Clinical Value Core Case Study
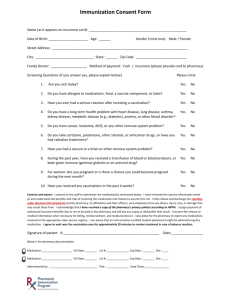
advertisement
HIMSS Davies Enterprise Application Submission Form Hilo Medical Center – Clinical Value Core Case Study --- Cover Page --Name of Applicant Organization: Organization’s Address: Submitter’s Name: Submitter’s Title: Submitter’s E-mail: Core Item: Hilo Medical Center 1190 Waianuenue Avenue, Hilo, HI 96720 Money Atwal CIO & CFO matwal@hhsc.org Clinical Value Executive Summary Hilo Medical Center (HMC) accomplished an electronic health record (EHR) implementation in May 2010 with well-defined goals of improving clinical outcomes, patient safety, and financial performance. Lack of an integrated medical record prior to EHR implementation placed patients at clinical risk, especially, when medication administration processes were encountered. Medication ordering, verification, dispensing and administration processes all warranted careful review and planned improvement to accomplish the transition from a disparate paper system to a closed loop electronic platform. Addressing continuity of care was of paramount importance as the capabilities of the EHR were evaluated for the provision of Computerized Provider Order Entry (CPOE), Clinical Decision Support (CDS), improved medication processing, and Barcode Medication Verification (BMV). The results demonstrated in this Case Study represent a remarkable reduction in Adverse Drug Events (ADEs) along with associated cost savings to the organization. The overall impact of the EHR on clinical value is illustrated by the improvements in the medication administration process, appropriate antibiotic usage, and the CMS core measure addressing pneumonia. 1. Background Knowledge Hilo Medical Center (HMC) is a part of the East Hawai’i Region of the Hawai’i Health Systems Corporation (HHSC) serving as a safety-net hospital for two critical access hospitals, Hale Ho’ola Hamakua and Ka’u Hospital. The East Hawai’i Region also includes nine outpatient clinics with specialties. HMC is a 276 bed facility comprised of 137 acute beds, 20 bed behavioral health facility, and 119 bed long-term care facility. Overall, 72% of HMC's patients have Medicare or Medicaid insurance. Hilo Medical Center’s Emergency Department is an established Level III Trauma Center providing 24 hour care for the community. The Emergency Department visits total approximately 45,000 patients annually making it the second busiest in the State of Hawai’i. Emergency Department visits range in caring for critically ill or critically injured to low acuity patients not able to obtain primary care services. The island of Hawai’i, also referred to as Hawai’i County can be compared in size to the land Page | 1 area of Connecticut, Hawai’i Island is home to approximately 194,000 residentsi. The county has three major hospitals and four critical access hospitals covering a land mass of 4,028 square miles. Geographically, the three main hospitals are separated by at least 50 miles in distance and an idyllic scenario for development of a robust EHR system The population by county shows Hawai’i County appropriating 15% of adults who are uninsured in comparison to the City and County of Honolulu at 9.2%, Hawai’i County includes a higher number of uninsured seniors than any other countyii. Death rates for cardiovascular disease, smoking, and diabetes are also highest in the state compared to other countiesiii. As a whole, Hawai’i County is designated as a Medically Underserved Area (MUA), 18.3% of the population is living below the poverty level and 16% of patients stating they do not have a usual source of health careiv. Physician shortages are estimated at 36% indicating an 18% higher rate than the City and County of Oahuv. Health care on Hawai’i Island is a collaboration of safety net services with limited access, funding, and capacity when compared to the island of Oahu or large medical centers. Hilo Medical Center is also the sole provider of emergency and acute care for the East Hawai’i region and for the majority of Hawai’i County. Without the services provided by HMC, health care in the East Hawai’i community would be drastically affected. 2. Local Problem Addressed and Intended Improvement The 2014 National Action Plan for Adverse Drug Event (ADE) Prevention indicates ADEs are among the largest contributors to hospital-related complications.vi The Institute for Safe Medication Practices (ISMP) relays that it is not possible to establish a national medication error rate or set a benchmark for medication error rates. Each hospital or organization is different.vii HMC determined baselines and organization tracking of errors could be monitored and trends captured and acted upon. In May 2008, HMC’s all-encompassing medication error rate reached a high of 23 medication errors for every 10,000 administered doses; see Figure 1. Figure 1: Pre and Post EHR Medication Error Rates per 10,000 Administered Doses. EHR Implemented May 2010. Closed Loop Medication Administration Initiated February 2011. Page | 2 In the 1997 study, “The Costs of Adverse Drug Events in Hospitalized Patients”, each avoidable ADE was found to cost $4,685. When adjusted for health care inflation, the cost rises to $8,048 per preventable ADE.viii The HMC pre-EHR medication process was as follows: Doctor provides written order If STAT, order is faxed to pharmacy & written order is placed in pharmacy bin to be picked up when rounding Pharmacy receives order & requests paper labs from Clinical Laboratory Pharmacy fills order and sends medication to the floor Nurse administers medications The medication process was vulnerable to errors and lacked efficiency every step of the way with time to administration delays exceeding desired standards. HMC approached the problem by implementing an integrated EHR targeting the following areas related to medication ordering, verification, dispensing, and administration: Closed Loop Medication Administration Clinical Decision Support Computerized Provider Order Entry Smart Data Bedside Medication Verification In an effort to address the national problem of increased and inappropriate antibiotic usage, the Pharmacy and Therapeutics Committee (P&T) developed an Antibiotic Stewardship Program comprised of nursing, infection control, physician champions, pharmacist, administration, and medical staff leadership. The overall goal of the program was to improve the appropriateness of antibiotic ordering throughout the organization, prevent drug resistance organism, as well as a business case to decrease the use of antibiotics and costs. Initiating an Antibiotic Stewardship Program did not require additional staff or resources associated with starting a program. The P&T Committee was essentially the Antibiotic Stewardship Committee with the addition of the Lab and Infection Control Director and Pathologist. The Physicians on the committee are volunteers. Staff members involved incorporated Antibiotic Stewardship duties in their normal workday. Antibiotic use was monitored using Days of Therapy per 1000 patient days (DOT/1000 patient days). Fifteen antibiotics were targeted for monitoring. The goal was to reduce the DOT/1000 patient days by 5% for the fifteen-targeted antibiotics. Pre-Antibiotic Stewardship Program DOT/1000 patients days was $129/admission (FY13). The successful outcomes of this program were further supported by additional optimizations created within the EHR. Together, the program and EHR processes, aimed to decrease hospital acquired disease processes, like C. difficile impacted by inappropriate antibiotic treatments. “C. difficile infections can be prevented by using infection control recommendations and more careful antibiotic use.”ix The C. difficile rate prior to implementing the Antibiotic Stewardship Program was four patients in 2012, which then climbed to nine patients in 2013. HMC also looked to meet CMS core measures regarding pneumonia, through the utilization of the EHR. 3. Design and Implementation The design of the Antibiotic Stewardship Program was well thought out by the P&T Committee Page | 3 who establishes and maintains a formulary of medications as well as functions related to the use of medications in HMC. Antibiotic Stewardship is an essential function of the committee by which they perform a consulting and decision-making role for the hospital. Utilizing the EHR to track and monitor performance in the use and ordering of antibiotics provides the committee valuable information to reach the goals of the Antibiotic Stewardship Program, which is to decrease antibiotic use by 5% for the selected antibiotics. The design and build of the EHR included reports, which the P&T/Antibiotic Stewardship Program monitors. In addition to the monthly reports, Pharmacy generates automated and on demand daily reports to track appropriate antibiotic ordering. The core EHR modules implemented in May 2010 were designed to integrate all facets of the inpatient medication process. In February 2011, the Closed Loop Medication Administration process became an additional requirement for all acute medication administrations. The combination of both implementations contributed in medication error rates dropping from 23 to consistently 5 or fewer errors (only 1 error in March 2014) per 10,000 administered doses; see Figure 1. Current Closed Loop Medication Administration process – post-EHR implementation: Doctor enters order in EHR Pharmacy verifies order. Lab results automated and available Nurse dispenses from Pyxis & Documents on the MAR The HMC CPOE initiative began in May 2011with the involvement of over 125 of its 250 physicians. Hospitalists place over 70% of HMC’s inpatient orders, of these 54% are medication orders. Protocol orders are primarily used in the Emergency and Obstetrics departments. The system was designed to support CPOE and CDS with the implementation of rapid resulting of laboratory orders to identify and document the critical values necessary for safe and effective medication management. In addition to rapid results reporting, the EHR was developed to collect Smart Data. Smart Data drives decision support, improved care, and better outcomes. CPOE was instrumental in the ordering of antibiotics and monitoring of antibiotic usage. The Antibiotic Stewardship Committee was tasked to create an Order Set to assist physicians in selecting the appropriate antibiotics for specific conditions; see Figure 2. Figure 2: Alternative Antibiotic Orders The Order Set contained suggested orders and listed the daily drug cost for more cost efficient alternatives; see Figures 3 and 4. Figure 3: Alert for Alternative Antibiotics Figure 4: Antibiotic Order Set Page | 4 If the physician attempted to order an antibiotic outside of the Order Set, supplementary questions were embedded in the order to guide further decision-making; see Figure 5. Figure 5: Reserved Antibiotic Questions Figure 6: Antibiotics Usage Report for Pharmacy The Pharmacy generates a daily report in the EHR to monitor the Antibiotics Stewardship Program. The report reflects antibiotics usage for the clinical pharmacist to evaluate the appropriateness of therapy. See Antibiotics Usage Report for Pharmacy in Figure 6. If the antibiotics are inappropriate for the specific clinical problem, it will prompt a direct discussion with the pharmacist and physician(s). The Nursing Process design for Pneumococcal vaccinations contained built in rules with required questions based on patient age and previous vaccination history. Once patient specific criteria was met, a vaccination order was required. Figure 7: Percentage of Patients Scanned Patient wristbands were updated with 2D barcodes in 2013 and an improved scanning approach utilizing wireless devices that increased the scanning rate by 40%. The percentage of patients scanned for the period August – October 2013 recorded on or above 98%; see Figure 7. BMV scan rates continue to range from 90 – 93%. 4. How Health IT Was Utilized HMC chose MEDITECH as its EHR vendor. Additional applications were implemented in short order to fully accomplish integration. Optimization of the system’s functionality to create Smart Data to drive decision support has proven quite beneficial. Prior to the implementation of the EHR, the workflow for medication ordering was on paper and did not allow for real time conflict and interaction checking by a pharmacist prior to Page | 5 administration. Once the order was written in the paper chart by the physician, there were numerous delays in providing a copy of the paper order to the pharmacist. A typical time frame for a clerk or nurse to review orders could take 30 minutes to an hour. Following this process, the paper order would sit in an outbox waiting to be delivered to Pharmacy. This amounted to a total time span from written order to pharmacist review averaging 2-4 hours for non-STAT orders. The Pharmacy Department was also not available 24/7, further causing medication review delays. Orders written late in the evening or during nightshift hours could experience a delayed review time of up to 8 hours. With the EHR and now operating a 24/7 Pharmacy, notifications are provided to the Pharmacy immediately upon a physician saving the entered order within the system. System generated alerts and notifications are displayed, and the physician is prompted to review at the time of ordering. Additional alerts, conflicts, and/or reactions are analyzed by the pharmacist before the nurse is able to acknowledge, scan, or administer the medication. The EHR allowed for adherence to medication administration best practices and improved overall patient care by increasing patient safety levels. To further supplement the reduction in ADE's, order logic was built into the EHR. Suggested orders were added to the CDS functionality for medication interaction checking and the configuration of proactive alerts. Figure 8 demonstrates the pre and post Order Entry workflow comparisons. Figure 8: Pre and Post EHR Physician Order Entry Workflow Pre and Post EHR Physician Order Entry Workflow Pre-EHR Physician Order Entry Workflow Handwritten orders placed for medications, labs, etc. Physician selects Patient to place orders Clerk or RN transcribes orders from chart to needed requisitions Paper order placed in outbox for Pharmacy pick-up Phone call to Pharmacy required for STAT medications RN administers medication to patient No conflict or interaction checking or reminders for required related orders for this process Paper orders sent to Pharmacy 1-4 hours following initial physician order Pharmacy reviewed orders for conflicts or interactions No conflict or interaction checking by Pharmacy prior to administration Post-EHR Physician Order Entry Workflow Navigates to Orders Panel Selects Medical Admission Order Set Use of an Order Set provides consistency in ordering process Selects ALL needed orders (i.e. ABG, EKG, Aspirin, Warfarin, etc.) Best practice solutions embedded within system Physician addresses any conflicts in selected and suggested orders Order electronically transmitted to Pharmacy. System generates alert prior to verifying medication Orders display on nursing worklist or as link on status board Increases Patient Safety by enforcing review for conflict or interaction prior to order placement Page | 6 Medication warnings, such as, those in Figure 9, were developed and are considered a cornerstone of the medication ordering process. Figure 9: Medication Warnings A Medication Monitoring Report created from the EHR’s real-time data gathers patient specific information monthly to track reasons why medications were stopped due to allergies, an adverse reaction or drug intolerance; see Figure 10. Figure 10: Medication Monitoring and Reporting In January 2013, HMC implemented Nova, Telcor’s mobile technology, which integrates directly with the EHR’s on-line electronic medication administration record (eMAR). Introducing the mobile scanning devices improved the scanning rate by 40%, as noted in the previous section. The Antibiotic Stewardship Program tracks and monitors antibiotic use by utilizing the EHR to provide real time reports to the Pharmacy department. Use of the antibiotics Order Set was encouraged as it contained associated lab results, recommended antibiotics, and information on cost, The additional information supports clinical decision-making, although deviating from the order could not be restricted and ordering outside of the Order Set was inevitable; see Figure 11. Figure 11: Antibiotic Order Set To monitor antibiotic ordering outside of the set, a notification to pharmacy was triggered when antibiotics were ordered from a reserved list. The reserved list is broad-spectrum antibiotics that should be saved for more resistant gram-negative organisms and/or for more specific organism such as MRSA. Custom defined questions were built into the order to assist the physician Page | 7 in justifying an antibiotic order and to consider alternatives prior to saving; see Figure 12. An order from the reserved list would appear on a compiled patient report in the EHR that was reviewed daily by Pharmacy to evaluate the appropriateness of antibiotics for patients. Once Pharmacy completes their evaluation of the patient, a recommendation is entered on the patient’s record in a form of a Pharmacy note for nonemergent recommendations. If immediate action is required the provider was contacted immediately by phone or through face-to-face communication. Figure 12: Custom Defined Questions When Ordering Outside of the Antibiotic Order Set Pharmacy also documents the outcome of recommendations in the EHR, which is reviewed monthly by the Antibiotic Stewardship Committee. The reports from the meetings of the Antibiotic Stewardship Committee are discussed in general medical staff meetings and published on the hospital intranet, particularly the antibiogram that physicians use in selecting antibiotics. The reports are also used for program efficacy and overall program improvement. The reports are not currently used for any disciplinary action. Optimizing the capture of outpatient Intravenous (IV) start and stop times was easily resolved by building required fields into the Emergency Department Nursing Disposition Worksheet, a form required for closing a chart. Documenting start and stop on the IV flowsheet; see Figure 13, automatically transfers the information to the Disposition Worksheet. If start and stop were not documented in the IV flowsheet, it would trigger required fields in the Disposition Worksheet creating “hard stop”; see Figure 14. The “hard stop” prevents the user from completing the chart. Figure 13: ED IV Flowsheet Figure 14: ED Nursing Disposition Worksheet Containing “Hard Stops” Through the use of health technology improvements in the Imaging Department, the volume of radiological studies increased from 50,000 studies/year to 59,000 studies/year; however ratios of studies to patients remained the same. The graph in Figure 15, displays the ratio of exam to patients for each modality from 2010 to 2015, which demonstrates a consistent ratio trend from year to year. That trend clearly illustrates the increase in volume was not associated to unnecessary radiological testing ordered per patient . Page | 8 Figure 15: Ratio of Exams to Patients In addition, through information collated within the EHR, imaging technologists are able to question the appropriateness of ordered exams in an effort to limit duplicate or redundant procedures from being performed. The patient's prior exam history is provided on every requisition and immediately available electronically via the EHR; see Figure 16. Along with the order history, a 'Diagnosis/Signs & Symptoms' field is required on every imaging order; see Figure 17. By reviewing the patient's exam history along with this required field, the technologist has the information to determine the suitability of the ordered exam. If the prior exam history displays the same test or the indicated diagnosis or signs and symptoms are not an indication for the exam, the technologist raises their concerns to the ordering physician. Figure 16: Imaging Prior Exam History Figure 17: Diagnosis/Signs & Symptoms Displayed on the Technologist Desktop This process, facilitated through the EHR and the use of tools within it, prevents duplicate or superfluous procedures from being performed. Eliminating redundant or unnecessary exams improves overall patient care by limiting their amount of exposure to ionizing radiation. In addition, it allows technologists to more effectively utilize their time, performing only those exams that are deemed medically necessary, all of which contribute to an increase in safe imaging studies. 5. Value Derived/Outcomes HMC’s implementation of the EHR changed the entire medication ordering and administration process and produced real savings for the hospital and its patients. A fully integrated clinical record for both inpatient and outpatient care is now in place and accessible anytime from any Page | 9 location. Clinicians can view real-time patient data for visits conducted anywhere in the continuum of care. The ability to enter orders, including medication orders using CPOE, improves patient safety by organizing meaningful data into Order Sets with timely clinical alerts and results. Prior to the EHR implementation, HMC’s monthly medication error rate averaged 16.8 errors per 10,000 doses administered per month for 27 months (January 2008 – March 2010). Using the health care inflation adjusted cost per ADE of $8,048; these errors resulted in an ADE cost of $3.7M per 10,000 doses administered over the period. After EHR implementation, the average medication error rate fell to 2.6 errors per 10,000 doses administered over the next 27 months (April 2010 – June 2012). Continuing to assume a single ADE costs $8,048, the total cost over the same period was $564,970; avoided ADE costs equaled $3.0M. Over the subsequent months, the average monthly medication error rate has remained at steady 2.7 errors per 10,000 doses administered; please refer back to Figure 1. Prior to the EHR implementation, HMC’s ADE costs were approximately $135,206 per month per 10,000 doses administered. Those costs using the above assumptions have dropped to $20,925 per month per 10,000 doses administered avoiding preventable ADE costs to the organization and unnecessary complications for our patients. The achieved total cost savings to the organization is $114,281 monthly or $1.4M annually. HMC’s Antibiotic Stewardship Program uses the EHR to collect data and generate reports to optimize antibiotic therapy for patients while also meeting fiduciary responsibilities. The antibiotic medication tracking initiative reports monthly antibiotic expenditures per acute admission. The tracking report alerts Pharmacy to changes in costs needing action. Real-time and monthly clinical data allows clinicians to provide the best antibiotic therapy, avoiding costly suboptimal therapies for patients. The Antibiotic Stewardship Program set a goal of reducing antibiotic use when antibiotics were not necessary and/or ordering antibiotics that Figure 18: January 2015 Improvement in Antibiotic were less costly but just as effective. HMC still Usage and Ordering has work to do in this arena, but the improvements are noteworthy as seen in Figure 18. For example, Caspofungin experienced an ordering drop of 63.6% and Tigecycline 80.4%. The results were accomplished by implementing required questions as well as antibiotic alternatives during the medication ordering process. The goal of reducing DOT/1000 patient days by 5% were achieved in ten of the fifteen-targeted antibiotics. Antibiotics costs were reduced from $129/admission (FY13) to $120/admission (FY14) or a 7% decrease. Page | 10 Exposure to antibiotics is the main risk factor associated with hospital acquired C. difficile infections. While antibiotics are a necessary part of medical treatment, they need to be used appropriately to ensure realization of the biggest benefit with a limited amount of risk. The clinical benefits of having an Antibiotic Stewardship Program and an antibiotic Order Set that is monitored daily by the pharmacist, coupled with questions built into the EHR, has led to a decrease in the facility’s hospital acquired C. difficile rate. The decrease was significant enough f o r the State Department of Health, which monitors the submitted data, to question the data and completed an audit validating the numbers were correct. Through the implementation of the Antibiotic Stewardship Program and associated EHR processes, a 66% decrease in the hospital acquired C. difficile rate was recognized from a high of nine patients in 2013 to zero patients for the current two quarters of 2015; see Figure 19. If it were not for the one patient in December of 2014, the C.diff rate would have been zero for 15 months. Figure 19: Hospital Acquired C. diff Rate per 1000 Pt. Days In conjunction with the medication ordering and appropriate usage of antibiotic enhancements created through use of the EHR, the initiation of processes to meet CMS core measures for Pneumococcal Immunizations were also made. An overall improvement for this core measure was identified and could be correlated through a decrease in Pneumonia mortality rates; see Figure 20. Figure 20: Pneumonia Vaccination and Mortality Rate Page | 11 6. Lessons Learned HMC’s goal was to create a system that increased the efficiency of clinical workflows. It was imperative to involve all stakeholders in this broad organizational change effort, even though some users were highly resistant to change. In order to complete the project with organizational input, HMC integrated a formal change control process alongside the implementation. The culture of the organization evolved with the unified efforts of engaging IT, clinical analysts, and department leadership in the governance, as well as, change control processes. A key means to accomplishing rapid Figure 21: CPOE Adoption deployment of CPOE required early involvement with the hospitalists and physician champions, along with establishment of a CPOE Governance Plan to guide the effort. Placing decisions in the hands of those entering the majority of the inpatient orders promoted acceptance and follow through when the tough conversations surrounding topics such as ADEs needed to occur. HMC is now a leader in CPOE adoption with percentages consistently above 90%; see Figure 21. Although the Antibiotic Order Set was implemented in September of 2012 and the Antibiotic Stewardship Program officially kicked off in January 2013, the adoption of utilizing the recommended Antibiotic Order Set did not yield positive results until 2014 and 2015. The C.diff rates in Figure 19 demonstrate the challenges of persuading physicians to adopt recommendations from the Antibiotic Stewardship Committee. It took patience, tracking, monitoring, and one-to-one physician discussions with peers and pharmacy to alter ordering behavior. The hospital learned applying punitive damages was not necessary. The spike of nine patients with hospital acquired C.diff in 2013 was analyzed by the Infection Control Director who could not find a pattern to account for the increase. The increase was not concentrated to one nursing unit or associated to a single physician, staff, or one antibiotic. The increase highlighted the vigilance of preventing C.diff in the hospital. Over time, the C.diff rates decreased due to the increase use of the Order Sets, direct discussions between physicians and pharmacy, and peer-to-peer physician communication/education. At the same time, Infection Control measures of hand washing and the use of personal protective equipment of staff and housekeeping contributed to the decrease of C.diff patients. 7. Financial Considerations HMC did not use external funding for the EHR project. All funding was from internal operational sources, including hardware, software, consultant implementation resources, and labor costs. East Hawai’i Region’s low cost of ownership for an EHR system was instrumental in eliminating the need for external funding of approximately $8M. Throughout the implementation initiative, HMC invested $31.0M in total costs resultant net Page | 12 benefit value of $4M over the period. For example, a reduction in transcription services has yielded $2.2M, and a reduction of paper chart and paper communication has resulted in a net savings of $2.6M. The benefits also include staff reductions in HIM and the clinics of approximately $5.5M. The actual-to-date cost breakdown is divided into the following categories: a) operational costs: $19,379,517 b) vendor costs: $12,199,986 c) on-going annual maintenance costs: $2,311,266. The savings HMC is now seeing in the ADE arena alone have made the investment more than worthwhile. Improving the safety of using medications has progressed by leaps and bounds for our patients – not only in measurable dollars but most importantly in the health and well-being of our patient population. i Hawaii Island Beacon Community. (2013). Final Report. Retrieved from: http://hibeacon.org/images/uploads/HIBC_FINAL_REPORT_12-27-2013.pdf University of Hawai’i System Report. (2015). Hawaii Physician Workforce Assessment Project. Retrieved from: http://www.hawaii.edu/offices/eaur/govrel/reports/2015/act18-sslh2009_2015_physician-workforce_report.pdf ii iii Hawaii Island Beacon Community. (2013). Final Report. Retrieved from: http://hibeacon.org/images/uploads/HIBC_FINAL_REPORT_12-27-2013.pdf iv Hawaii Health Matters. (2015). Disparities Dashboard, indicators for county: Hawaii. Retrieved from: http://www.hawaiihealthmatters.org/modules.php?op=modload&name=NSIndicator&file=index&topic=0&topic1=County&topic2=Hawaii&breakout=all&regname=Hawaii University of Hawai’i System Report. (2015). Hawaii Physician Workforce Assessment Project. Retrieved from: http://www.hawaii.edu/offices/eaur/govrel/reports/2015/act18-sslh2009_2015_physician-workforce_report.pdf v vi vii U.S Department of Health and Human Services, Office of Disease Prevention and Health Promotion (2014) ISMP, (2014), http://www.ismp.org/faq.asp#Question_2 viii Bates, David W. MD, et al., The Costs of Adverse Drug Event in Hospitalized Patients, 1997 ix Centers for Disease Control and Prevention (2015), Healthcare-associated Infections (HAIs), http://www.cdc.gov/hai/organisms/cdiff/Cdiff_clinicians.html Page | 13