The Citric Acid Cycle The Catabolism of Acetyl-CoA

L.1&2 Dr. Najlaa AL-Dahhan
1.The Citric Acid Cycle: The Catabolism of Acetyl-CoA
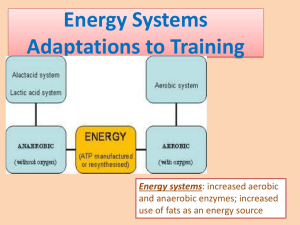
Biomedical importance: The citric acid cycle (Krebs cycle, tricarboxylic acid cycle) is a series of reactions in mitochondria that oxidize acetyl residues
(as acetyl-CoA) and reduce coenzymes that upon reoxidation are linked to the formation of ATP. The citric acid cycle is the final common pathway for the aerobic oxidation of carbohydrate, lipid, and protein because glucose, fatty acids, and most amino acids are metabolized to acetyl-CoA or intermediates of the cycle.
The citric acid cycle provides substrate for the respiratory chain.
Reactions of The citric acid cycle liberate reducing equivalent & CO2.
(Figure 1).Twelve ATP are formed per turn of the citric acid cycle .
Vitamins play key roles in the citric acid cycle .Four of the B vitamins are essential in the citric acid cycle and therefore in energy-yielding metabolism:
(1) riboflavin, in the form of flavin adenine dinucleotide (FAD),a cofactor in the α-ketoglutarate dehydrogenase complex and in succinate dehydrogenase;
(2) niacin, in the form of nicotinamide adenine dinucleotide (NAD), the coenzyme for three dehydrogenases in the cycle—isocitrate dehydrogenase, αketoglutarate dehydrogenase,and malate dehydrogenase; (3) thiamin (vitamin
B1), as thiamin diphosphate, the coenzyme for decarboxylation in the αketoglutarate dehydrogenase reaction;and (4) pantothenic acid, as part of coenzyme A,the cofactor attached to “active” carboxylic acid residues such as acetyl-CoA and succinyl-CoA. The citric acid cycle plays apivotal role in metabolism.
The Citric Acid Cycle Takes Part in Gluconeogenesis, Transamination,&
Deamination.( Figure 2). The Citric Acid Cycle Takes Part in Fatty Acid
Synthesis .Regulation of the citric acid cycle depends primarily on a supply of oxidized Cofactors.
1
2
The citric acid cycle is the final pathway for the oxidation of carbohydrate, lipid, and protein whose common end-metabolite, acetyl-CoA, reacts with oxaloacetate to form citrate. By a series of dehydrogenations and decarboxylations, citrate is degraded,releasing reduced coenzymes and 2CO2 and regenerating oxaloacetate. The reduced coenzymes are oxidized by the respiratory chain linked to formation of ATP. Thus, the cycle is the major route for the generation of ATP and is located in the matrix of mitochondria adjacent to the enzymes of the respiratory chain and oxidative phosphorylation. The citric acid cycle is amphibolic, since in addition to oxidation it is important in the provision of carbon skeletons for gluconeogenesis, fatty acid synthesis,and interconversion of amino acids.
3
2. Glycolysis & the Oxidation of Pyruvate
Biomedical importance :Most tissues have at least some requirement for glucose. In brain, the requirement is substantial. Glycolysis, the major pathway for glucose metabolism, occurs in the cytosol of all cells. It is unique in that it can function either aerobically or anaerobically. Erythrocytes, which lack mitochondria, are completely reliant on glucose as their metabolic fuel and metabolize it by anaerobic glycolysis. However, to oxidize glucose beyond pyruvate (the end product of glycolysis) requires both oxygen and mitochondrial enzyme systems such as the pyruvate dehydrogenase complex, the citric acid cycle, and the respiratory chain . Glycolysis is both the principal route for glucose metabolism and the main pathway for the metabolism of fructose, galactose, and other carbohydrates derived from the diet. Glycolysis canfunction under anaerobic conditions.When a muscle contracts in an anaerobic medium, ie, one from which oxygen is excluded, glycogen disappears and lactate appears as the principal end product. The reactions of glycolysis constitute the main pathway of glucose utllization. The overall equation for glycolysis from glucose to lactate is as follows:All of the enzymes of glycolysis (Figure 3) are found in the cytosol. Glucose enters glycolysis by phosphorylation to glucose
6-phosphate, catalyzed by hexokinase,using ATP as the phosphate donor.
Tissues That Function Under Hypoxic Circumstances Tend to Produce Lactate
(Figure 3).This is true of skeletal muscle, particularly the white fibers, where the rate of work output and therefore the need for ATP formation may exceed the rate at which oxygen can be taken up and utilized. glycolysis in erythrocytes, even under aerobic conditions, always terminates in lactate, because the subsequent reactions of pyruvate are mitochondrial, and erythrocytes lack mitochondria.
4
5
Glycolysis Is regulated at three steps involving nonequilibrium reactions .
Although most of the reactions of glycolysis are reversible, three are markedly exergonic and must therefore be considered physiologically irreversible.These reactions,catalyzed by hexokinase (and glucokinase),phosphofructokinase, and pyruvate kinase.In Erythrocytes, the First Site in Glycolysis for ATP
Generation May Be Bypassed. The oxidation of pyruvate to acetyl-ACoA is the irreversible route from glycolysis to the citric acid cycle. Pyruvate dehydrogenase Is regulated by end-product inhibition & covalent modification.pyruvate dehydrogenase is inhibited by its products,acetyl- CoA and NADH .
Oxidation of glucose yields up to 38 mol of ATP under aerobic conditions but only 2 mol when O2 is absent. Clinical aspects: inhibition of pyruvate metabolism leads to lactic acidosis. Glycolysis is the cytosolic pathway of all mammalian cells for the metabolism of glucose (or glycogen) to pyruvate and lactate. It can function anaerobically by regenerating oxidized NAD+
(required in the glyceraldehyde-3-phosphate dehydrogenase reaction) by reducing pyruvate to lactate. Lactate is the end product of glycolysis under anaerobic conditions (eg, in exercising muscle) or when the metabolic machinery is absent for the further oxidation of pyruvate (eg, in erythrocytes).Glycolysis is regulated by three enzymes catalyzing nonequilibrium reactions: hexokinase, phosphofructokinase,and pyruvate kinase. In erythrocytes, the first site in glycolysis for generation of ATP may be bypassed, leading to the formation of 2,3-bisphosphoglycerate, which is important in decreasing the affinity of hemoglobin for O2. Pyruvate is oxidized to acetyl-CoA by a multienzyme complex, pyruvate dehydrogenase, that is dependent on the vitamin cofactor thiamin diphosphate. Conditions that involve an inability to metabolize pyruvate frequently lead to lactic acidosis.
6
7
L.3
3.Gluconeogenesis & Control of the Blood Glucose
Gluconeogenesis is the term used to include all pathways responsible for converting noncarbohydrate precursors to glucose or glycogen.The major substrates are the glucogenic amino acids and lactate, glycerol, and propionate. liver and kidney are the major gluconeogenic tissues.
Gluconeogenesis involves glycolysis ,The citric acid cycle & some special reactions .Thermodynamic Barriers Prevent a Simple Reversal of Glycolysis
.Three nonequilibrium reactions catalyzed by hexokinase, phosphofructo kinase, and pyruvate kinase prevent simple reversal of glycolysis for glucose synthesis .They are circumvented as follows:
A. Pyruvate & Phosphoenolpyruvate.
B. Fructose 1,6-bisphosphate & fructose 6-phosphate
C. Glucose 6-Phosphate &glucose .
D. Glucose lucose 1-Phosphate &glycogen.
Since glycolysis &gluconeogenesis share the same pathway but in opposite directions ,they must be regulated reciprocally. Induction & repression of key enzyme synthesis requires several hours.covalent modification by reversible phosphorylation Is rapid. Allosteric modification is instantaneous.fructose 2,6-bisphosphate plays a unique role in the Regulation of glycolysis &gluconeogenesis in liver.substrate (Futile) cycles allow fine tuning.The concentration of blood glucose is regulated within narrowlimits.blood glucose is derived from the diet,gluconeogenesis& glycogenolysis.metabolic &hormonal mechanisms regulate the concentration of the blood glucose. glucokinase Is important in regulating blood glucose after a meal. Insulin plays a central Role in regulating blood glucose. glucagon opposes the actions of insulin.other hormones affect blood glucose.Further cilinical aspects. glucosuria occurs when the renal threshold for glucose Is exceeded. hypoglycemia may occur during pregnancy &in the neonate. The
8
body’s ability to utilize glucose may be ascertained by measuring Its glucose tolerance.
Gluconeogenesis is the process of converting noncarbohydrates to glucose or glycogen. It is of particular importance when carbohydrate is not available from the diet. Significant substrates are amino acids, lactate,glycerol, and propionate.The pathway of gluconeogenesis in the liver and kidney utilizes those reactions in glycolysis which are reversible plus four additional reactions that circumvent the irreversible nonequilibrium reactions.Since glycolysis and gluconeogenesis share the same pathway but operate in opposite directions, their activities are regulated reciprocally. The liver regulates the blood glucose after a meal because it contains the high-Km glucokinase that promotes increased hepatic utilization of glucose. Insulin is secreted as a direct response to hyperglycemia;it stimulates the liver to store glucose as glycogen and facilitates uptake of glucose into extrahepatic tissues.
Glucagon is secreted as a response to hypoglycemia and activates both glycogenolysis and gluconeogenesis in the liver, causing release of glucose into the blood.
9
10
11