18. Auditory – Kaylie. CBI206 – 2014
advertisement

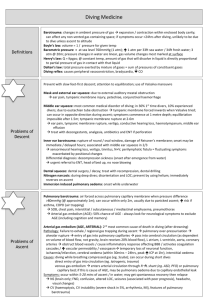
Otologic Manifestations of Barotrauma David M. Kaylie, MD FACS Otolaryngology – Head and Neck Surgery ENT Manifestations of Barotrauma • • • • EAC squeeze Sinus squeeze Mask squeeze Middle Ear Barotrauma Elastic Cavity • The pressure of a gas is inversely proportional to volume at constant temperature • Boyle’s law P1V1=P2V2 1 atm surface 2 atm 10 m 4 atm 30 m Inelastic Cavity • Constant volume • Pressure changes 1 atm surface 33ft 4 atm 30 m Cavities Surface 1 atm 3 ATM Lungs (elastic) 33ft Bony Cavity (inelastic)) 4 atm 132 ft Changing Pressure • 33 feet of seawater (fsw)=1 atmosphere pressure (14.7 psi) • Balloon (or Lungs) at surface – If pressure is 3x, volume is 1/3 and density is 3x – When breathe at depth, gas at higher pressure than surface – If hold breath as resurface • Volume expands and lungs overinflate. – DON’T HOLD BREATH External Ear Canal Squeeze • • • • • Hood Cerumen Plug Elderly Congenital small ear canals • Swimmers (Surfers) Ear → Exostoses Exostoses • Cold water exposure • Benign • Trap cerumen Osteoma External Ear Canal Barotrauma Inside: Hemotympanum and Hemorrhage of Ear Canal Skin 1 Month: Exfoliation 6 Weeks: Otitis Externa Treatment of EAC Barotrauma • Dry ear precautions x 6 weeks (cotton/vas) • Topical antibiotic/steroid drops (Ciprodex) • Oral antibiotics if cellulitis (amox/clav) • Wick if obstructed (merocel) • Analgesia Barosinusitis • Descent 68%, Ascent 32% (Fagan 1976) • Pain • Nosebleed Barosinusitis • Frontal > maxillary > ethmoid • Blindness and meningitis (Parell and Becker, 2000) Treatment of Barosinusitis • • • • • • • Elevate head Heat Oxymetazoline (Afrin) Pseudoephedrine (Sudafed) Avoid antihistamine – not beneficial Antibiotics for secondary bacterial infection Analgesia Middle Ear Barotrauma • Most common medical condition of divers – Occurs mainly on descent – Symptoms- pain, conductive hearing loss – Signs- hemotympanum, perforation MEBT • 4 fsw pressure > tensor tympani strength • 10–69 fsw Dimeric TM rupture – Keller, 1958 – Jensen, 1993 Normal Ear Canal and TM Acute Hemotympanum Resolving Hemotympanum Perforation Management of MEBT • • • • Usually resolves without treatment Oxymetazoline < 1 wk Antibiotics in advanced cases No diving until sx free, normal TM and able to autoinflate x 3 mo. Equalizing General Recommendations • Avoid diving with URI, allergies • Avoid medications causing nasal congestion (turbinate ↑) • Antihypertensives • BPH (Hytrin) • ED (Viagra) • Descent feet first • Autoinflate 1-2 ft. No pain is acceptable Equalizing Techniques • Swallow, jaw thrust • pseudoValsalva: – Alar balloon • Lowry: – pValsalva+swallow • Edmonds: – pValsalva+jaw thrust Other Equalizing Techniques Courtesy Allen Dekelboum, MD • Toynbee: – Swallow with mouth and nose closed – Good for ascent • Frenzel: – pValsalva with throat contraction • Neck twitch: – Sudden lateral motion with nose closed Equalizing Middle Ear: Managing Difficult Cases • Dry land practice • Anchor line – helps control decompression stop in rough water • Private lesson • No bouncing • Medication Medication for Eustachian Tube Dysfunction • • • • Otolaryngology examination Rarely: Allergy, Septum, CT or MRI Topical nasal steroid Afrin 12 hour • Rebound • Sudafed 120 mg ER • Cardiac, High blood pressure, Urinary retention • Oral corticosteroids (prednisone, medrol) • Diabetes, Peptic ulcer, GERD, Infection, CNS, +++ TMJ • • • • • 25 – 65% of SCUBA divers Sea Cure Right Bite Custom mouth piece Check hose length Otolaryngology clearance to dive • Normal examination, able to auto inflate • Diving with ENT disorders – Meniere’s disease (1 year rule, asymmetrical C°) – Prior IEBT (hearing loss, vertigo) – S/P Surgery • • • • • • • • Tympanoplasty Mastoidectomy Ossiculoplasty Stapedotomy Cochlear Implant Acoustic Neuroma ESS Laryngeal surgery (C°) (C°) (C°) Meniere’s Disease • Spontaneous vertigo at depth • Emphasize risk of aspiration, death • One year symptom free without treatment chamber/rescue diver • Simultaneous (C°) Dive with perforation/cavity • Pro Ear 2000 Dive with perforation Dive with perforation/cavity • Dry Hood Diving After Ear Surgery • • • • • • Tympanoplasty PORP TORP Cochlear Implant PLF Acoustic neuroma 3 months yes +/3 atm (device 4 atm) +/No Dive after Sinus Surgery • -6 weeks • -Healed ostia Practical Approach to Stings • Hot water (as tolerated, 110°) • Ammonia, alcohol, papain, peroxide • Vibrio vulnificus – gram negative – Ceftriaxone, Cipro, Septra, Doxycycline The Dizzy Diver Differential • • • • • • • Hangover Motion sickness Disembarkment Diving disorders Heart Circulation CNS, Endocrine Motion Sickness • Mechanism: sensory mismatch (adaptation) – Yaw (0.2 Hz) vertical linear motion – Susceptibility: Ages: 2- 10; 40-50 • Non-pharmacologic therapy – Sea Band (P6, Nei Kuan point) • = placebo • Some studies show it works MEDICAL TREATMENT OF MOTION SICKNESS • Pharmacologic therapy – Diminhydrinate (50-100mg) antihistamine 2hrs 8hrs (25 mg) antihistamine 2hrs 6hrs (25-50mg) phenothiazine 2hrs 18hr (0.5 mg) antimuscarinic 8hrs anticholinergic 72hr drowsy – Meclizine drowsy – Promethazine drowsy – Scopolamine drowsy – D-amphetamine (5-10mg) amphetamine 1hr abuse, palpitation, HBP, arrhythmia, psychosis, insomnia, euphoria, use in pregnancy, MAOI, hyperthyroid 6hr Disembarkment Syndrome (Mal de debarquement) • Tal (2005) – – – – – Swaying, swinging, unsteadiness after return to land Symptoms appear after landing Associated with sea sickness while onboard No objective measures available Mostly women • Hain (1999) – 26 of 27 women (age = 49.3) – Duration 3.5 years – Treatment • • • • Meclizine Scopolamine Vestibular rehab Benzodiazapines + Diving Disorders Causing Dizziness •Four categories of IEBT –During compression –At Stable Depths –During decompression –Noise trauma Diving Disorders Causing Dizziness •Inner ear barotrauma •Perilymph fistula •Inner ear DCI •Alternobaric vertigo •Gas toxicity •Isobaric counter-diffusion INNER EAR BAROTRAUMA (IEBT) • Usually with MEBT • Cochlear 90%, Vestibular 60%, Both 50% (Molvaer, 1988) • Mechanism – Forced inflation on descent – Sudden equilibration – TM snaps, pressure wave from stapes to RWM Oval and Round Windows • Sudden insufflation of middle ear snaps TM laterally, displacing stapes laterally and RW medially. Incidence of IEBT • 76 of 15,000 (0.5%) logged dives – Molvaer (1988) • 26 of 319 (8%) patients with dive-ENT disorders – Klingmann (2006) Recurrent IEBT • Israel Naval Medical Institute – 2 of 44 (5%) of IEBT seen in 18 years (Shupak, 2006) Treatment of IEBT • Bed rest, head elevated • Control B.P., discontinue aspirin • Prednisone • Observe (dial tone, etc.), serial audio • Explore if strong suspicion of PLF PERILYMPH FISTULA MECHANISM: - RWM or OW ligament - Implosion - Explosion Rupture on descent Symptoms on ascent gas from ME to IE (Molvaer, 1988) Perilymph Fistula • Increased CSF pressure without equilibration = OW • Sudden forced insufflation with snap of TM = OW or RW PERILYMPH FISTULA • Pneumolabyrinth PERILYMPH FISTULA TREATMENT: 1. Bedrest, head elevated x 5d 2. Explore if SNHL progresses 3. Explore immediately if significant SNHL occurs with barotrauma 4. Explore vertigo > 5 days (normal MR and neuro) PERILYMPH FISTULA Middle ear exploration • 30 minutes • Local or G.A. PERILYMPH FISTULA INNER EAR DECOMPRESSION ILLNESS (IEDCI) • Any depth, any diver • More common in decompression diving – Dives >130 feet require special gas mixtures INNER EAR DECOMPRESSION ILLNESS (IEDCI) • Vertigo (most common), HL, tinnitus • Type II DCI – Associated with systemic DCI: spinal cord symptoms, pain, itching, rash, dyspnea, LOC, death – Inner ear: bubble formation → hemorrhage tissue rupture (Antonelli, 1993) Recurrent IEDCI • 5 of 24 IEDCI (21%) • Nachum (2001) • 2 of 18 IEDCI (11%) • Klingman (2006) Management of IEDCI • HBO, fluids, steroids, n-acetyl cysteine – HBO within 1 hr → 50% complete resolution – 5 hr → 10% – 10 hr → 22% • Do not dive for 3 months (Nachum, 2001) (Shupak, 2003) (Klingmann, 2006) (Molvaer, 2003) – Do not dive if SNHL, RVR persist? • Recompression with fistula safe – Guinea pigs – Human experience – Tubes (Stevens, 1991) (Dekelboum 2005; Klingmann 2004) Right to Left Shunt (PFO) • R/O PFO in patients with DCI – Right to left shunt in IEDCI 82% • in controls 25% (Cantais, 2003; Klingmann, 2006) – German Diving Medical Society—’Unfit to Dive’ ALTERNOBARIC VERTIGO • Asymmetric ME pressure Onset during ascent Duration up to 20 minutes (Lundgren, 1965) • Human study: 20 mm Hg asym→NYS (Henrickson, 1966) Incidence of Alternobaric Vertigo • 10% of Swedish divers (Lundgren, 1974) • 33% of Norwegian divers (n = 194) (Molvaer, 1988) • 14% sport divers (OME or ET) (Uzun, 2003) ASYMMETRIC CALORIC STIMULATION • Stimulus: – Unilateral EAC obstruction (cerumen, plug, hood, squeeze) – ME/Mastoid asymmetry (bone, OME, squeeze) • Response: – Compensated RVR GAS TOXICITY • Nitrogen narcosis (rapture) Dizziness, hallucination >100 feet • O² toxicity: Seizure, death VENTID (vision, ears, nausea, twitching, irritaion, death C0², CO contamination COUNTERDIFFUSION • Physiologic effect of diffusion of different gases in opposite directions under constant ambient pressure • Two gases with different diffusion and solubility coefficients – Rapidly diffusing gas moves into tissues – More soluble gas diffuses slower • Local supersaturation and bubbles • Occurs at perilymph/endolymph boundaries • Skin lesions and vertigo most common Counterdiffusion • Occurs in divers – Immersed in lighter rapidly diffusing gas (helium) – Breathes slower gas (neon or nitrogen) • Prevent by – Recompressing when switching from N to He rich mixes (other way around ok) – Avoiding helium rich gases for breathing when surrounded by nitrogen rich gases DIFFERENTIAL DIAGNOSIS DIAGNOSIS IEBT Fistula IEDCI Asymmetric caloric Alternobaric vertigo Gas toxicity Counter diffusion Hearing loss ++ + + +/- Onset Descent D/A Ascent Descent Ascent Stable Stable