbaric » Aware of closest «Hyperbaric Facility» Questions ? Ottawa Base Hospital Program Want more? • DAN: – www.diversalertnetwork.org – Emergency Hotline (919) 684-8111 – Non-emergency (919) 684-2948 • Undersea & Hyperbaric Medicine • Wilderness & Environmental Medicine Submersion Injuries Richard Dionne MD Emergency Medicine – University of Ottawa March 2013 Case A 4 yr old boy is found face flat semi-floating in the pool, after his mother heard screaming from his older sister… What do we need to know ? Pathophysiology Laryngospasm Wet Drowning Dry Drowning 80% 20% Hypoxemia Acidosis End organ damage Cardiac Arrest Near Drowning Fresh water Salt water No difference Surfactant is destroyed Alveolar instability Atelectasis & Compliance & Bronchospasm V/Q mismatch Hypoxia Drowning / Near drowning Drowning : is defined as death 2nd to asphyxia while immersed in a liquid within 24h of the submersion. Near Drowning: is defined as immersion episode of sufficient severity to warrant medical attention, with potential morbidity or mortality. Drowning is 2nd to MVA as cause of Death in children Submersion Outcome in Children 35% fatal 11% severe neurologic sequelae 33% some degree of CNS damage Protecting Factors Diving reflex Hypothermia Rescucitation & CPR within 10 minutes Factors Bad Prognosis No consensus / No proven scale Examples … Delay in CPR > 10 min. Severe acidosis Coma in ED Asystole in ED Fixed dilated pupils Hyperkalemia > 10 mmol/L R/o Associated Causes Trauma ( C-spine) Child abuse (bathtubs) Suicide & Homicide Myocardial Infarction & Cardiac Arrest Dysbarism Seizure disorder Diabetes & Hypoglycemia Substance abuse & poor judgment Hypothermia Complications Pulmonary Injury Secondary Drowning « ARDS» Secondary infection CNS Injury Primary & Secondary Acute Tubular Necrosis Secondary to Hypoxemia & Acidosis Hypothermia Cardiac Dysrythmias Case Young 19 yr old male just broke up with his girlfriend at the city pool. He does not know how to swim and decides to throw himself in the water. He goes down and after a few minutes he is taken out. He swallowed a lot of water, vomited, is coughing and wheezing. When is it safe to discharge ? Asymptomatic Normal Chest X-Ray Normal Blood Gas Normal Renal function Sat.> 95% & 6 - 8 hr of observation Caution : asymptomatic can still be hypoxic Management Aggressive respiratory treatment CPaP / Bi-PaP / 100% O2 Early intubation if Hypoxia persists pO2 < 70 mmHg or < 80 mmHg child with 100% O2 face mask… Address Bronchospasm & ARDS Address Hypothermia… Prevention Children supervision CPR courses to families with pools Boating sobber & lifevests Diving injuries Caution: CAD / Seizure / Diabetics Take Home ... Global hypoxic-ishemic event involving brain, lungs and heart … No difference Fresh or Salt water ... No prognostic scale is accurate to predict outcome ... Aggressive pulmonary support ... Take Home ... Global hypoxic-ishemic event involving brain, lungs and heart … No difference Fresh or Salt water ... No prognostic scale is accurate to predict outcome ... Aggressive pulmonary support ... Thank you !!! Ottawa Base Hospital Program