PEM Board Review Series Surgical Emergencies: Abdominal
advertisement

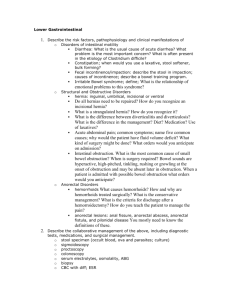
PEM Board Review Series Surgical Emergencies: Abdominal & Genitourinary Pyloric Stenosis: The presence of hypokalemic, hypochloremic metabolic alkalosis suggests the diagnosis of hypertrophic pyloric stenosis (HPS). HPS classically presents between 2 and 8 weeks of age (peak, 3 to 4 weeks) with progressively worsening postprandial vomiting that eventually becomes “projectile” in many cases. Because the obstruction is at the level of the pylorus, the vomiting is nonbilious; prolonged gastric stasis may result in gastritis and hematemesis. As the obstruction and resultant vomiting worsen, the loss of acidic gastric contents and subsequent renal compensation leads to alkalosis and hypokalemia. Poor weight gain progresses to weight loss. With the increased availability of diagnostic radiologic studies, HPS is diagnosed in more patients very early in the disease course, before significant dehydration, weight loss, or electrolyte abnormalities occur. HPS is most common in white infants, less common in African Americans, and rare in the Asian population. The male-to-female ratio is more than 3:1, and first-born males are affected more commonly than subsequent children. The likelihood of developing HPS is significantly increased in infants who have an affected first-degree relative (five times increased risk); a male infant whose mother had HPS has a more than 10-fold increased risk of developing the condition. Another recognized risk factor is neonatal exposure to erythromycin. The pyloric muscle thickness and channel length are measured directly, with a thickness greater than 4 mm and a length greater than 15 mm being diagnostic of HPS. On UGI radiography, the narrowed pyloric channel appears as the “string sign” of thin, elongated barium passing through this region. Although both ultrasonography and UGI have excellent sensitivity for identifying HPS, ultrasonography is superior in differentiating true HPS from pylorospasm. Treatment of HPS starts with fluid resuscitation with isotonic saline and correction of the alkalosis and hypokalemia. Once this has been achieved, surgical correction using either open or laparoscopic pyloromyotomy is performed. Testicular Torsion: Physical examination findings of a high-riding, tender, firm testis with a horizontal lie and an absent cremasteric reflex are highly suggestive of testicular torsion. In certain situations, a urologist may elect to take a patient who has such physical findings directly to the operating room without imaging studies. The most definitive test to evaluate for testicular torsion short of operative exploration is color Doppler ultrasonography. In the presence of a concerning history and physical examination findings, urologic consultation should be sought, even if ultrasonographic findings are not suggestive of torsion. A number of patients who have torsion have white cells present on urinalysis, and some patients who have epididymitis have normal urinalysis results. 1 In cases of torsion, testicular viability is time-dependent; salvage is unlikely if the blood supply is completely disrupted for 6 to 12 hours. However, the torsion often is intermittent and incomplete. Therefore, timely diagnosis and treatment should be attempted, even beyond the traditional 6-hour window. After administration of appropriate analgesia, the physician should grasp the affected testis and rotate it toward the ipsilateral thigh. Several rotations may be required; the degree of torsion may be from 180 to 1,080 degrees. Successful detorsion results in almost immediate pain relief and a return of the testis to a lower position in the scrotum. Although the initial rotation attempt should be toward the affected side (ie, “open the book”), this is the correct direction in only two thirds of the cases. If the attempt does not appear to be successful, the testicle should be rotated in the opposite direction. Because residual torsion is a potential complication of this procedure, Doppler ultrasonography to confirm blood flow and subsequent surgical explorations still are necessary. Torsion of the testicular appendage is most common in boys between the ages of 7-12 years. The scrotal tenderness and swelling may be localized to the superior-lateral aspect of the testis. The “blue dot”, an infracted appendage, may be visible. The cremasteric reflex is usually intact. The treatment is supportive with analgesics, rest, and scrotal support. If the diagnosis of epididymitis is likely (it is a clinical diagnosis), a urinalysis and urine culture should be obtained to r/o UTI. The scrotal pain and swelling in patients with epididymitis is usually more gradual in onset compared to torsion of the testicle or the testicular appendage. Associated symptoms such as dysuria, frequency, discharge, or fever may be present. The cremasteric reflex is intact. The Prehn sign—the relief of pain with elevation of the testis—may be present in epididymitis. In sexually active boys, common causative organisms include Chlamydia, Gonorrhea, E Coli, and viruses. Testing, therefore, for these organisms is indicated in sexually active adolescents. In prepubertal boys, however, epididymitis can be associated with a UTI. Bowel Obstruction: The history of bilious emesis in the newborn period is highly suggestive of obstruction. Plain radiography cannot exclude malrotation or intermittent bowel obstruction, but it is useful to exclude the possibility of perforation. After plain radiography has been completed, the diagnostic test of choice for infants who have possible bowel obstruction is an upper gastrointestinal (UGI) radiographic series. If lower bowel obstruction is suspected (intussusception, Hirschsprung disease), contrast enema (CE) may be indicated. After initial fluid resuscitation, emergent exploratory laparotomy is appropriate if peritoneal signs or evidence of perforation are present. The specific signs and symptoms of gastrointestinal obstruction depend on the level of the obstruction. Obstruction proximal to the ampulla of Vater produces nonbilious emesis; more distal obstruction typically results in bilious vomiting. Abdominal distention is unlikely in proximal obstructions, but is prominent with more distal lesions. 2 Initial therapy for patients who have suspected bowel obstruction is aimed at support of cardiorespiratory function, correction of fluid or electrolyte deficits, and decompression of dilated stomach and small bowel. Ill-appearing or dehydrated patients should receive intravenous fluid therapy and placement of a nasogastric suction catheter. Surgical consultation should be sought early in the course of the evaluation and management of suspected bowel obstruction, and decisions regarding timing and order of radiologic and other tests should be made in conjunction with a pediatric surgeon. Antibiotic therapy is indicated when perforation or peritonitis is suspected and should include broad-spectrum coverage that encompasses gram-positive, gram-negative, and anaerobic organisms. Foreign Bodies: Sharp objects (pins, screws, etc.) greater than 5 cm in length in the stomach or proximal duodenum should be promptly removed using flexible endoscopy. A sharp object that has passed beyond the proximal duodenum in an asymptomatic patient can be followed by serial radiographs to document its passage. Surgical removal is indicated when the object is beyond the reach of an endoscope and the patient is symptomatic. A sharp object in the esophagus should be removed immediately because of a high risk of perforation. If left within the esophageal lumen, disc batteries (bilaminar on x-ray—check both views!) can cause necrosis and ulceration. Therefore, immediate operative removal with flexible or rigid endoscopy is required. The Foley catheter technique involves passage of a deflated catheter distal to the object in the esophagus, inflation of the balloon, and gentle withdrawal of the foreign body, often under fluoroscopic guidance. Foley catheter removal is not recommended for these disc batteries because the esophagus cannot be examined for damage and the rate of removal failure or inadvertent dislodgement into the airway is higher with this technique than with direct endoscopic viewing. Any delay in removal of the battery from the esophagus increases the risk of complications and should be avoided. On the other hand, if the battery already has entered the stomach, it has a 90% chance of passing without intervention. Most authors recommend close follow-up with repeat radiographs in such patients to ensure passage of the battery. Approximately 90% of all foreign bodies ingested by children do pass spontaneously. Many authors recommend expectant waiting for round, smooth objects lodged for less than 24 hours in the esophagus because up to one third of these pass spontaneously, especially if they are in the lower esophagus. Food is an uncommon cause of esophageal obstruction in children, except for those who have underlying anatomic abnormalities, strictures, or scarring. If the patient has a known foreign body that is not radiopaque or one is suspected and the patient is symptomatic, esophagography should be performed. Recently, some authors have recommended computed tomography scan with three-dimensional reconstruction as an alternative to esophagography because barium may obscure the view on subsequent endoscopy or may 3 be aspirated if the foreign body is obstructing the esophageal lumen completely. Of the foreign bodies that become lodged in the “normal” esophagus, approximately 70% become stuck at the level of the thoracic inlet, 15% become stuck in the midesophagus as the aortic arch crosses, and 15% are stopped at the lower esophageal sphincter. Round objects larger than 25 mm in diameter, linear objects longer than 5 to 6 cm, or objects that are sharp are less likely to pass spontaneously and often require removal. Approximately 40% of children who ingest foreign bodies are asymptomatic at presentation. The decision to proceed with imaging (posteroanterior and lateral view of the chest that includes the larynx, down to the stomach) frequently is based on the history of a choking or coughing episode or an eyewitness account of ingestion. If imaging reveals a smooth object at the level of the stomach or lower, expectant waiting is appropriate. Appendicitis: In children with a classic presentation of acute appendicitis (initial poorly localized or periumbilical pain, often followed by vomiting and low-grade fever; pain then migrates to the RLQ; WBC usually 11,000-20,000 during the first 12-24 hours of the illness), surgical consultation should be obtained and further imaging is not indicated. Abdominal-pelvic ultrasound is recommended as the initial diagnostic modality in nonobese children when ovarian pathology is also being considered. Abdominal CT is the preferred initial study in obese patients and/or when ovarian pathology is unlikely. While abdominal x-ray may show an appendicolith in 10% of patients with appendicitis, it is not helpful in making a specific diagnosis or ruling out appendicitis. Intussusception: Symptoms starting with sudden onset of intermittent, colicky abdominal pain, followed by vomiting, along with the finding of blood in the stool, raises suspicion for intussusception, which occurs most commonly in children under 2 years of age. Either gross or occult blood is found in up to 70% of cases. A sausage-shaped mass may be palpable in the right side of the abdomen. In patients with a classic presentation, barium or air-contrast enema is both diagnostic and therapeutic. The reason for an abdominal series is simply to rule out contraindications for an air-contrast enema (namely, free air, pneumatosis intestinalis or a high grade bowel obstruction.) Note: A child with hemolytic anemia or sickle cell disease who has upper abdominal pain has cholelithiasis until proven otherwise. 4 Hirschsprung’s Disease: The majority of patients with Hirschsprung’s Disease are diagnosed during the neonatal period. These infants often have delayed passage of meconium after birth. If not identified early, the initial presentation may include signs and symptoms of distal intestinal obstruction: bilious emesis, distended abdomen, and constipation. Children with Hirschsprung’s Disease often require assistance with bowel movement. Rectal exam classically reveals no stool in the rectal vault. Abdominal x-ray usually shows signs of distal intestinal obstruction with absent or decreased air in the rectum and dilated bowel loops proximal to the aganglionic region. After an abdominal x-ray is performed, a barium enema is the best initial diagnostic procedure. The transition zone, which is a change between contracted aganglionic region and the proximal dilated ganglionated bowel, can be seen in the rectosigmoid region. Anorectal manometry is also another useful diagnostic tool for Hirschsprung’s Disease. In patients with barium enema and anorectal manometry indicating Hirschsprung’s Disease, rectal biopsy is not necessary to confirm the diagnosis. Rectal Bleeding: Meckel’s Diverticulum should be suspected in a child with painless rectal bleeding. 2% of the population is born with this condition. Most patients are asymptomatic. The history often is unrevealing, except for the possible occurrence of previous similar episodes. Laboratory findings usually indicate iron-deficiency anemia from chronic blood loss. A nuclear medicine (technetium-99) scan for ectopic gastric mucosa offers the greatest diagnostic accuracy for this malformation. Treatment is surgical excision. The most common complication is repeated episodic hematochezia. Bleeding occurs as a result of erosion within the ectopic gastric mucosa and is usually painless. Diagnosis starts with a careful history and physical examination. A history of recurrent episodes, points to a chronic (or anatomic) condition. External hemorrhoids and anal fissures usually are readily apparent. A distended or tender abdomen points to more ominous causes of LGI bleeding such as intussusceptions or volvulus. Abnormal pigmentation around the lips suggests Peutz-Jeghers syndrome, or familial intestinal polyposis, which predisposes to intussusception. Trauma to intestinal polyps also can lead to LGI bleeding. Allergic colitis is a common cause of LGI bleeding in the neonate. The most frequent allergen is cow milk protein. Allergic colitis is a diagnosis of exclusion because there is no definitive diagnostic test. Milk protein allergy is unlikely if the child has no cramping or diarrhea. In addition, this condition usually improves and even resolves with time and does not usually manifest with intermittent symptoms. 5 Paraphimosis: The findings of a retracted and swollen foreskin, along with swelling of the glans, in an uncircumsized boy, are consistent with paraphimosis, a condition which occurs when the foreskin is retracted behind the glans and left in that position, causing venous congestion. Manual reduction is the treatment of choice, but may require a penile nerve block or procedural sedation. Application of ice packs and local manual compression of the glans and foreskin can reduce the edema. With the pressure applied to the glans, in a manner similar to turning a “sock inside out,” the foreskin can be reduced back to its normal position. Surgical division of the foreskin (“dorsal slit procedure”) is performed only when the manual reduction fails. Cutting the median bar of the zipper is the recommended method for releasing the foreskin when the foreskin is entrapped in the zipper mechanism. Straddle Injuries: A patient who sustained a straddle injury may present with scrotal swelling, tenderness and ecchymosis. Ultrasound is indicated to determine the extent of injury, which may include intrascrotal hematomas, testicular hematoma, testicular dislocation, and testicular rupture. If the ultrasound is inconclusive, a radionuclide scan may provide additional information. A retrograde urethrogram is indicated when urethral injury is suspected. Posterior urethral injury is associated with pelvic fractures; therefore, pelvic x-ray should only be obtained when fracture is suspected. Blood at the urethral meatus and inability to void suggests injury to the urethra. Other findings associated with urethral injury include hematuria, periurethral or perineal edema and ecchymosis. The diagnosis can be confirmed by performing a retrograde urethrogram. Blind placement of a foley catheter should be avoided when blood is present at the meatus, as such a maneuver can convert a partial tear into a complete transection. A straddle injury is the most common mechanism of injury to the female perineum. Superficial lacerations and vulvar hematomas can be managed by supportive care. Superficial lacerations do NOT require suturing and can be treated conservatively by sitz baths 3-4 times a day—patients with mild urinary retention may be more comfortable voiding in a tub of warm water. The wound should be allowed to heal by secondary intention. When perineal suturing is necessary, it should be performed under moderate or general sedation to minimize trauma to the child. Likewise, patients with significant vaginal lacerations should undergo detailed evaluation by a gynecologist or surgeon under general anesthesia. 6 Priapism: Priapism, a condition seen in patients with sickle cell disease, is a medical emergency. The treatment should begin with IV hydration and analgesics. When treatment is initiated within 4-6 hours, priapism usually resolves with these conservative measures. If there is no response to IV hydration and analgesics, aspiration of the corpora and RBC transfusion should be considered. Flank Trauma: The history of flank contusion along with flank ecchymosis and gross hematuria are indicative of renal injury. Contrast-enhanced CT is the preferred diagnostic modality for evaluation of renal injuries (ultrasound has lower sensitivity in detecting renal injury compared to CT.) Serial urinalyses without an imaging study may be all that are required in patients who are asymptomatic and only have microscopic hematuria after minor trauma. Hernias: The incidence is higher in males and preterm infants, with a predilection for the right side. If the patient presents with no inguinal mass or reducible hernia, they should be referred for an elective outpatient surgical repair. The most common clinical sign is a bulge in the groin that increases in size with increased intra-abdominal pressure. Because an irreducible or incarcerated hernia (Fig. 2) is painful, the infant may be irritable and have a history of vomiting that suggests bowel obstruction. Figure 2: Incarcerated hernia. Courtesy of E. Weiner. 7 Procedural sedation and analgesia followed by manual reduction can reduce the contents into the intra-abdominal cavity. The infant is placed in Trendelenburg position and reduction is accomplished with slow, steady circumferential pressure directing the contents of the hernia sac toward the external inguinal ring. The procedure usually requires several minutes of gradually increasing traction and pressure in the groin. After successful reduction, patients may be admitted to the hospital for observation and elective herniorrhaphy, depending on the local practice pattern. If the contents cannot be reduced manually into the abdominal cavity, emergent surgical consultation is recommended. Failure to reduce the hernia in a timely fashion can lead to development of a strangulated hernia, resulting in bowel infarction. Clinically, such patients are ill, with signs of peritonitis and the skin overlying the hernia appearing discolored and hemorrhagic. For an incarcerated hernia, manual reduction should be performed unless the child has signs of peritonitis. Most incarcerated hernias can be successfully reduced manually. Elective surgical repair after successful manual reduction is associated with lower complication rates compared to emergent surgical reduction. Emergent surgical reduction is only indicated when attempts at manual reduction have failed. Hydroceles: Hydroceles are fluid-filled sacs that do not extend to the inguinal ring. They are painless, boggy, mobile, and transilluminate brilliantly (Fig. 4). Figure 4: Hydroceles are fluid-filled sacs that do not extend to the inguinal ring when palpated. Courtesy of The Media Lab at Doernbecher. Ultrasonography may be helpful when the diagnosis is in doubt or when testicular torsion is suspected. 8 Causes of False-Positive Guaiac Card Testing: Iodide Iron supplements Peroxidase-rich veggies (turnips, horseradish, artichokes, mushrooms, radishes, broccoli, bean sprouts, cauliflower, oranges, bananas, cantaloupes, grapes) Causes of False-Negative Guaiac Card Testing: Antacids Barium Charcoal Chili sauce Cocoa Jello NAC Orange Juice Pepto Bismol Peaches Raisens Red bell peppers Red chili powder Red wines Rifampin Simethicone Spaghetti sauce Sucralfate Tomato paste Vitamin C 9