Basic Word version - Healthwatch Sandwell
advertisement

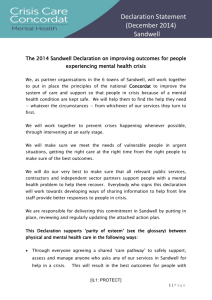
Right Care Right Here partnership Background • Established, growing partnership between health, social and voluntary care organisations across Sandwell & West Birmingham, including: – Black Country Mental Health Partnership NHS Trust – Sandwell Council for Voluntary Organisations – Sandwell Council – Sandwell & West Birmingham NHS Trust – Sandwell & West Birmingham Clinical Commissioning Group (CCG) – Your Health Partnerships – Sandwell Healthwatch • 10 Health & Wellbeing objectives & 10 Regeneration pledges Work so far……. • 2006/7 public consultation - large amount of care in community, single specialist hospital, community hospitals, early intervention & more care in people’s own homes, appropriately supported • Continuing redesign to increase care away from hospital settings – more to do • Investment in primary & community buildings • Sustained commitment to Midland Metropolitan Hospital (MMH) • Examples of joint working e.g. strategic models of care but more joining up needed • Higher number of people requiring outpatient appointments than planned Changes to Services Examples: • Fatigue, anxiety and breathlessness clinic (FAB) • iCARES service • Diabetes Community Care Extension (DICE) team • Modality (formerly Vitality) Health Hub Changes affecting health & social care National: • 2012 NHS reorganisation – PCTs replaced by CCGs, Public Health move to Council • Less money in Public sector: significant Local Authority budget cuts, NHS QIPP/CIP to balance books • Joining up health & social care, services available Monday to Sunday • NHS funding for GP buildings & equipment • Mental Health patients having right crisis services, and both their mental and physical health needs met (Crisis Care Concordat, Parity of Esteem) • Drive for new models of care and GP organisations (NHS Five Year Forward View) • Primary Care co-commissioning – CCG responsibility for performance of services provided by GPs • 2014 Care Act – Better Care Fund Changes affecting health & social care Local: • Organisations working together i.e. Unit of Planning, Provider alliances, West Midlands Combined Authority • New hospital go ahead by January 2016, known time to grow ‘out of hospital’ services • Vitality and Mental Health Alliance for Excellence, Resilience, Innovation and Training (MERIT) “vanguard” areas • Funding for some of the primary/community care buildings no longer available after 2012 • Managing mental health patients differently 0-25 year old and over 25 years mental health provision (April 2016) • Increase in secondary mental health demand with increase in challenging behaviour • New partner organisations and Executive leads • SWBH 2020 vision – adopting the National Voices definition of integrated care • Person-centred, co-ordinated care • “I can plan my care • with people who work together • to understand me and my carer(s), • allow me control, • and bring together services • to achieve the outcomes important to me” (National Voices) What partners are working together on Joining up health and social services with professionals working differently around individuals – to do what’s right for patients/citizens Improving the impact of care on individuals (& their families/carers) Providing high quality care in people’s own homes or closer to home……..where care has to be provided in buildings elsewhere, ensuring the environment is modern, safe and accessible Delivering the Midland Metropolitan Hospital (October 2018) Creating a healthier place to live – better neighbourhood, jobs, local business opportunities, better education, happier more prosperous people Engaging and educating individuals about their own care to improve efficiency, health and wellness Get the most out of money available Action Areas • Continued work by partners to support the new hospital • Need to increase focus on what’s available ‘out of hospital’, including: – Ensuring GP referrals are made at the right time – Turn as much care to planned care e.g. GPs, community services and patients working together to manage their long term conditions better – Establish easy to understand, joined up urgent care services – Ensuring patients can leave acute hospital care at the earliest opportunity, and are supported to minimise their return • Partners need to understand & deliver its contribution – how changes will be delivered & resourced • Need to work out how the new models of care fit • Partners need to stick to agreed RCRH principles – openness, transparency, shared understanding, holding to account • Joint working to make sure no partner ‘falls over’ And key to all this……. …….Re-engaging you, our local people, involving them, providing assurance & sharing information regarding changes to services Any thoughts or questions? Thank you angela.poulton@nhs.net Telephone: 07872 055064