Fibrinolytic
advertisement

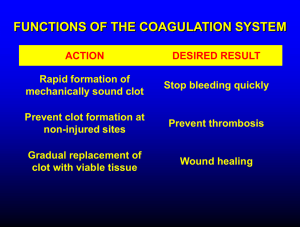
lec 6_ Fibrinolytic “Thrombolytic” drugs **Hemostasis refers to the finely regulated dynamic process of maintaining fluidity of the blood, repairing vascular injury, and limiting blood loss & avoiding vessel occlusion Hemostasis refers to the prevention of blood loss, and is accomplished by vasoconstriction and coagulation by cellular and coagulation factors. Undue bleeding is controlled and the fluidity of the blood is maintained by counterbalances within the coagulation and fibrinolytic systems. Blood vessel injury or disruption, platelet defects, abnormalities of the normally circulating anticoagulants and fibrinolytic mechanisms may upset the balance between fibrinolysis and coagulation. Blood normally circulates through endothelium-lined vessels without coagulation or platelet activation occurring and without appreciable hemorrhage. Injury to the endothelial cells triggers the hemostatic process, which typically begins with the attachment of platelets (“Adhesion”) to the damaged endothelium or exposed subendothelial proteins such as collagen and von Willebrand factor (vWf). The platelets then change form (“Activate”) and release factors that stimulate the clotting process. They also bind together (“Aggregate”). At the same time, plasma proteins may react with elements in the subendothelium, activating the “contact” phase of coagulation. Exposed fibroblasts and macrophages present tissue factor, a membrane protein, to the blood at the injured site, thereby triggering the “Extrinsic “phase of blood coagulation. Under normal conditions, hemostasis protects the individual from massive bleeding secondary to trauma. In abnormal states, life-threatening bleeding can occur or thrombosis can occlude the vascular tree. Hemostasis is influenced by a number of different factors including: (a) vascular extracellular matrix and alterations in endothelial reactivity, (b) platelets, (c) coagulation proteins, (d) inhibitors of coagulation, and (e) fibrinolysis. Hemostasis Platelets Hemostatic plug Fibrin Hemostasis means finely regulated dynamic process of maintaining fluidity of the blood, repairing vascular injury, and limiting blood loss & avoiding vessel occlusion After the formation of a thrombus, flow must be restored by lysis of the clot “fibrinolysis” that means fibrin digestion by the fibrin-specific protease, plasmin During plug formation thefibrinolytic pathway is locally activated. Plasminogen is converted to plasmin ( fibrinolysin by plasminogen activators in the tissue. Plasmin dissolves the fibrin network as wound heal A fibrinolytic cascade is initiated concomitantly with the coagulation cascade, resulting in the formation of plasmin, which digests fibrin. Thrombosis: • Occlusion of an artery or a vein caused by a thrombus or embolus - results in ischemia & necrosis of the tissues • When they occur in coronary, cerebral or pulmonary vessels, they can be immediately life-threatening • Coronary thrombi are the cause of MI, cerebrovascular thrombi produce strokes **, and pulmonary thromboemboli can lead to respiratory and cardiac failure Aim of Therapy: • It takes about 1 to 2 weeks for the blood clot to disintegrate by natural fibrinolytic mechanisms • If the thrombus is dissolved quicker damage will be minimized & blood flow restored faster purpose of therapy • Therefore, it is important to rapidly diagnose and treat blood clots Thrombolytic drugs: • Thrombolytic drugs dissolve blood clots by activating plasminogen, which forms plasmin , a proteolytic enzyme capable of breaking cross-links between fibrin molecules • Because of these actions, thrombolytic drugs are also called "plasminogen activators" and "fibrinolytic drugs" • Thrombolytic drugs are used in the acute stage of thromboembolic events to dissolve thrombi (e.g. acute MI) • It is important to note that the efficacy of thrombolytic drugs depends on the age of the clot. Older clots have more fibrin cross-linking and are more compacted; therefore, older clots are more difficult to dissolve **It is important to note that the efficacy of thrombolytic drugs depends on the age of the clot. Older clots have more fibrin cross-linking and are more compacted; therefore, older clots are more difficult to dissolve Thrombolytic drugs – Indications: The advantage of therapy is highest within the first few hours They are administered by IV infusion To dissolve thrombi in case of : Acute myocardial infarction (MI) Deep vein thrombosis (DVT) Pulmonary embolism (PE) **Clearing thrombosed shunts and cannulae Thrombolytic drugs mechanism of action **Thrombolytic drugs catalyse the conversion of the proenzyme plasminogen to plasmin, which, when in proximity to a thrombus or embolus… Thrombolytic drugs – mechanism of action …degrades fibrin into soluble peptides **Plasmin itself cannot be used because naturally occurring inhibitors in plasma prevent its effects…degrades fibrin into soluble peptides, known as fibrin degradation products (FDPs) and D-dimers, thus dissolving the main body of the clot. These drugs are therefore often referred to as ‘clot busters’. Examples of Fibrinolytic drugs: 1- Streptokinase (SK) the first thrombolytic drug and Urokinase 2- Tissue plasminogen activator (t-PA) is naturally occurring but is manufactured using recombinant DNA technology “ Alteplase” 3-Recombinant mutant variants of t-PA, “Reteplase ***1- Streptokinase (SK) the first thrombolytic drug and urokinase have now been replaced by the 2nd generation agent Streptokinase (Streptase: It is a bacterial protein obtained from cultures of ß-haemolytic streptococci • Streptokinase activates plasminogen, catalyses the conversion of plasminogen to plasmin • Infused intravenously, it reduces mortality in acute myocardial infarction, and this beneficial effect is additive with aspirin **is a protein extracted from cultures of streptococci. As a bacterial product continuous use - immune reaction It activates plasminogen. Infused intravenously, it reduces mortality in acute myocardial infarction, and this beneficial effect is additive with aspirin (Fig. 21.8). Its action is blocked by anti bodies, which appear about 4 days or more after the initial dose. At least 1 year must elapse before it is used again. , it still activates circulating plasminogen thereby releasing plasmin, which can lead to the breakdown of circulating fibrinogen and cause an unwanted systemic fibrinolytic state. Streptokinase : Side Effects: • High incidence of bleeding (GI bleeding, cerebral hemorrhage) as plasmin lysis fibrin haemostatic plugs and degrades fibrinogen and factor V and VII, causing systemic fibrinolytic state. • Hypersenstivity: Patients with antistreptococcal antibodies can develop fever, rash, and therapeutic failure Hypotension (due to formation of plasmin and generation of kinins **High incidence of bleeding (GI bleeding ,cerebral hemorrhage) as plasmin lysis fibrin haemostatic plugs and degrades fibrinogen and factor V and VIIcause an unwanted systemic fibrinolytic state. . Streptokinase causes a burst of plasmin formation, generating kinins (see Ch. 13), and can cause hypotension by this mechanism. Urokinase: • Urokinase (UK) is a human enzyme synthesized by the kidney that directly converts plasminogen to active plasmin • It has limited clinical use because, like SK, it produces considerable fibrinogenolysis • One benefit over SK is that UK is non-antigenic but it is expensive **Urokinase (Abbokinase®; UK) is sometimes referred to as urinary-type plasminogen activator (uPA) because it is formed by kidneys and is found in urine. It has limited clinical use because, like SK, it produces considerable fibrinogenolysis; however, it is used for pulmonary embolism. One benefit over SK is that UK is non-antigenic; however, this is offset by a much greater cost. Tissue plasminogen activator (t-PA): t-PA is an endogenous fibrinolytic protein produced by the endothelium (important in maintaining the body's own clot-dissolving process) t-PA is more active on fibrin-bound plasminogen than on plasma plasminogen, and is therefore a 'clot-selective **This family of thrombolytic drugs is used in acute myocardial infarction, cerebrovascular thrombotic stroke and pulmonary embolism. For acute myocardial infarctions, tissue plasminogen activators are generally preferred over streptokinase. This family of thrombolytic drugs is used in acute myocardial infarction, cerebrovascular thrombotic stroke and pulmonary embolism. For acute myocardial infarctions, tissue plasminogen activators are generally preferred over streptokinase. But because of the relative fibrin specificity of tPA, clot dissolution occurs with less breakdown of circulating fibrinogen than occurs with SK and UK • This family of thrombolytic drugs is used in acute MI, cerebrovascular thrombotic stroke and pulmonary embolism • For acute MI, t-PAs are generally preferred over streptokinase Alteplase (Activase): t-PA , alteplase is a recombinant form of human tPA Alteplase has the following advantages: i- it is not allergic ii-It is clot selective Therefore can be given in: i. Severe life threatening clot ii. Known recent streptococcal infection iii. Previous exposure to streptokinase It has a very short duration of action (5 min) **Alteplase (Activase®; rtPA) is a recombinant form of human tPA. It has a short half-life (~5 min) and therefore is usually administered as an intravenous bolus followed by an infusion. Third-generation thrombolytic drugs: • Third-generation thrombolytic drugs are recombinant mutant variants of t-PA and have comparable efficacy with that of t-PA • They differ from native t-PA by having increased plasma half-lives that allow more convenient dosing • These agents are similar to t-PA in efficacy and toxicity • Examples: Reteplase Contraindications to Thrombolytic Therapy: • Active bleeding • Pregnancy • General surgery within the previous 10 days Thrombolytic Therapy: Drawbacks: • A single course of fibrinolytic drugs is expensive: hundreds of dollars for streptokinase and thousands for urokinase and t-PA • Additional disadvantage of current thrombolytic drugs is that they can only be administered by injection Toxicity of Thrombolytic Therapy: The major toxicity of all thrombolytic agents is hemorrhage which results from two factors: (1) The lysis of fibrin in "physiological thrombi" at sites of vascular injury (2) A systemic lytic state that results from systemic formation of plasmin, which degrades fibrinogen and other coagulation factors (esp. factors V and VIII). Treatment of bleeding during use of thrombolytic drugs: Stop the drug Fresh frozen blood / fibrinogen concentrate Aminocaproic acid / tranexamic acid Inhibition of Fibrinolysis Aminocaproic Acid & Tranexamic acid • Aminocaproic Acid & Tranexamic acid are potent inhibitor of fibrinolysis which inhibit activation of plasminogen • They can be given by IV or oral routes • Side effects: intravascular thrombosis THANK YOU