Chapter 4 Skin and Body Membranes
advertisement
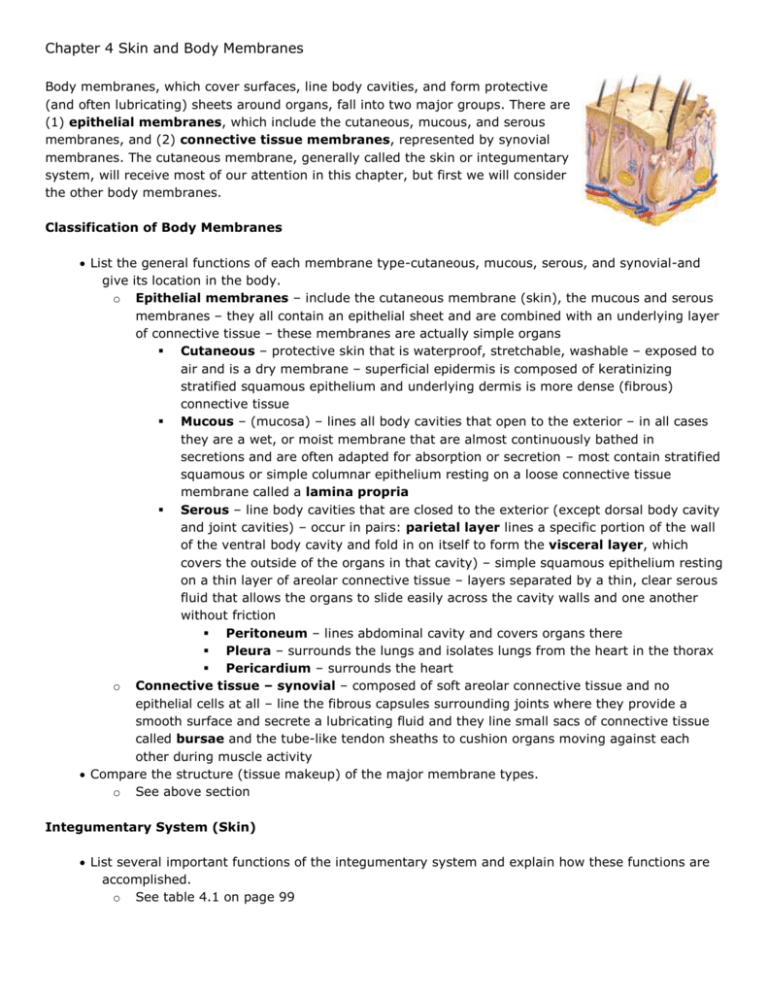
Chapter 4 Skin and Body Membranes Body membranes, which cover surfaces, line body cavities, and form protective (and often lubricating) sheets around organs, fall into two major groups. There are (1) epithelial membranes, which include the cutaneous, mucous, and serous membranes, and (2) connective tissue membranes, represented by synovial membranes. The cutaneous membrane, generally called the skin or integumentary system, will receive most of our attention in this chapter, but first we will consider the other body membranes. Classification of Body Membranes List the general functions of each membrane type-cutaneous, mucous, serous, and synovial-and give its location in the body. o Epithelial membranes – include the cutaneous membrane (skin), the mucous and serous membranes – they all contain an epithelial sheet and are combined with an underlying layer of connective tissue – these membranes are actually simple organs Cutaneous – protective skin that is waterproof, stretchable, washable – exposed to air and is a dry membrane – superficial epidermis is composed of keratinizing stratified squamous epithelium and underlying dermis is more dense (fibrous) connective tissue Mucous – (mucosa) – lines all body cavities that open to the exterior – in all cases they are a wet, or moist membrane that are almost continuously bathed in secretions and are often adapted for absorption or secretion – most contain stratified squamous or simple columnar epithelium resting on a loose connective tissue membrane called a lamina propria Serous – line body cavities that are closed to the exterior (except dorsal body cavity and joint cavities) – occur in pairs: parietal layer lines a specific portion of the wall of the ventral body cavity and fold in on itself to form the visceral layer, which covers the outside of the organs in that cavity) – simple squamous epithelium resting on a thin layer of areolar connective tissue – layers separated by a thin, clear serous fluid that allows the organs to slide easily across the cavity walls and one another without friction Peritoneum – lines abdominal cavity and covers organs there Pleura – surrounds the lungs and isolates lungs from the heart in the thorax Pericardium – surrounds the heart o Connective tissue – synovial – composed of soft areolar connective tissue and no epithelial cells at all – line the fibrous capsules surrounding joints where they provide a smooth surface and secrete a lubricating fluid and they line small sacs of connective tissue called bursae and the tube-like tendon sheaths to cushion organs moving against each other during muscle activity Compare the structure (tissue makeup) of the major membrane types. o See above section Integumentary System (Skin) List several important functions of the integumentary system and explain how these functions are accomplished. o See table 4.1 on page 99 When provided with a model or diagram of the skin, recognize and name the following skin structures: epidermis, dermis (papillary and reticular layers), hair and hair follicle, sebaceous gland, and sweat gland. o See diagrams 4.3 and 4.4 on pages 100 – 101 Name the layers of the epidermis and describe the characteristics of each. o Stratum basale – deepest layer lies closest to the dermis and receives adequate nourishment via diffusion from the dermis – constantly dividing and pushing daughter cells upward – also contains melanin pigment produced by melanocytes that functions to protect the skin from UV light from the sun o Stratum Spinosum o Stratum Granulosum o Stratum Lucidum – flatter, increasingly full of keratin and dead cells – occurs only where the skin is hairless and extra thick (palms of hands and soles of feet) o Stratum Corneum - shingle-like dead remnants, completely filled with keratin that prevents water loss and invasion from biological, chemical, and physical damage – flake off slowly and are replaced by cells from deeper layers Name the layers of the dermis and describe the characteristics of each o Papillary – upper region – uneven and has fingerlike projections from its superior surface called dermal papillae, which indent the epidermis above – may contain capillary loops or may contain pain receptors or touch receptors – form fingerprints – ridges of the fingertips are covered in sweat pores o Reticular – deepest layer that contains blood vessels, sweat glands and oil glands and deep pressure receptors called Pacinian corpuscles – phagocytes also are found here to kill bacteria o Both layers have collagen responsible for the toughness of the dermis which attract and bind water to keep the skin hydrated and elastic fibers that give the skin its elasticity – both decrease as we age along with the loss of fat from subcutaneous tissues causing wrinkles Describe the distribution and function of the epidermal derivatives-sebaceous glands, sweat glands, and hair. o Exocrine glands – release their secretions to the skin surface via ducts Sebaceous (oil) glands – found all over the skin, except palms and soles – ducts usually empty into a hair follicle while others open onto the skin surface Sebum – mix of oily substances and fragmented cells – lubricant that keeps the skin soft and moist and prevents the hair from becoming brittle – also contains chemicals that kill bacteria Sweat glands – widely distributed in the skin Eccrine glands – found all over the body – produce sweat, an acidic, clear secretion that is water, salts, vitamin C, lactic acid, traces of metabolic wastes such as ammonia, urea, uric acid – nerve endings cause them to secrete sweat which helps the body maintain a constant temperature Apocrine sweat glands – confined to the axillary and genital areas – larger than the eccrine glands and their duct empty into hair follicles – secretions contain fatty acids and proteins as well as the same substances as eccrine gland secretions – secretions are milky to yellowish and odorless except when bacteria are present – become active at puberty with no precise function known Hair – scattered all over the body – serve only minor protective functions – produced by a hair follicle Root – the part of the hair enclosed in the follicle Shaft – the part projecting from the surface of the scalp or skin Hair bulb matrix – growth zone where a hair is formed by division of the nourished stratum basale epithelium cells at the inferior end of the follicle Hair follicle – inner epidermal sheath composed of epithelial tissue and forms the hair, outer dermal sheath is dermal connective tissue that supplies the blood vessels and reinforces the epidermal part Arrector pili – smooth muscle cells that pull the hair upright and causes goose bumps and help keep the animal warm when air is trapped in the hairs Name the factors that determine skin color and describe the function of melanin. o Melanin – a pigment that ranges in color from yellow to brown to black – produced by melanocytes cells – when sunlight hits the skin, melanocytes are stimulated to produce melanin pigment causing a tan – the melanin is taken in by stratum basale cells and it forms a protective covering over the cell’s nucleus protecting the DNA from further UV damage o The color of skin depends on: The amount and kind of melanin in the epidermis The amount of carotene deposited in the stratum corneum and subcutaneous tissue The amount of oxygen bound to hemoglobin in the dermal blood vessels Differentiate between first-, second-, and third-degree burns. o First-degree – only the epidermis is damaged – area becomes red and swollen – sunburns – heal within a few days o Second-degree – partial-thickness burns – involve injury to the epidermis and the upper region of the dermis – blisters appear – regeneration is still possible but a scar may form o Third-degree – full-thickness burns – destroys the entire thickness of the skin – nerve endings are also destroyed therefore no pain – regeneration not possible requiring grafting Explain the importance of the "rule of nines." o Used to estimate the volume of fluid lost based on how much of the body surface is burned – body is divided into 11 areas, each accounting for 9 percent of the total body surface area, plus an additional area surrounding the genitals representing 1 percent of the body surface Summarize the characteristics of basal cell carcinoma, squamous cell carcinoma, and malignant melanoma. o Basal cell carcinoma – the least malignant and most common skin cancer and is slow growing and metastasis seldom occurs – cells of the stratum basale are altered so they cannot form keratin and no longer honor the boundary between epidermis and dermis – most often occur in sun-exposed areas o Squamous cell carcinoma – arises from cells of the stratum spinosum – lesion appears as a scaly, reddened papule that gradually forms a shallow ulcer with a firm, raised border – grows rapidly and metastasizes to adjacent lymph nodes if not removed o Malignant melanoma – cancer of melanocytes and can begin wherever there is pigment – appears as a spreading brown to black patch that metastasizes rapidly to surrounding lymph and blood vessels ABCD rule (A) asymmetry – two sides not equal (B) border irregularity – borders not smooth (C) color – spot contains different colors (D) diameter – larger than 6mm in diameter Developmental Aspects of Skin and Body Membranes List several examples of integumentary system aging. o During adolescence – skin and hair become more oily and acne may form o Skin reaches optimal appearance in 20s and 30s when it is thick, resilient, and well hydrated then it loses it elasticity and thins as aging occurs o During old age the amount of subcutaneous tissue decreases, which leads to intolerance to cold and drier skin, which may become itchy and bothersome – the thinning of the skin makes it more susceptible to bruising and other injuries – decreased elasticity along with decreasing subcutaneous fat allows bags under eyes and jowls to sag o Hair loses its luster with age and the number of follicles decreases resulting in baldness, or alopecia