Clinical uses
advertisement

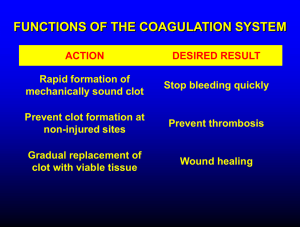
Chapter 29 Agents affecting blood and hematopoietic organ Dysfunctions of blood • Thrombosis – the formation of an unwanted clot within the blood vessls or heart • Bleeding disorders –due to failure of hemostasis and include hemophilia and vitamin K deficiency • Anemia -- caused by nutritional deficiency • • • • • • • Anticoagulants Antiplatelet drugs antithrombolic drugs Fibrinolytic drugs Hemostatics Agents Used in Anemia Hematopoietic growth factors Plasma volume expanders Clot formation requires platelet activation and aggregation (white clot or platelet clot), followed by formation of a fibrin clot (red clot). intrinsic pathway Ⅻ Ⅻa process of normal blood coagulation + Ⅺ Ⅺa extrinsic pathway + Ⅸ Ⅸa + Ⅹ Ⅲ, Ⅶ Ⅲa,Ⅶa + Ⅹa ⅩIII Ⅹ + + Thrombin(Ⅱa) Prothrombin(Ⅱ) + fibrinogen ⅩIIIa + Fibrin Fibrin (soluble) ( Insoluble) Fibrin clot §1 anticoagulants Anticoagulants are drugs employed in preventing blood coagulation. They inhibit certain clotting factors in the liver. The function of them is to: • 1) prevent the formation of new blood clots. • 2) keep existing blood clots from growing larger. Classification of anticoagulants ⅠAnticoagulants both in vivo and vitro: e.g. Heparin Ⅱ Anticoagulants in vivo: dicoumarol Ⅲ Anticoagulants in vitro: Sodium citrate 1. Heparin 1.1 source and chemistry (1)large amount of negative charge (2)strong acidity pharmacokinetics Absorption • Administered by i.v or s.c Metabolism Excretion 1.2 Pharmacological effects • 1. Anticoagulative effect Mechanism: accelerate inactivation of clotting factors.(Ⅱa, Ⅸa, Ⅹa, Ⅺa, Ⅻa ) by enhancing the anticoagulative activity of ATⅢ ( antithrombin Ⅲ ). Ⅻ Ⅻa + Ⅺ Ⅺa + Ⅸ Ⅸa + Ⅹ Ⅶ Ⅶa + Ⅹa ⅩIII Ⅹ + + Thrombin(Ⅱa) Prothrombin(Ⅱ) + fibrinogen ⅩIIIa + Fibrin Fibrin soluble insoluble Fibrin clot ATⅢ: a plasma protease inhibitor Mechanism of heparin • This reaction happens in normal physiological state, but it’s very slow and weak. • In the presence of heparin (which acts as an catalyst), it will be accelerated by more than 1,000 times Characteristics of anticoagulative effect • effective both in vivo and in vitro • quick onset and potent effects • efficacy positively relative to mocular weight 1.2 Pharmacological effects • 2.Other effects adjusting blood lipid anti-inflammatory effect anti-proliferative effect on vascular smooth muscle cell inhibiting pletelet aggregation ……. 1.3 Clinical uses 1) thromboembolic disease: deep venous thrombosis(DVT), pulmonary embolism, unstable angina, acute myocardial infarction, cerebral infarction 2) DIC (Disseminated intravascular coagulation): early stage 3) extracorporal circulation (eg. dialysis machine) 1.4 Adverse reactions • Spontaneous hemorrhage : monitoring of aPTT antagonist: protamine sulfate(1mg:100u) • Heparin-induced thrombocytopenia: (a decrease in circulating platelets) 2~10 days of therapy, 3% , • Others : allergic reaction osteoporosis(骨质疏松) 1.5 Contraindications: 1. Bleeding tendency: • Severe hypertension • Ulcer • surgery of the brain ,eye, spinal cord 2. pregnancy 3. Renal and hepatic dysfunctions LMWHS (low molecular weight heparins) • • • • • Weaker effect than heparin Low incidence of hemorrage Long-lasting effect Small individual deviation No need to monitor generally Coumarin derivatives ---Oral anticoagulants These agents are often referred to as oral anticoagulants because they are administered orally, which exists as the main difference from heparin. • Warfarin(华法林), • Dicoumarin(双香豆素) • Acenocoumarin (醋硝香豆素) pharmacokinetics • Absorption: rapid and complete (warfarin) • Distribution: PPBR>90% • Elimination: liver • Excretion: kindney 4.1 pharmacological effects • Anticoagulative effect 1) mechanism: antagonizing Vit K→inhibiting the synthesis of cloting factor Ⅱ,Ⅶ,Ⅸ,Ⅹ Precursors of Ⅱ、Ⅶ、Ⅸ、Ⅹ Vitamin K (reduced) mature Ⅱ、Ⅶ、Ⅸ、Ⅹ Vitamin K epoXide reductase warfarin Vitamin K (epoxide) Mechanism of Oral anticoagulants Several clotting factors (Ⅱ, Ⅶ, Ⅸ, Ⅹ) depend on vit K as a coenzyme in their complete synthesis by the liver. Oral anticoagulants antagonize VitK →inhibiting the synthesis of clotting factorⅡ,Ⅶ,Ⅸ,Ⅹ →inhibiting coagulation 2) • • • • characteristics (1) oral administration (2) effective in vivo, not in vitro (3) slow onset, long duration (4) overcome by administration of Vitamin K • 4.2 clinical uses: For long use • Prevent acute deep vein thrombosis or pulmonary embolism Prevent venous throboembolism in patients undergoing orthopedic or gynecological surgery Prevent systemic embolization in patients with myocardial infarction, prosthetic heart valves or chronic atrial fibrillation 4.3 adverse effects 4.3.1 Spontaneous hemorrhage : monitoring of PT (凝血酶原时间) Treatment: withdrawal of the drug; administration of vitamin K and fresh blood 4.3.2 others: birth defect (warfarin) Allergic reaction • 4.4 drug interactions 4.4.1 enzyme inducer:barbiturates 4.4.2 competitive antagonist: Vit K 4.4.3 high PPBR: aspirin, quinidine, sulfonamide, phenylbutazone 4.4.4 enzyme inhibitor: cimetidine, isoniazid 4.4.5 PLT inhibitors: aspirin Ⅲ Anticoagulants in vitro Sodium citrate, potassium oxalate Mechanism: Ca2+ Uses: prevent blood coagulation in vitro §2 Fibrinolytic drugs (thrombolytic agents) These agents can activate the conversion of plasminogen to plasmin, a serine protease that hydrolyzes fibrin and thus dissolves clots. Mainly used in acute thrombolism. plasminogen inhibitors - activators + (Fibrinolytic drugs) plasmin + Degration products fibrinogen + fibrin fibrin splits products Ⅰ Plasminogen activator from human body Urokinase (UK) , Alteplase (t-PA) Ⅱ Plasminogen activator form bacteria Streptokinase (SK) , Anistreplase, Stephylokinase Ⅲ Plasminogen activator from snake Snake venom antithrombus enzyme, Ancrod, Acutase SHARED CHARACTERISTICS • ACTION • All act either direct or indirect to convert plasminogen to plasmin, which in turn cleaves fibrin, thus lysing thrombi. • Clot dissolution occurs with a higher frequency when therapy is initiated early after clot formation. • CLINICAL USES: • Used for the treatment of deep-vein thrombosis, serious pulmonary embolism, acute myocardial infarction, peripheral arterial thrombosis, etc. 1. Streptokinase(SK) • 1.1 mechanism: acts indirectly SK-plasminogen complex → activate plasminogen • 1.2 clinical uses: thrombolytic therapy: early,< 6h intravenous route: DVT, multiple pulmonary emboli intra-arterial route: myocardial infarction • 1.3 adverse reactions: • bleeding, hypotension, allergic reaction plasminogen inhibitors - + SK- plasminogen complex plasmin + Degration products fibrinogen + fibrin fibrin splits products 2. Urokinase(UK) • mechanism: activating plasminogen directly • clinical uses: Same use as SK, especially cerebral embolism • adverse reactions: bleeding, but no antigenicity plasminogen inhibitors - + UK plasmin + Degration products fibrinogen + fibrin fibrin splits products 3.tissue plasminogen activator (t-PA) Mechanism: act directly Charateristics: • act selectively , risk of bleeding ↓ (High affinity to plasmnogen bound to fibrin in the embolism ,low affinity to free plasmnogen) • superior to SK and UK 4. anistreplase (anisoylated plasminogen streptokinase activator complex) • a complex of purified human plasminogen and bacterial streptokinase that has been acylated to protect the enzyme’s active site. • When administered, the acyl group spontaneously hydrolyzes, activating streptokinase-proactivator complex. • greater clot selectivity (ie, more activity on plasminogen associated with clots than on free plasminogen in the blood) §3 antiplatelet drugs Antipletelet drug---- Drug that inhibits platelets from aggregating to form a plug. They are used to prevent clotting and alter the natural course of atherosclerosis. Platelets activation processes involve three steps: 1.adhesion to the site of injury 2.release of intracellular granules 3.aggregation of the platelets. Classification Ⅰ Inhibitors of platelet metabolism Ⅱ Agents inhibting platelet activity induced by ADP: Ticlopidine Ⅲ Thrombin inhibitor: argatroban IV GPΠb / Шa receptor blocker: abciximab aspirins TXA2 - AA COX (-) AC COX aspirinl PGI2 (+) + Dipyridamole AC PDE cAMP ↓ ↑aggregation (PLT) cAMP↑ 5-AMP ↓aggregation (endothelium) Ⅰ Inhibitors of platelet metabolism ⅰ Cyclooxygenase inhibitors: Aspirin ⅱ PDE inhibitors : Dipyridamole ⅲ TXA2 synthetase inhibitor: Ridogrel ⅳ Activators of adenylate cyclase: epoprostenol (PGI2) ⅰ Cyclooxygenase inhibitors: Aspirin • Aspirin is a classic old drug which is used as a NSAIDs for more than 100 years. Besides antipyretic, analgesic and antiinflammatory activities, it can inhibit platelet aggregation. Pay attention! • at small dose (50~75mg/d): inhibit the synthesis of TXA2 – which causes platelet aggregation • at higher doses (> 320 mg/day): inhibits the synthesis of PGI2 – which inhibits platelet aggregation. Clinical Uses Prophylaxis after cardiac operation to reduce the incidence of recurrent myocardial infarction (MI) Prophylaxis for transient ischemic attacks (TIA) or post TIA ⅱ PDE inhibitors : Dipyridamole Mechanism : 1) ↓PDE → cAMP ↑ ↓ aggregation 2) ↓ the uptake of adenosine →↑AC Clinical use: Substitute of aspirin prosthetic heart valves, etc. • ⅲ TXA2 synthetase inhibitor: Ridogrel • More effective than aspirin • Fewer adverse reaction Ⅱ Agents inhibting platelet activity induced by ADP: Ticlopidine Broad spectrum inhibitor of PLT aggregation • Mechanism: disturb the release of α-granule and binding of fibrin to GP Ⅱb/ Ⅲ a receptor induced by ADP • Clinic use: thromboembolic disease • Severe toxicity: nausea, bone marrow depression • Ⅲ Thrombin inhibitor: • Argatroban • Thrombin inhibitor • has a short half-life, is given by continuous intravenous infusion, and monitoring is done by aPTT. • Its clearance is not affected by renal disease but is dependent on liver function. hirudin • irreversible thrombin inhibitor from the leech • now available in recombinant form as lepirudinin. • has a short half-life, but it accumulates in renal insufficiency and no antidote exists. • Mainly used after surgery IV GPΠb / Шa receptor blocker: abciximab(阿昔单抗) • • activation of glycoprotein receptor on PLT membrane is the final common pathway for platelet aggregation. Mechanism: blockade of glycoprotein receptors on PLT membrane §4 Hemostatics Ⅰ Coagulants Vitamin K Ⅱ Antifibrinolytic drugs Tranexamic acid Aminomethylbenzoic acid Ⅲ Thrombin Ⅳ Vasoconstrictors Etamsylate Posterior pituitary(垂体后叶素) ⅰ Vitamin K • [Source and types] • Vitamin K is found in meats, dairy products, leafy green vegetables • Two natural forms : VitK1,VitK2 • Two synthesized forms: VitK3,VitK4 Mechanism of vitamin K Smoe clotting factors (Ⅱ, Ⅶ, Ⅸ, Ⅹ) that are involved in the coagulation reactions depend on vitamin K as a coenzyme in their complete synthesis by the liver. Ⅻ Ⅻa + Ⅺ Ⅺa + Ⅸ Ⅸa + Ⅹ Ⅶ Ⅶa + Ⅹa ⅩIII Ⅹ + + Thrombin(Ⅱa) Prothrombin(Ⅱ) + fibrinogen ⅩIIIa + Fibrin Fibrin soluble insoluble Fibrin clot • Clinical uses: Hemorrage resulting from VitK deficiency 1) Excess of oral anticoagulants 2) Obstructive jaundice and biliary fistula (vitamin K is a fat-soluble vitamin ) 3) long term use of broad spectrum antibiotics: (some vitamin K is synthesized by intestinal bacteria.) 4) Prevent hemorrhage in newborn baby and premature infants. Ⅱ Anti-fibrinolysin(抗纤溶剂) • Aminomethylbenzoic acid • Mechanism: • 1) inhibit plasminogen activation 2) inhibit the activity of plasmin (large dose) • Clinical uses bleeding due to high activity of plasmin • Adverse reactions intravascular thrombosis plasminogen inhibitors - + activators (Anti-fibrinolysin) plasmin + Degration products fibrinogen + fibrin fibrin splits products Ⅲ Thrombin (Factor Ⅱ) • Extracted from animal blood • Activate firinogen to fibrin • Used to stop bleeding or hemorrhage. §5 Agents Used in Anemia • Anemia ---a deficiency in erythrocytes or hemoglobin. • Normal value • Adult male • Adult famale RBC(104/μL) 12~16 11~15 Hb(g/dL) 400~550 350~500 Types of anemia • • • • Iron-deficiency anemia megaloblastic anemia aplastic anemia hemolytic anemia 1. Iron • p.o.: Ferrous sulfate(硫酸亚铁) Ferric ammonium citrate(枸橼酸铁铵) Ferrous fumarate(富马酸亚铁) • i.m.: Iron dextran Pharmacokinetics: Absorption: Fe2+ Increase: Vitamin C, amino acid, gastric acid Decrease: phosphorus, calcium,Tannic acid, Antacids, H2-receptor blockers, Proton pump inhibitors, Tetracyclines • Transfer: transferrin • Utilization: transferrin-R on proliferating erythroid cells. • Storage: ferritin(Fe3+) in intestinal mucosal cells and in macrophages in the liver, spleen, and bone. Pharmacological actions: Iron is part of hemoglobin, the oxygencarrying component of the blood. Irondeficient people tire easily because their bodies are starved for oxygen. Iron is also part of myoglobin. Myoglobin helps muscle cells store oxygen. Clinical uses: • treatment or prevention of iron deficiency anemia • 1) chronic blood loss in heavy menstrution or hemorrhoid • 2) insufficient intake during periods of accelerated growth in children, or in pregnant women. 10~14d 4~8w 2~3m Adverse reactions • 1) p.o. : marked gastrointestinal irritation • 2) i.m. : remarkable local irritation • 3) acute iron toxicity: >1g gastric irrigation→shock→death lavage: phosphate or carbonate deferoxamine: a potent iron chelating compound • 2. Folic acid • Process in body FA → FH2 → FH4 → 5-CH3-FH4 • Machinism: One carbon unit carrier • ☆ Reduction of folic acid → ↓dTMP →↓ DNA→megaloblastic anemia ↓amino acid biosynthesis • Clinical uses: • 1. Megaloblastic anemia • 2. Pernicious anemia • 3. Megaloblastic anemia caused by FH2 reductase inhibitors: methotrexate, Pyrimethamine(乙嘧啶,息疟定) Calcium Leucovorin ( not for regular deficiency ) 3. Vitamin B12 Source: • Meat (especially liver), eggs, and dairy products. Pharmacokinetics: • Requirements of Vitamin B12: 1μg/d • Absorption: intrinsic factor • Storage: in liver Pharmacological Action: dUMP dTMP • 1) methyl transfer • pernicious anemia • 2) isomerization of methylmalonyl-CoA to succinyl-CoA • destroy integrity of myelin sheath→ nerve damage TAC Clinical uses: 1. Megaloblastic anemia 2 .Pernicious anemia 3 .Nervous system diseases 4. Hepatopathy Section 6 Hematopoietic growth factors Erythropoietin (EPO) Granulocyte colony-stimulating factor (G-CSF) Granulocyte-macrophage colonystimulating factor (GM-CSF) Erythropoietin (EPO) source: produced by the kidney in response to tissue hypoxia. Pharmacological effects: • stimulates erythroid proliferation and differentiation • Stimulates maturation of red blood cell • also induces release of reticulocytes from the bone marrow Clinical uses: • patients with chronic renal failure • patients with aplastic anemia • anemias associated with chronic inflammation, AIDS, and cancer Adverse reaction: • a rapid increase in hemoglobin • hypertension and thrombotic complications. Granulocyte colony-stimulating factor (G-CSF) Pharmacological effects: • stimulates proliferation and differentiation of progenitors to neutrophils • Increase release of neutrophils from bone marrow • activates the phagocytic activity of mature neutrophils and prolongs their survival in the circulation. Clinical uses: neutropenia Granulocyte-macrophage colonystimulating factor (GM-CSF) Pharmacological effects: • stimulates proliferation and differentiation of early and late granulocytic progenitor cells as well as erythroid and megakaryocyte progenitors • stimulates the function of mature neutrophils • Clinical uses: neutropenia • Adverse reaction: fevers, malaise, arthralgias, myalgias, peripheral edema and pleural or pericardial effusions, allergic reactions Section 7 Plasma volume expanders • Used to replace or maintain blood vol • Charactristics: – ↑ plasma Osmotic pressure – Slowly eliminated – Not toxic – No antigenicy dextran Dextran 70 (medium molecular dextran) Dextran 40 (low molecular dextran) Dextran 10 (small molecular dextran) Pharmacological actions • Increase plasma Osmotic pressure ↑ blood volume ( dextran 70 > dextran 40 >dextran 20 ) • Anti-coagulative effect: ↓aggregation of red blood cell, platelet ; inhibit clotting factor Ⅱ; improve microcirclation • Osmotic diuretic effect Clinical uses • hypovolemic shock • Thrombolic disease Adverse reaction • Alergic effect • Dysfunction of blood coagulation • AHF