revised version from 6/7/2010

A Self Study of the Master of Public Health Program
University of Nevada, Reno
Submitted In Partial Fulfillment of Requirements for Accreditation to the Council on Education for Public Health
Contact Persons:
Paul G. Devereux, PhD, MPH, Associate Professor,
Lead, Self-Study Committee,
775-692-7080 devereux@unr.edu or
Trudy Larson, MD, Interim Director,
775-682-7103 tlarson@medicine.nevada.edu
School of Community Health Sciences
UNR Mailstop 274
1664 N. Virginia Street
Reno, NV 89557-0034
October 2010
UNR School of Community Health Sciences
Table of Contents
1.0 The Public Health Program ............................................................................................4
1.1 Mission ...........................................................................................................................4
1.2 Evaluation and Planning ................................................................................................9
1.3 Institutional Environment ............................................................................................18
1.4 Organization and Administration .................................................................................25
1.5 Governance ..................................................................................................................29
1.6 Resources .....................................................................................................................35
2.0 Instructional Programs .................................................................................................49
2.1 Master of Public Health Degree ...................................................................................49
2.2 Program Length ...........................................................................................................51
2.3 Public Health Core Knowledge ...................................................................................56
2.4 Practical Skills .............................................................................................................58
2.5 Culminating Experience...............................................................................................62
2.6 Required Competencies ...............................................................................................67
2.7 Assessment Procedures ................................................................................................73
2.8 Academic Degrees .......................................................................................................80
2.9 Doctoral Degree ...........................................................................................................81
2.10 Joint Degrees ..............................................................................................................82
2.11 Distance Education or Executive Degree Programs ..................................................85
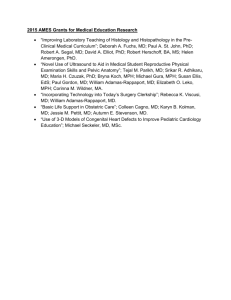
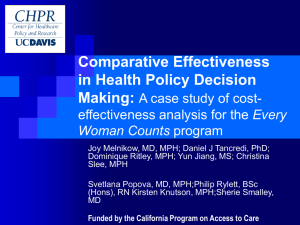
3.0 Creation, Application and Advancement of Knowledge .............................................86
3.1 Research .......................................................................................................................86
3.2 Service..........................................................................................................................98
3.3 Workforce Development ............................................................................................106
4.0 Faculty, Staff and Students ........................................................................................115
4.1 Faculty Qualifications ................................................................................................115
4.2 Faculty Policies and Procedures ................................................................................127
4.3 Faculty and Staff Diversity ........................................................................................131
4.4 Student Recruitment and Admissions ........................................................................140
4.5 Student Diversity .......................................................................................................146
4.6 Advising and Career Counseling ...............................................................................152
Final Self Study, October 2010 Page 2
UNR School of Community Health Sciences
List of Appendices
MPH Program Review Report ............................................................................................ A
Asset and Opportunities Inventory .................................................................................... B
MPH Internship Memorandum of Understanding .............................................................. C
MPH Professional Paper Approval Form ........................................................................... D
Core Course Competency Plans & Assessment Data ......................................................... E
Matrix of Core Competencies ............................................................................................. F
Epidemiology Competencies & Assessment Data .............................................................. G
Matrix of Epidemiology Competencies .............................................................................. H
Social & Behavioral Health Competencies & Assessment Data ......................................... I
Matrix of Social & Behavioral Competencies ..................................................................... J
Evaluation Tool Professional Paper & Presentation ........................................................... K
Forum for Healthy Nevada ................................................................................................. L
SCHS Bylaws..................................................................................................................... M
MPH Student Handbook ..................................................................................................... N
Final Self Study, October 2010 Page 3
UNR School of Community Health Sciences
1.0 The Public Health Program
1.1 Mission. The program shall have a clearly formulated and publicly stated mission with supporting goals and objectives. The program shall foster the development of professional public health values, concepts and ethical practice.
1.1.a. A clear and concise mission statement for the program as a whole.
The mission of the MPH program is to develop, disseminate, and apply knowledge with an ecological approach to protect and promote the health of populations statewide and worldwide.
This is also the mission of the School of Community Health Sciences (SCHS), Division of
Health Sciences (DHS), University of Nevada, Reno (UNR) in which the program is located.
The program mission is congruent with the missions of the univeristy and Division of Health
Sciences. The mission of the Division is to contribute to the advancement and dissemination of knowledge that will help to improve society at the state, regional, and national levels. The
Division of Health Sciences is tied together by the need to find solutions for and help people towards improving their health and well-being through education, research, clinical care, and public service. Through one-on-one treatment of people with health problems, providing opportunities to participate in medical and social behavioral research, and conducting scholarly activities aimed at improving the health and well-being of whole populations, faculty prepare and teach students to work in high-demand professions.
The University of Nevada, Reno is a constitutionally established, land-grant university. The university served the state of Nevada as its only state-supported institution of higher education for almost 75 years. In that historical role, it has emerged as a doctoral-granting university which focuses its resources on doing a select number of things well. The University of Nevada, Reno offers a wide range of undergraduate and graduate programs, including selected doctoral and professional studies, which emphasize those programs and activities which best serve the needs of the state, region, and nation. By fostering creative and scholarly activity, it encourages and supports faculty research and application of that research to state and national problems.
Areas in which the mission of the University of Nevada, Reno are especially relevant for the
MPH program include the resolve to: emphasize undergraduate, graduate, and professional programs which meet the needs of the citizens of Nevada; offer a range of applied, interdisciplinary and career-oriented programs at both the undergraduate and graduate levels; provide community and public service programs through continuing education and cooperative extension; contribute to the advancement and dissemination of knowledge that will help to improve society at the state, regional, and national levels; reflect and respect the rich ethnic and cultural diversity of the citizens of Nevada in its academic programs, support programs, and in the composition of its faculty, administration, staff and student body; and, enhance the research and public service capabilities of the university through increased collaboration with both the public and the private sectors, and by providing assistance to the state and local governments.
Final Self Study, October 2010 Page 4
UNR School of Community Health Sciences
1.1.b. One or more goal statements for each major function by which the program intends to attain its mission, including instruction, research and service.
The goals of the MPH Program and SCHS are:
To prepare future public health practitioners, researchers, educators and leaders
To develop the knowledge base for public health through research
To be recognized for leadership in innovative approaches to public health
To engage with multiple communities through professional and scholarly service
To expose students to diversity in multiple venues
1.1.c. A set of measurable objectives relating to each major function through which the program intends to achieve its goals of instruction, research and service.
Table 1.1.c. Listing of SCHS Goals and Objectives.
1) Goal: “To prepare future public health practitioners, researchers, educators and leaders.”
Objective 1): Recruitment/Admissions
1a. By 2011, 80% of students enrolled in the MPH program will have an overall undergraduate
GPA that exceeds 3.2.
1b. By 2011, 40% of students enrolled in the MPH program will have a standardized test score
(GRE, MCAT) that exceeds the 50th percentile.
Objective 2): Education/Training
2a. By 2011, 90% of MPH students will receive grades of B or higher as evidence of partial attainment of core MPH and emphasis-specific competencies.
2b. By 2011, 95% of MPH students will receive approval of their culminating project proposal by their committee on the first attempt.
2c. By 2011, 30% of MPH students will be involved with faculty in research activities.
2d. By 2011, 10% of current MPH students or graduates within the last 5 years will be the primary author or a co-author on a publication (peer-reviewed).
2e. By 2011, 20% of current MPH students or graduates within the last 5 years will be the primary author or a co-author on a presentation at a scientific conference (peer-reviewed).
2f. By 2011, 35% of MPH students will be involved in leadership roles and providing service to the community or university.
Objective 3): Graduation/Post-Graduation
3a. By 2011, 90% of full-time MPH students will complete their degree within 3 years of matriculation.
3b. By 2011, 75% of MPH graduates will become employed in public health or settings closely related to their degree within 6 months of graduation.
3c. By 2011, 5% of MPH graduates will be admitted to a program for further academic training
(PhD, MD, etc.).
3d. By 2011, 10% of MPH graduates will have local or national leadership positions in public health.
3e. 60% of employed UNR MPH graduates are located in Nevada and the Intermountain West by
2011.
Final Self Study, October 2010 Page 5
UNR School of Community Health Sciences
2) Goal: “To develop the knowledge base for public health through research.”
Objectives:
1.
At least 60% of faculty will publish an article in a peer-reviewed journal by 2011.
2.
At least 70% of faculty will present research results at a conference by 2011.
3.
At least 70% of faculty will submit one proposal for grant funding by 2011.
4.
External funding per FTE will increase 10% by 2011.
3) Goal: “To be recognized for leadership in innovate approaches to public health.”
Objectives:
1.
At least 25% of faculty holding positions on advisory boards, review panels, study sections, editor positions, and other influential bodies by 2015.
2.
30% of faculty will share health-related information with community or media by 2011.
4) Goal: “To engage with multiple communities through professional and scholarly service.”
Objectives:
1.
By 2011, 40% of faculty will co-author reports and publications with colleagues at other units on campus.
2.
By 2011, 30% of faculty will co-author reports, publications, and presentations with community members.
3.
By 2011, 15% of faculty will provide workshops, trainings and continuing education opportunities to public health professionals.
4.
By 2011, 15% of faculty will provide technical assistance to the community, including but not limited to, program evaluations, consulting, data analysis, grant partnerships.
5.
By 2011, 10% of UNR faculty is members of community boards or committees.
6.
By 2011, 10% of UNR SCHS committee composition will be community members.
5) Goal: To expose students to diversity in multiple venues.
Objectives:
1.
Faculty and staff are representative of women, underrepresented minority, and other diverse groups in the relevant labor markets by 2015.
2.
By 2011, efforts to recruit underrepresented populations for the MPH program will increase by 10%.
3.
Efforts to recruit diverse faculty and staff will increase by 5% for each new hire.
4.
By 2011, historically underrepresented racial/ethnic populations will comprise 20% of the students enrolled in the MPH program.
5.
By 2011, 20% of MPH applicants will report experience working with underrepresented populations.
6.
By 2011, 50% of faculty address issues affecting underrepresented populations in their work.
1.1.d. A description of the manner in which mission, goals and objectives are developed, monitored and periodically revised and the manner in which they are made available to the public.
The mission and goals have been reviewed nearly every year since the formation of the MPH program in 2000 and revised as needed. The faculty hold school-wide retreats twice a year at the beginning of each semester. Strategic planning, which includes reviewing our goals and mission, typically occurs during these meetings. Measureable objectives tied to the mission and values were first developed in SCHS faculty subcommittees. The drafts were then presented to all
Final Self Study, October 2010 Page 6
UNR School of Community Health Sciences program faculty who voted to adopt the final list of objectives in the fall of 2009. The process of developing measurable objectives will allow for a stronger tie in to our goals, concrete feedback, and a better evaluation process to occur at our fall 2010 retreat.
The mission, goals, and objectives are made available on the school’s website and in program materials, such as those distributed to community partners and in the school’s bylaws. They are included in the students’ handbook available on the website and distributed to students at new student orientation.
The faculty efforts and accomplishments are monitored through the use of Digital Measures, an online effort reporting system that faculty complete each year which captures accomplishments in service, teaching, and research. Objectives related to students are measured most commonly through surveys and instructor records.
1.1.e. A statement of values that guide the program, with a description of how the values are determined and operationalized.
The program’s values reflect what guides our work as a faculty, school and our interactions with the community and what actions we want to model to our students and other stakeholders.
Values of the School of Community Health Sciences
• Professionalism
• Integrity
• Diversity
• Community and Collaboration
• Advancement of Knowledge and Learners
The values were determined by a vote of faculty and MPH students in fall 2009. The same five values were chosen separately by the students and faculty. The primary way we have operationalized our values is in the development of our goals and objectives. Table 1.1.e. maps our values to our goals and objectives.
Table 1.1.e. Operationalization of SCHS Values to SCHS Goals and Objectives.
Value Corresponding Goal/Objective
Professionalism Goal 1; Obj. 1.a, 1.b, 2.c.-f., 3b.-e., Goal 2;
Obj. 1-4; Goal 3; Obj. 1-2; Goal 4; Obj.
1,3,4; Goal 5; Obj.1,3,6
Integrity
Diversity
Community and Collaboration
Advancement of Knowledge and Learners
Goal 3; Goal 5; Obj. 2-3, 5
Goal 4; Obj. 6; Goal 5; Obj. 1-6
Goal 1; Obj. 2.c.-f., 3d., Goal 3; Obj. 1-2,
Goal 4; Obj.1-6; Goal 5; Obj.5-6
Goal 1; Obj. 1.a, 1.b, 2.a.-f., 3a.-e., Goal 2;
Obj. 1-4; Goal 3; Obj. 2; Goal 4; Obj. 1-4,
Goal 5; Obj.5-6
Final Self Study, October 2010 Page 7
UNR School of Community Health Sciences
Our values are embedded in our mission statement, discussed at our faculty retreats and faculty meetings, displayed in our building and classrooms, and reflected in our curriculum, our commitment to the community and to the univesity. To increase the saliency of our values it was decided after a faculty-wide discussion that we would each provide a reflective statement in our yearly faculty and staff evaluations beginning in 2010 in we respond to the question “During the last year, in which ways have you supported the school’s values?”
1.1.f. Assessment of the extent to which this criterion is met.
This criterion is met.
Strengths
Our mission, values, goals and objectives were developed with broad support among faculty and students.
Suggested Improvements
Measureable objectives are a new process for the school and they will require careful monitoring especially in the next couple years to ensure that they are measured appropriately and revised as needed.
The program should consider identifying more teaching-related objectives. For example, our analysis has revealed an emphasis on research and student-related objectives rather than what we do in the classroom. This omission has been brought to the attention of the
Steering Committee for further discussion and development of a plan with assessment for teaching objectives within the program.
The program should begin to establish a process in which more stakeholders are involved in the development and review of goals and objectives. Involving our Advisory Board has been chosen as the first step in this effort. It is in concert with our Advisory Board that most appropriate stakeholders are involved in this development and review of goals and objectives.
Final Self Study, October 2010 Page 8
UNR School of Community Health Sciences
1.2 Evaluation and Planning. The program shall have an explicit process for evaluating and monitoring its overall efforts against its mission, goals and objectives; for assessing the program’s effectiveness in serving its various constituencies; and for planning to achieve its mission in the future.
1.2.a. Description of the evaluation procedures and planning processes used by the program, including an explanation of how constituent groups are involved in these processes.
Based on a thorough needs assessment in 1999 which demonstrated strong support for an MPH program among health professionals within a 45-mile radius of the university, a lack of public health training among existing professionals in Nevada, and few MPH programs in the
Intermountain West, UNR’s MPH program was designed and launched to meet a clearly demonstrated need in the state.
Since that time, the MPH program has undertaken numerous planning efforts. In 2003, as a result of a strategic planning process to address the state’s needs, plans were launched to develop a full
School of Public Health at UNR which was approved by the Nevada State Board of Regents in
2004. However, due to budget constraints that were slowing the progress of a full school, in spring 2008, faculty decided to delay the development of the School of Public Health and to pursue the advancement of the MPH program.
The Nevada Code of Higher Education requires that all departments undergo periodic review and the program complies with university planning and evaluation procedures. The school conducts program reviews every couple years and most recently completed a review of the MPH program in spring 2009 (see Appendix A). The review included site visits from other faculty at other graduate public health programs and input from students and community stakeholders. The school collaborates with UNR’s Office for University Assessment (OUA) which conducts the yearly employer and MPH alumni surveys. In addition to formal reviews at the university level, the bi-yearly school faculty retreats are the primary site for program planning and evaluation.
For example, the measureable program objectives developed in fall 2009 will be reviewed at the faculty retreat in fall 2010.
The school has actively engaged the community and key public health stakeholders to provide input to guide improvements since it began plans to offer an MPH. The original committee to explore the feasibility of a UNR MPH program consisted of students, faculty from medicine and other related departments (nutrition, nursing, aging), and eight state and county health professionals. Alumni and employer surveys are conducted each year and in 2006, a needs assessment of Nevada State Health Division staff (see Section 3.3.a.), demonstrated continued support for public health education and training.
Another way in which community constituents participate in program planning is by their involvement in the MPH students’ and school committees. In particular, the school’s advisory board consists of public health professionals from the region (including program alumni). In addition, the school’s affiliate and adjunct faculty include community members.
Student representatives attend the monthly MPH Graduate Committee meetings. Students provide feedback on all aspects of the MPH program through communication with their
Final Self Study, October 2010 Page 9
UNR School of Community Health Sciences instructors, advisors, and the graduate program director. Particular feedback from students is obtained each semester about their courses, instructors, and internship preceptors. The internship preceptors also evaluate the student and the amount of support received from program faculty.
The graduate program director serves as the program’s assessment coordinator with input and guidance provided by the graduate and steering committees. The faculty and graduate committees meet monthly. The steering committee meets regularly, typically once a month.
1.2.b. Description of how the results of evaluation and planning are regularly used to enhance the quality of programs and activities.
The program continually uses evaluation results to improve the quality of the program and activities. The most typical feedback source is information from alumni surveys. This information has been used to revise the curriculum, such as adding or removing particular courses. For example, the alumni feedback showed that there was redundancy in a course designed to introduce students to the field of public health with other core courses and a lack of research methods in the curriculum. As a result Community Health Sciences (CHS) 700
“Introduction to Public Health” was replaced by CHS 700R “Research Methods for Public
Health”. In other cases, internship sites have been discontinued based on student feedback about the preceptor or site. In fall 2009, the graduate committee approved adding a question to the
2010 alumni survey to ask about leadership activities to better capture information on alumni leader positions, which is one of the school’s outcome objectives.
Planning processes with stakeholders led to the development of the dual MPH/MD and the removal of the nutrition emphasis which lacked student participation. Feedback from students and alumni was also used to support revisions to the dual MSN in nursing/MPH degree. These revisions are currently occurring and therefore, students will not be admitted into the dual
MSN/MPH program until the curriculum is updated.
As part of the development plans for a full School of Public Health, a SWOT analysis was conducted in October 2007 (see Appendix B). Although the development of a full school has been delayed, the planning process produced a number of changes (e.g., identification of the need to hire an internship coordinator).
Finally, in part based on feedback from students, the MPH culminating experience has been changed. In addition to input from the students and faculty who served on the MPH students’ committees, the evidence showed that students’ time-to-degree completion was unnecessarily long, and that the focus of the culminating project was too narrow allowing students to sufficiently demonstrate mastery of only one or just a few competencies. As a result of a review of this review, the culminating experience project was replaced with a 3-credit capstone course in spring 2010.
1.2.c. Identification of outcome measures that the program uses to monitor its effectiveness in meeting its mission, goals and objectives. Target levels should be defined and data regarding the program’s performance must be provided for each of the last three years.
Final Self Study, October 2010 Page 10
UNR School of Community Health Sciences
Table 1.2.c. UNR SCHS MPH Program Goals, Objectives, Targets, and Data for the Last 3 Years.
1) Goal: “To prepare future public health practitioners, researchers, educators and leaders.”
Objective 1): Recruitment/Admissions
2007 to 2008 to 2009 to 2010
Data
1a. By 2011, 80% of students enrolled in the MPH program will have an overall undergraduate
GPA that exceeds 3.2.
1b. By 2011, 40% of students enrolled in the MPH program will have verbal and quantitative
GRE scores that exceed the 50 th
percentile.*
Objective 2): Education/Training
53%
31%
67%
33%
70%
47%
2a. By 2011, 90% of MPH students will receive grades of B or higher as evidence of partial attainment of core MPH and emphasis-specific competencies.
2b. By 2011, 95% of MPH students will receive approval of their culminating project proposal by their committee on the first attempt.
2c. By 2011, 30% of MPH students will be involved with faculty in research activities.
2d. By 2011, 10% of current MPH students or graduates within the last 5 years will be the primary author or a co-author on a publication
(peer-reviewed).
2e. By 2011, 20% of current MPH students or graduates within the last 5 years will be the primary author or a co-author on a presentation at a scientific conference (peer-reviewed).
92%
New objective: data not yet available
14%
8%
11%
Final Self Study, October 2010
84%
New objective: data not yet available
21%
5%
13%
86%
New objective: data not yet available
22%
12%
13%
Page 11
UNR School of Community Health Sciences
1) Goal: “To prepare future public health practitioners, researchers, educators and leaders.”
Objective 2): Education/Training cont’d
2f. By 2011, 35% of MPH students will be involved in leadership roles and providing service to the community or university.
Objective 3): Graduation/Post-Graduation
3a. By 2011, 90% of full-time MPH students will complete their degree within 3 years of matriculation.
2007 to
100%
71%
3b. By 2011, 75% of MPH graduates will become employed in public health or settings closely related to their degree within 6 months of graduation.
3c. By 2011, 5% of MPH graduates will be admitted to a program for further academic training (PhD, MD, etc.).
3d. By 2011, 10% of MPH graduates will have local or national leadership positions in public health.
3e. 60% of employed UNR MPH graduates are located in Nevada and the Intermountain West by 2011.
2) Goal: “To develop the knowledge base for public health through research.”
Objectives:
1.
At least 60% of faculty will publish an article in a peer-reviewed journal by 2011.
Final Self Study, October 2010
92%
8%
15%
75%
2007 to
75%
2008 to
90%
2009 to 2010
Data
73%
75%
*Historical graduation rate is 80%.
Three years have not yet elapsed for this cohort.
57%
N/A
*This cohort just entered in fall 2009.
Data not yet available
29%
14%
86%
2008 to
71%
Data not yet available
Data not yet available
Data not yet available
2009 to 2010
Data
63%
Page 12
UNR School of Community Health Sciences
2) Goal: “To develop the knowledge base for public health through research.”
Objectives: cont’d
2.
At least 70% of faculty will present research results at a conference by 2011.
3.
At least 70% of faculty will submit one proposal for grant funding by 2011.
4.
Number of new external fund awards and amount of awards per FTE will increase 5% by
2011.
(2006-2007 Baseline: 3 faculty received grants
Total amount = $261,090 = $18,649 amount/faculty FTE)
3) Goal: “To be recognized for leadership in innovative approaches to public health.”
Objectives:
1.
At least 25% of faculty holding positions on advisory boards, review panels, study sections, editor positions, and other influential bodies by
2015.
Objectives:
2.
30% of faculty will share health-related information with community or media by
2011.
4) Goal: “To engage with multiple communities through professional and scholarly service.”
Objectives:
1.
By 2011, 40% of faculty will co-author reports and publications with colleagues at other units on campus.
2007 to
88%
69%
31%
$187,299 per faculty
FTE
>5% increase
2007 to
39%
17%
2007 to
56%
Final Self Study, October 2010
2008 to
71%
71%
43%
$92,312 per faculty FTE
44%
$84,671 per faculty FTE
2008 to
38%
19%
2008 to
21%
2009 to 2010
Data
59%
75%
2009 to 2010
21%
37%
2009 to 2010
31%
Page 13
UNR School of Community Health Sciences
4) Goal: “To engage with multiple communities through professional and scholarly service.”
Objectives: cont’d
2.
By 2011, 30% of faculty will co-author reports, publications, and presentations with community members.
3.
By 2011, 15% of faculty will provide workshops, trainings and continuing education opportunities to public health professionals.
4.
By 2011, 15% of faculty will provide technical assistance to the community, including but not limited to, program evaluations, consulting, data analysis, grant partnerships.
5.
By 2011, 10% of UNR faculty is members of community boards or committees.
6.
By 2011, 10% of UNR SCHS committees will include a community member.
5) Goal: To expose students to diversity in multiple venues.
Objectives:
1.
Faculty and staff are representative of women, underrepresented minority, and other diverse groups in the relevant labor markets by 2015.
Relevant Labor Markets Targets:
Women
Faculty:54%
Staff: 46%
Minority
Faculty:16%
Staff: 21%
2007 to
25%
17%
22%
56%
N/A
2007 to
Women:
Faculty:
50%
Staff: 67%
Minority
Faculty:
17%
Staff: 50%
2008 to
36%
19%
25%
63%
N/A
2008 to
2009 to 2010
35%
32%
32%
47%
17%
2009 to 2010
Women
Faculty:
56%
Staff: 100%
Minority
Faculty:
19%
Staff: 25%
Women
Faculty: 65%
Staff: 83%
Minority
Faculty: 15%
Staff: 50%
Final Self Study, October 2010 Page 14
UNR School of Community Health Sciences
5) Goal: To expose students to diversity in multiple venues.
Objectives: cont’d
2.
By 2011, efforts to recruit underrepresented populations for the MPH program will increase by 10%.
2007 to
1 effort
2008 to
1 effort
2009 to 2010
2 specific efforts
(participation in diversity recruitment fairs)
3.
Efforts to recruit diverse faculty and staff will increase by 5% for each new hire.
4.
By 2011, historically underrepresented racial/ethnic populations will comprise 20% of the students enrolled in the MPH program.
5.
By 2011, 20% of MPH applicants will report experience working with underrepresented populations.
6.
By 2011, 50% of faculty address issues affecting underrepresented populations in their work.
7.
By 2011, 20% of MPH applicants will report experience working with underrepresented populations.
No Search
13%
100%
50%
100%
No Search
25%
90%
59%
90%
3 specific efforts
4%
73%
58%
73%
8.
By 2011, 50% of faculty address issues affecting underrepresented populations in their
50% 59% 58% work.
*N = those students with GRE scores. A few students complete other entrance exams (e.g., MCAT, LSAT).
Final Self Study, October 2010 Page 15
UNR School of Community Health Sciences
1.2.d. An analytical self-study document that provides a qualitative and quantitative assessment of how the program achieves its mission, goals and objectives and meets all accreditation criteria, including a candid assessment of strengths and weaknesses in terms of the program’s performance against the accreditation criteria.
This self study is hereby submitted in compliance with Criterion 1.2.d.
1.2.e. An analysis of the program’s responses to recommendations in the last accreditation report (if any).
Not Applicable
1.2.f. A description of the manner in which the self-study document was developed, including effective opportunities for input by important program constituents, including institutional officers, administrative staff, teaching faculty, students, alumni and representatives of the public health community.
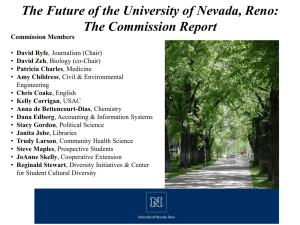
The self study was developed in partnership with the community, faculty, and students. The primary committee was comprised of Paul Devereux, Chair, Self-Study, SCHS faculty, Dana
Loomis, former SCHS Director, Richelle O’Driscoll, representative from the Division of Health
Sciences, William Cathey, Vice Provost, Instruction and Undergraduate Programs at UNR, Kim
Somma Mueller MPH Student, Ginger Fenwick, Center for Ethics & Health Policy, Division of
Health Sciences, Karla Bee MPH Student and Aliya Buttar MPH Student. The committee was designed in response to feedback from a site visit from Mollie Mulvaney, CEPH in spring 2009 and from the CEPH Accreditation Workshop in July 2009.
All school faculty were involved in writing the self-study. Subcommittees were formed to address each self-study section. Faculty also reviewed and edited self-study sections written by others. In addition, the complete list of suggested improvements from each self-study section was distributed separately to faculty so that identified areas for improvement could be used in planning.
The draft was be placed on WebCampus, an online community, for students to review,
Sharepoint, a shared network which faculty and staff can access, and on the program’s website for community input. It will be sent to alumni who requested a copy to review. The school’s
Advisory Board was sent a copy and provided input on the draft before final submission to
CEPH. Finally, Patty Charles, DrPH, MPH, SCHS Affiliate Faculty and Professor at the School of Medicine agreed to provide a review of the document.
1.2.g. Assessment of the extent to which this criterion is met.
This criterion is met.
Strengths
The school has an explicit plan for monitoring its efforts towards its mission, goals, and objectives.
The school seeks input from students and other stakeholders in its planning process.
The school uses evaluation data to inform its course.
Final Self Study, October 2010 Page 16
UNR School of Community Health Sciences
Suggested Improvements
Resources and more structure are needed to ensure successful future planning efforts. To that end, the school’s Center for Program Evaluation has agreed to direct the yearly evaluation of the school’s objectives, graduate, and undergraduate assessments.
Final Self Study, October 2010 Page 17
UNR School of Community Health Sciences
1.3 Institutional Environment . The program shall be an integral part of an accredited institution of higher education.
1.3.a. A brief description of the institution in which the program is located, along with the names of accrediting bodies (other than CEPH) to which the institution responds.
The Graduate Program in Public Health is housed in the School of Community Health Sciences
(SCHS), a unit of the Division of Health Sciences of the University of Nevada, Reno.
The University of Nevada, Reno is a constitutionally established, land-grant university. The university is classified by the Carnegie Foundation for the Advancement of Education as a
Comprehensive Doctoral institution with medical and/or veterinary medicine. Within the university, nine colleges offer wide range of undergraduate and graduate majors. Graduate-level training and research, including a number of doctoral-level programs enhance the uiversity's mission to create scholarly activity.
Nevada is one of the top 120 universities in America for funded research, according to the
Carnegie Foundation. With more than $80 million in research expenditures, a figure that has almost doubled over the past 10 years, the University is the leading research enterprise in
Nevada's higher-education system.
The Division of Health Sciences (DHS) includes the Schools of Medicine, Nursing, Social Work and Community Health Sciences, as well as several free-standing centers. Its chief administrative officer is the Vice President for Health Sciences (VPHS). The VPHS position is currently vacant. A national search for this position is in progress and an acting replacement has been named for the health sciences units, Trudy Larson, MD, is Interim Director of the School of
Community Health Sciences. The Director reports to the Vice President for Health Sciences; level of authority and reporting lines are equivalent to those of the Directors of the schools of nursing and social work. Dr. Larson has standing bi-weekly meetings with the vice president and may communicate directly with him whenever needed.
The University of Nevada, Reno is accredited by the Northwest Commission on Colleges and
Universities, recognized by the Council for Higher Education Accreditation and the U.S.
Department of Education. The university has been accredited since 1938. On January 28, 2008, the university received a letter from the NWCCU which reaffirmed its accreditation on the basis of the fall 2007 Comprehensive Evaluation report.
In addition to the Northwest Commission institutional accreditation, there are numerous university programs which are accredited by their national professional accrediting organizations. These specialized accrediting organizations, which are recognized by the Council for Higher Education Accreditation, are shown below:
Accreditation Board for Engineering and Technology, Inc. (for selected programs in engineering and mines)
Association to Advance Collegiate Schools of Business
American Dietetics Association Commission on Accreditation for Dietetics Education
Final Self Study, October 2010 Page 18
UNR School of Community Health Sciences
Council on Academic Accreditation in Audiology and Speech-Language-Hearing
Pathology, American Speech-Language-Hearing Association
Accrediting Council on Education in Journalism and Mass Communication
American Psychological Association
Council for Accreditation of Counseling and Related Educational Programs
Commission on Collegiate Nursing Education
Council on Social Work Education
Liaison Committee on Medical Education (U.S. Department of Education -recognized accrediting body for programs leading to the M.D. degree in the United States)
National Association of Schools of Music
National Council for Accreditation of Teacher Education
1.3.b. One or more organizational charts of the university indicating the program’s relationship to the other components of the institution, including reporting lines.
Organizational charts for the University of Nevada, Reno and the Division of Health Sciences are shown in Figures 1.3.b.1. and 1.3.b.2.
Figures 1.3.b.1. UNR Organizational Chart.
Final Self Study, October 2010 Page 19
UNR School of Community Health Sciences
Final Self Study, October 2010 Page 20
UNR School of Community Health Sciences
Figure 1.3.b.2. Division of Health Sciences Organizational Chart.
DIVISION OF HEALTH SCIENCES
1.3.c. A brief description of university practices regarding: Lines of accountability, including access to higher-level university officials; Prerogatives extended to academic units regarding names, titles and internal organization; Budgeting and resource allocation, including budget negotiations, indirect cost recoveries, distribution of tuition and fees and support for fund-raising; Personnel recruitment, selection and advancement, including faculty and staff; Academic standards and policies, including establishment and oversight of curricula.
1.3.c.1. Lines of accountability, including access to higher-level university officials. The
University of Nevada, Reno has clear lines of reporting as shown in 1.3.b. The president is the university’s chief executive, with ultimate decision-making responsibility for all aspects of the institution. The Executive Vice President and Provost reports directly to the president and is the university’s chief academic officer. Other aspects of university operations, such as administration and finance, information technology, development, student services and sponsored research are the responsibility of several vice presidents (see 1.3.b). The academic
Final Self Study, October 2010 Page 21
UNR School of Community Health Sciences portion of the university is divided into colleges defined along subject-matter lines. Each college is headed by a dean who reports to the Provost (see 1.3.b). Departments are grouped within colleges and department chairs report to their respective deans. In general, departments are the fundamental academic units of the university.
The University’s Division of Health Sciences departs from this general structure, however (see
1.3.b). The division, which includes the Schools of Medicine, Nursing, Community Health
Sciences and Social Work is headed by the Vice President for Health Sciences (VPHS; for fall
2010, this position is currently occupied by an Interim Dean while a search for a replacement is occurring), who has a direct reporting line to the president, as well as to the provost. Because of this reporting line, the division can be seen as a higher administrative unit than the colleges. The
Dean of the School of Medicine and the Directors of the Schools of Nursing, Community Health
Sciences and Social Work all report to the VPHS. Schools that have directors, rather than a dean, are regarded as intermediate units with attributes of both colleges and departments.
The vice presidents and deans interact regularly with the president and provost. Chairs of academic departments relate primarily to the deans of their colleges, while in the Division of
Health Sciences, directors of schools interact in a similar way with the VPHS. In most situations, the deans and the VPHS represent the departments and schools to higher administrators.
However, school directors may communicate with the provost and meet with him when the need arises.
1.3.c.2. Prerogatives extended to academic units regarding names, titles and internal organization. Academic units have considerable autonomy with respect to internal organization. The director of the School of Community Health Sciences has the authority under the school’s bylaws to create internal subunits, name them and to appoint their heads. The position of MPH graduate program director is specifically named in the school’s bylaws, which were drafted by the school’s faculty and have the authority of the bylaws of the division and the university.
Units may also initiate proposals for new names. Name changes that are considered to be cosmetic in nature require internal approval by the division and university courses and curriculum committees, and approval by the Academic Affairs Council of the Nevada System of
Higher Education. Substantive changes must also be approved by the Board of Regents.
1.3.c.3. Budgeting and resource allocation, including budget negotiations, indirect cost recoveries, distribution of tuition and fees and support for fund-raising. The university administration sets the non-grant portion of academic unit budgets in consultation with the deans and vice presidents. Under the university’s funding formula (see 1.6), unit budgets are proportional to the number of instructional faculty. Units also receive 7.25% of indirect costs receipts for grants involving unit faculty. Tuition and fees are not returned directly to the units that generate them, but are part of the pool of funds available to the administration to meet the university’s operating expenses. Fund-raising support is typically provided at the college or division level by specialized development staff.
Final Self Study, October 2010 Page 22
UNR School of Community Health Sciences
1.3.c.4. Personnel recruitment, selection and advancement, including faculty and staff.
Faculty recruitment, selection and advancement are handled primarily at the level of the school and the division. Searches for tenure-track faculty are initiated by the unit and must be authorized by the dean or vice president and the provost. The areas in which new faculty are recruited are determined by the units in consultation with the dean or vice president. When a candidate is selected as a result of a search, the selection is made by the unit and requires approval from the dean or vice president and the provost. There is considerable flexibility in hiring grant-funded, non-tenure track faculty, but approval of the dean or vice president is still required.
Faculty promotion and tenure applications are also initiated by the academic unit following a standard schedule. Applications are reviewed within the unit and subsequently by faculty committees at the college (or division) and university level. Recommendations for promotion and tenure must be approved by the dean or vice president and the provost. Awards of tenure require final approval by the Board of Regents of the Nevada System of Higher Education.
Classified staff positions are governed by the policies and procedures of the Nevada State
Personnel System. Staff hires are initiated by the units, and staff are evaluated within the units according to state personnel policies. The dean or vice president must review and approve staff evaluations but is usually not involved directly.
1.3.c.5. Academic standards and policies, including establishment and oversight of curricula.
Curricula are developed and managed within academic units. Proposals for new curricula and changes to existing ones are reviewed by division and university committees on courses and curricula. Graduate curricula are also reviewed by the University’s Graduate
Council. These internal reviews tend to be concerned primarily with the potential for duplication of courses and programs within the university. Proposals for new majors and new degrees also require approval by the Board of Regents. Unless changes are proposed, oversight of curricula is usually left to the academic units that administer them.
Minimum academic standards for graduate degrees are set by the UNR Graduate School.
Academic units may set additional requirements if they do not conflict with graduate school policies. For example, a unit may establish the number of credits required for a degree, as long as that number is no less than the minimum established by the graduate school.
1.3.d. If a collaborative program, descriptions of all participating institutions and delineation of their relationships to the program.
Not applicable
1.3.e. If a collaborative program, a copy of the formal written agreement that establishes the rights and obligations of the participating universities in regard to the program’s operation.
Not applicable.
Final Self Study, October 2010 Page 23
UNR School of Community Health Sciences
1.3.f. Assessment of the extent to which this criterion is met.
This criterion is met.
Strengths
UNR and Nevada System of Higher Education have a well-established infrastructure within which to develop new programs.
The Division of Health Sciences structure facilitates multidisciplinary teaching and research. Faculty within different departments of the division are focusing on interdisciplinary teams and training, which will have a positive impact on the MPH program.
Suggested Improvements
Greater faculty representation on university committees would enhance engagement with the broader system and promotion of the MPH program.
Final Self Study, October 2010 Page 24
UNR School of Community Health Sciences
1.4 Organization and Administration.
The program shall provide and organizational setting conducive to teaching and learning, research and service. The organizational setting shall facilitate interdisciplinary communication, cooperation and collaboration. The organizational structure shall effectively support the work of the program’s constituents.
1.4.a. One or more organizational charts showing the administrative organization of the program, indicating relationships among its component offices of other administrative units and its relationship to higher-level departments, schools and divisions .
The graduate program in public health is located within the School of Community Health
Sciences (SCHS). A chart depicting the organization of the school and the public health program is given in Figure 1.4.a.
Final Self Study, October 2010 Page 25
UNR School of Community Health Sciences
Figure 1.4.a. Organizational Chart for the SCHS.
Final Self Study, October 2010 Page 26
UNR School of Community Health Sciences
1.4.b.
Description of the roles and responsibilities of major units in the organizational chart.
The school’s chief administrative officer is the director. As described in Section 1.3, the SCHS
Director reports to the Vice President of Health Sciences; his level of authority and reporting lines are equivalent to those of the Directors of the Schools of Nursing and Social Work. The director has standing bi-weekly meetings with the Vice President of Health Sciences and may communicate directly with him whenever needed.
The program is administered by the graduate program director and the school’s graduate committee. The graduate director is chair of the committee, which is composed of 6 members of the graduate faculty. The graduate committee meets monthly and has primary responsibility for establishing, reviewing and monitoring the curriculum and core competencies. The committee also recommends and implements curriculum changes; sets admissions standards for the MPH program; reviews applicants to the program; provides input to faculty searches based upon program needs; and develops materials and strategies for marketing and student recruitment.
Each specialty area is represented by the graduate curriculum coordinator appointed by the school director. In addition to overseeing the curriculum, the coordinator recommends teaching assignments within the respective areas and facilitates communication between the specialty areas, the school director and the graduate committee.
1.4.c. Description of the manner in which interdisciplinary coordination, cooperation and collaboration are supported.
The graduate program director and the graduate committee have primary responsibility for ensuring coordination, cooperation and collaboration among the disciplines that make up the public health program. The graduate director (from social/behavioral health), the graduate curriculum coordinator (from epidemiology), and the graduate committee work together to ensure that the program exposes students both to a broad public health perspective representative of the core public health disciplines and to specialized knowledge within their areas of concentration. The graduate curriculum coordinator and the graduate director are also members of the school’s steering committee. The steering committee typically meets monthly and is specifically charged with facilitating communication and collaboration among the school’s academic programs, both graduate and undergraduate. The undergraduate coordinator is a member as is the Division of Health Science’s Director of Internal/External Relations.
1.4.d. Identification of written policies that are illustrative of the program’s commitment to fair and ethical dealings.
The program’s commitment to fair and ethical dealings is exemplified by the Bylaws of the
School of Community Health Sciences. Section 1.1 of the bylaws states specifically the purpose of the bylaws is “to provide consistency, fairness and equity to school operations.”
1.4.e. Description of the manner in which student grievances and complaints are addressed, including the number of grievances and complaints filed for each of the last three years.
MPH Student Concerns Resolution. The MPH program strives for a professional, collegial relationship with all MPH students. Students are encouraged to follow the University of Nevada,
Reno policies for resolving any concerns – see
Final Self Study, October 2010 Page 27
UNR School of Community Health Sciences http://www.unr.edu/grad/forms/docs/GraduateSurvivalHandbook.pdf
. Our commitment is resolution of issues, and different situations support different methods.
Depending on the type of concern the student may have, there are several options:
If the concern is about a course, students are encouraged to seek assistance first from the course instructor, then from his or her advisor and/or graduate director. If a result is still not satisfactory, the student may seek assistance from the Director of the School of
Community Health Sciences. Beyond that, the route would be to the Vice President for
Health Sciences.
If a concern involves the advisor and/or internship preceptor, the student is encouraged to seek assistance from the graduate director and/or internship coordinator, and finally the director of the school. Again, the route would then be to the Vice President for Health
Sciences.
If a graduate assistant has an issue with their supervisor, the student can come to the graduate director and/or then to the director of the school.
If students have issues with other students, this would be formally handled though the instructor and/or advisor, depending on the situation.
In any case, if a student is not comfortable discussing the issue with the graduate program director, he/she may approach the graduate curriculum coordinator.
Regardless of the issue, an MPH student may choose to meet with and process the issue with the
MPH student representative for their program specialization. We recognize that in some cases,
MPH students may need support in resolving their issue. From that point, the MPH student and student representative can follow the appropriate line of authority process as noted above to work toward resolution.
Communication of the process for conflict resolution has been distributed to our list-serve, posted on the graduate student bulletin board, and also posted on the MPH WebCampus site.
There has been 1 student grievance in the last 3 years.
1.4.f. Assessment of the extent to which this criterion is met.
This criterion is met.
Strengths
The infrastructure is designed to assure ongoing monitoring, collaboration, interdisciplinary teamwork and learning.
Mechanics are in place to facilitate program improvement, such as twice a semester student affairs committee meetings to address possible concerns related to MPH students.
Faculty and students have a set of policies and procedures which assure that they will be treated fairly and to guide them through situations which may require resolution. These policies and procedures have been reviewed and approved by the faculty senate and the upper administration of the university.
Final Self Study, October 2010 Page 28
UNR School of Community Health Sciences
1.5 Governance. The program administration and faculty shall have clearly defined rights and responsibilities concerning program governance and academic policies. Students shall, where appropriate, have participatory roles in conduct of program evaluation procedures, policy-setting and decision-making.
1.5.a.
Description of the Program’s governance and committee structure and processes, particularly as they affect: - general Program policy development - planning - budget and resource allocation - student recruitment, admission and award of degrees - faculty recruitment, retention, promotion and tenure - academic standards and policies - research and service expectations and policies.
School of Community Health Sciences. The governance of the Public Health Program falls under the governance structure of the School of Community Health Sciences, as established in the school’s bylaws under the authority of the bylaws of the Division of Health Sciences and the
University of Nevada, Reno and the Code of the Nevada System of Higher Education (see 1.5.b).
Within the School of Community Health Sciences, the school director is the primary level of governance and final authority. The director is appointed by the president of the university on the recommendation of the vice president for health sciences and the faculty of the school. The faculty constitutes the second level of governance. Rights and responsibilities of the faculty are established by the Bylaws of the University (Chapter III, section 39). Under the bylaws of the school, the faculty provides input regarding policies and procedures. Policy recommendations are developed by standing or ad hoc committees of faculty and brought forward to the director for consideration. The director may also develop policies and procedures needed for the operation of the school. The faculty votes on matters affecting the mission, programming and functioning of the school. Approval by majority vote of the faculty is required for curriculum changes (described below), establishment of new academic programs and centers, appointment of adjunct faculty, and amendment of the bylaws. In other matters, votes of the faculty are advisory to the director. Decisions of the director can be appealed by a majority vote of the faculty, which may petition the Vice President for Health Sciences if resolution cannot be reached internally. The university bylaws provide further mechanisms for resolution of faculty grievances.
The Public Health Program. Policies and procedures for the Graduate Program in Public Health are developed by the SCHS Graduate Program Committee. The graduate committee is established by the Bylaws of the School of Community Health Sciences; its charge and membership are shown in 1.5.c. The graduate program director is chair of the committee, which has 6 other members representing the graduate faculty and the core areas of public health. The committee is required by the bylaws to have at least one member who is a graduate student. The members of the committee and the graduate director are appointed by the school director for 2year terms. Student members typically serve for one academic year.
The graduate committee meets monthly during the academic year and has primary responsibility for establishing, reviewing and monitoring the curriculum and core competencies. Proposals for new courses and curriculum changes must be reviewed and approved by the faculty and director of the school, and subsequently by the Division of Health Sciences Courses and Curriculum
Committee, the University Courses and Curriculum Committee, and Graduate Council. The school has a representative on the Division Courses and Curriculum Committee. The Division, in
Final Self Study, October 2010 Page 29
UNR School of Community Health Sciences turn, has a representative on the university-level committee and the Graduate Council who represents the interests of the School of Community Health Sciences, as well as the other units in the division.
Academic standards, policies and procedures for the public health program are established by the graduate committee, subject to the regulations of the Graduate School. These are disseminated to students in the MPH Student Handbook (see Appendix N) and to faculty in the Handbook for
MPH Advisors. The committee also sets admissions standards for the MPH program, reviews applicants to the program, and develops materials and strategies for marketing and student recruitment. Graduate degrees are awarded by UNR’s Graduate School.
Faculty Recruitment, Retention, Promotion and Tenure. Faculty recruitment, retention, promotion and tenure are managed at the level of the school and the division (with approvals required at the university level). Searches for new faculty are initiated by the school director in consultation with the faculty and standing committees and must be authorized by the Vice
President for Health Sciences and the provost. The specific areas in which new faculty are recruited are prioritized to advance the mission, goals and objectives of the school and the program. Development of the public health program is a high priority in faculty recruitment, and all new tenure-line faculty members are expected to contribute. Searches for new faculty members are conducted by a search committee approved by the director. The search committee is responsible for advertising, interviewing, and recommending candidates to the director, who makes the final selection, with approval by the vice president and provost.
UNR Bylaws require that faculty are evaluated annually for research, teaching and service. At the beginning of each calendar year, faculty submit a role statement listing goals for the year. At the end of the calendar year, faculty submit an annual review document summarizing productivity. Evaluations must include peer review and student evaluations of teaching. Program faculty is evaluated initially by the School of Community Health Sciences Personnel/Promotion
& Tenure Committee, which recommends an evaluation to the director. The director then produces an evaluation report, which takes the committee’s input into account. The director’s report is shared with the faculty member in writing and discussed in a meeting, and is then forwarded to the vice president for review and approval.
Promotion and tenure actions are also initiated within the school. Candidates prepare an application package. This document, along with letters from external referees that have been solicited by the director, is reviewed initially by the Personnel/Promotion & Tenure Committee.
Following the P&T committee’s review, the director makes a written recommendation to the vice president that refers to the recommendation of the committee and the external referees.
Recommendations for promotion and tenure require further approval by the division and university promotion and tenure committees. Awards of tenure must be approved by the Board of Regents of the Nevada System of Higher Education.
Budget and Resources. Financial support for the Graduate Program in Public Health is provided through the budget of the School of Community Health Sciences as described in 1.6. The budget includes lines for salary and operations for the school as a whole. Since the school administers both graduate and undergraduate programs and members of the faculty and staff typically contribute to both at varying levels, the program does not have a separate budget. Resources are allocated to the program through the assignment of faculty and staff to teaching and
Final Self Study, October 2010 Page 30
UNR School of Community Health Sciences administrative functions. These assignments are made by the school director in consultation with the program directors and the steering committee.
Classroom and administrative space is also shared by all of the school’s programs. Office and research space is assigned by the school director according to criteria specified in the bylaws.
Again there is no specific allocation for the public health program, since most faculty are involved in both graduate and undergraduate teaching. However, research conducted in the school’s laboratory space furthers the mission of the graduate program and involves graduate students.
1.5.b. A copy of the constitution, bylaws or other policy document that determines the rights and obligations of administrators, faculty and students in governance of the
Program.
The Bylaws of the School of Community Health Sciences are provided in Appendix M and are available at http://www.unr.edu/facultysenate/bylaws/health-sciences/school-of-communityhealth-sciences-policies-and-procedures-11-25-09.pdf
The rights and responsibilities of administrators and faculty are also governed by the following documents:
Bylaws of the Division of Health Sciences: http://www.unr.edu/healthsciences/documents/DHS.Bylaws.DRAFT_2010.pdf
Bylaws of the University of Nevada, Reno (URL) http://www.unr.edu/facultysenate/bylaws/UNR%20Bylaws/unr-bylaws-11-18-09-2.pdf
Code of the Nevada System of Higher Education (URL) http://system.nevada.edu/Board-of-R/Handbook/TITLE-2---/index.htm
1.5.c. A list of standing and important ad hoc committees, with a statement of charge, composition, and current membership for each.
The standing committees of the school are the Steering Committee (described in 1.4), the
Personnel/Promotion and Tenure Committee, the Undergraduate Program Committee, and the
Graduate Program Committee. The Personnel/Promotion and Tenure committee is charged under school and university bylaws with providing peer review for annual evaluations of faculty performance and for promotion and tenure decisions. The undergraduate and graduate program committees are charged with the management of the undergraduate and graduate academic programs, respectively. The role of the graduate committee in connection with the public health program is described in more detail above. Ad hoc committees may also be formed as needed to complete a specific task or charge. These committees are temporary and are dissolved when their charge is fulfilled. Chairs of all committees are appointed by the school director and actions of committees are advisory to the director and the faculty. The charges and current membership of standing committees is shown in below.
Charge of the Graduate Program Committee. The purpose of the Graduate Committee is to:
“monitor the quality of the graduate program including periodic review of curriculum and assessment of learning outcomes; provide recommendations pertaining to changes, modifications or additions to the graduate curriculum, and recommend action to the SCHS Director; process
Final Self Study, October 2010 Page 31
UNR School of Community Health Sciences graduate applications for admission to the graduate program; develop marketing programs to increase student enrollment in the graduate programs; review applications for Graduate Assistant positions, and make recommendations to SCHS Director; develop an assessment plan, conduct assessment activities, and provide assessment data to the university assessment office; develop competencies and the means to assess the extent to which those competencies are met; conduct regular reviews of curriculum, competencies and assessment results and recommend those changes needed to ensure competencies are met; regularly review accreditation criteria set by
CEPH and other relevant bodies and recommend changes needed to ensure the program meets accreditation requirements.” (Bylaws of the School of Community Health Sciences, section
2.3.3)
2009-2010 Membership of the Graduate Committee
Melanie Minarik, MPH, PhD (Chair)
Michelle Granner, PhD
Kristen Clements-Nolle, MPH, PhD
Jeff Angermann, PhD
Paul Devereux, PhD
School Director (Ex-Officio)
Minggen Lu, PhD
Leslie Elliott, MPH, PhD
Graduate Student Member (beginning fall
2010: 2 graduate student members)
1.5.d. Identification of Program faculty who hold membership on university committees, through which faculty contribute to the activities of the university.
Members of the Program faculty serve regularly on committees at the division and university level, through which they contribute to academic planning, policy-making, personnel evaluation, and other activities. Examples of faculty serving on university and division committees in the last 3 years are listed below.
*Jennifer Bennett: Health Sciences’ Interprofessional Education Committee, 2009-present.
*Marie Boutte, Member, University Promotion & Tenure Committee, 2009-present; Division of
Health Sciences Promotion & Tenure Committee, 2007-08.
*Elizabeth Christiansen: Chair, Division of Health Sciences Bylaws Committee, 2009-10
*Daniel Cook: Chair of Health Care Ethics, Nevada Center for Ethics and Health Policy, 2010.
Scholarships in Aging Awards Committee, spring 2010.
*Paul Devereux: Member, Search Committee, Vice-President of Health Sciences/Dean of
Medical School position; Program Reviewer of Department of Nutrition Graduate Program for
UNR’s Graduate Council, Member, Faculty Senate Grievance Committee for Promotion and
Tenure Review, 2010.
*Dana Loomis: Member, university committee on environmental sustainability 2009-10.
*Judith Sugar, Member, Faculty Senate, 2007-8. Interdisciplinary Gerontology Curriculum
Committee 2007-present.
*Wei Yang, Member, Division of Health Sciences Curriculum Committee, 2009-10.
*Nora Constantino, Member, Steering Committee for Campus Recreation & Wellness 2009present, Collaboration and Communication, DHS 2008-present.
Final Self Study, October 2010 Page 32
UNR School of Community Health Sciences
1.5.e. Description of student roles in governance, including any formal student organizations, and student roles in evaluation of Program functioning.
Graduate Public Health Network : MPH Students have an officially recognized club with the
UNR graduate student association. This allows the students to have organizational capacity, and provides resources to launch special projects, programs, and activities.
Graduate Student Association : The UNR graduate student union has a student government that utilizes student fees to support programs and activities. The health sciences division holds three seats on the council, and MPH students have frequently been elected to these seats. The GSA participates in campus-wide policy and program advocacy on campus.
Community Health Sciences Graduate Student Government: In the past year, MPH students have created a student government structure to address students’ concerns related to academic programs, curriculum, grievances, and professional development. Four offices were created:
Epidemiology Co-Chair, Social and Behavioral Health Co-Chair, First Year Representative, and
Professional Development Representative. Elections for the two Co-Chair and Professional
Development positions are held during the spring semester and the election for the first year representative is held during the fall semester. These procedures have not yet been implemented.
Future students can alter and revise the government structure and election procedures as needed.
Course evaluations : Students complete confidential course evaluations at the end of each semester for all of our courses. The results of these are compiled by school administrative staff and then shared shortly after (1 month or less) with the individual faculty members. Faculty then has this information for self-assessment purposes for the next time they teach the course. In addition, this course information is part of the faculty member’s annual performance review during which the personnel committee will also see the data.
Faculty Teaching : The course evaluation process includes teaching evaluation by the students.
Results are also shared in the same method for review. Faculty also provide peer evaluations of classroom performance.
Graduate Assistantship Evaluations: Each semester, the Graduate Director sends out a confidential survey to student GA’s to get feedback on their experiences under faculty supervision. Results are shared with the graduate committee and faculty supervisors for improvement purposes.
Internship Evaluation : As part of the internship experience, our students are asked several times throughout to evaluate their internship site, their preceptor, and their experiences related to their competencies. Results are then shared with the internship site and preceptor for improvement purposes.
Career Placement Evaluation: Informally, students give us feedback about professional opportunities and needs that they have in regard to career placement. This feedback has prompted us to more closely connect with our professional networks, our alumni, and other programs with career placement services on campus such as, the College of Business. These evaluations are received from students via faculty advisors and direct discussions.
Final Self Study, October 2010 Page 33
UNR School of Community Health Sciences
Graduate Committee: MPH student representatives are members of this committee. They are asked monthly for input on the committee agenda, and they attend the meetings, participate in the discussions and give voice to student issues and needs.
Advisors: Advisors are assigned early in the student’s program of study. There have been instances where students have requested changes for various personal and professional reasons.
Those requests were accommodated. Each advisor receives feedback from students in their individual meetings and the faculty may share this at faculty meetings or at graduate committee meetings.
WebCampus Communication: After pilot-testing networking/communication vehicles, we now use a section of WebCampus for all of our communications with MPH students. It is a convenient tool that allows for 2-way communication between groups and/or individuals. While traditional methods are also utilized (announcements posted on central bulletin boards and sent by e-mails), our standard method is WebCampus, since it is accessible for all students and faculty and regularly used as UNR for various purposes.
Search Committees: In every search for new faculty, MPH students are involved at each stage of the process, providing input and student perspectives about the job description and the selection of candidates. Student participation allows perspective candidates to gain information about our program as well.
MPH Program Review: In 2009 during the MPH program review initiated by the UNR Graduate
School (see Appendix A), students were involved in creating documents, gathering data, reading the documents, and meeting with the external reviewers.
CEPH Self-Study: In this year as we complete the self-study for CEPH, students have participated in each step the process. The self-study requires greater depth and breadth than the
2009 Program Review, and we have enlisted more students in creating our self-study (see
Section 1.2.f.).
1.5.f. Assessment of the extent to which this criterion is met.
This criterion is met.
Strengths
There are numerous avenues for faculty participation in governance both within the
School of Community Health Sciences and across the university.
Policy documents are in place that clearly delineate roles, rights, and responsibilities.
Students actively participate in administering the public health program.
Suggested Improvements
Student involvement in the MPH program needs to increase in depth and scope (e.g., greater representation on other school committees and by more students).
We recognize that our connection with alumni is weak. There are no alumni events or formal mechanism to reach out to them. We therefore plan to create a stronger connection with alumni. As a first step toward this goal, we have recruited two alumni to serve on the school’s advisory board.
Final Self Study, October 2010 Page 34
UNR School of Community Health Sciences
1.6 Resources. The program shall have resources adequate to fulfill its stated mission and goals, and its instructional, research and service objectives.
1.6.a. A description of the budgetary and allocation processes, sufficient to understand all sources of funds that support the teaching, research and service activities of the program.
This should include, as appropriate, discussion about legislative appropriations, formula for funds distribution, tuition generation and retention, gifts, grants and contracts, indirect cost recovery, taxes or levies imposed by the university or other entity within the university, and other policies that impact on the resources available to the program.
The funds that support the MPH Program are provided by the SCHS. The main components of the school’s budget are state funds allocated by the University of Nevada, Reno, grants and contract awards to the school’s faculty, and funds for instructional support and graduate assistantships provided by the Division of Health Sciences and the Graduate School, respectively. The school also receives 7.25% of indirect costs received by the university. Further details of the school’s budget are outlined in section 1.6.b.
The University of Nevada, Reno has total annual revenues of approximately $500 million as shown in the table below for the fiscal year ended June 30, 2009 (the most recent data available).
Table 1.6.a.
Revenue sources, University of Nevada, Reno (data for fiscal year ended
June 30, 2009).
Source
Total revenue
State appropriations
Tuition & fees
Grants & contracts
Amount ($ x 1000)*
512,548
200,432
77,710
150,141
Percent*
100
39
15
29
Sales & services
Gifts & investments
Other
65,682
15,956
2627
13
3
<1
Legislative appropriations are allocated to the university on the basis of a funding formula that accounts for enrollment and the level and cost of the academic programs offered. Briefly, the formula incorporates an estimate of student FTEs in each course taught, which is calculated as the product of enrollment and course credits, divided by weights for clinical doctoral, master’s, and upper and lower-division undergraduate courses. These weights are selected such that doctoral courses yield the most FTEs and lower-division undergraduate courses the least, given equal enrollment and credits. Additional weights corresponding to target student-faculty ratios in clinical, high-, medium-, and low-cost disciplines are then applied to the sum of student FTEs to determine the number of faculty positions required for instruction. Staff positions and graduate assistantships are allocated in proportion to faculty numbers. Details of the formula are given on the university’s web site ( http://www.unr.edu/vpaf/pba/budget/fundformula.html
).
The effect of the funding formula is that institutions with larger enrollment in graduate courses or in high-cost disciplines, such as medicine and physical science, receive more resources relative to those that enroll primarily undergraduates or a proponderance of low-cost programs, such as business and social science.
Final Self Study, October 2010 Page 35
UNR School of Community Health Sciences
The funding formula governs the allocation of state funds to the institution as a whole, rather than to academic units and programs within the university. Internally, the university administration sets the non-grant portion of academic unit budgets in consultation with the deans and vice presidents. Tuition and fees received by the university are not returned directly to the units that generate them, but are part of the pool of funds available to the administration to meet the university’s operating expenses. Faculty salaries are the largest component of the state funds allocated to units. This sector of the budget is dictated by the number and rank of occupied faculty positions allocated to the unit in a given fiscal year. Tenure-line faculty positions in the
School of Community Health Sciences are fully state-supported, so state funding for these positions supports teaching, research, and service activities. Classified staff positions are handled similarly in that the number of state-supported positions is determined by the university administration in proportion to the number of faculty positions. Funds for staff positions are also allocated annually according to the job title and seniority of the incumbents. The university also allocates funds for general operations, including equipment, supplies, communications, travel, and student recruitment. Annual operating budgets are typically based on the budgets for previous years.
Funds for graduate assistantships are provided by the Graduate School. The number of full-time equivalent assistantships allocated to each academic program is determined by the Dean of the
Graduate School and is typically based on allocations in past years. However, the School of
Community Health Sciences has the option to split fulltime assistantships into full- and half-time positions.
Additional funds for instructional support and special projects are provided by the Office of the
Vice President for Health Sciences on request from the school. At the beginning of each academic year, the school submits an estimate of the number of credit hours to be taught by temporary and contract faculty and a budget based on this estimate and a standard contract rate set by the university. These requests are routinely granted. The school director may occasionally request other funds from the vice president. This process was used, for example, to equip a video conference facility that can be used for meetings and distance education.
1.6.b. A clearly formulated program budget statement, showing sources of all available funds and expenditures by major categories, since the last accreditation visit or for the last five years, which is longer. If the program does not have a separate budget, it must present an estimate of available funds and expenditures by major category and explain the basis of the estimate.
The MPH Program does not have a budget separate from the School of Community Health
Sciences. The school has an annual budget of approximately $2.2 million, including university funds, grants and indirect-cost recovery. University funds are the largest component, totaling approximately $1.6 million in the current fiscal year, including $1.3 million for faculty salaries,
$64,000 for staff salaries, $39,000 for general operations, $30,000 for instructional support and
$70,000 for graduate student stipends. Grant income in the last 5 years ranged from $262,000 in
2005-2006 to about 2.8 million in 2007-2008. Indirect cost receipts on faculty grants generate income averaging $5,000-7,000 per year. In addition, the university provided research startup funds to new faculty supporting the public health program. The school does not receive a direct appropriation from the state or a share of tuition and fees and does not have an endowment. No direct gifts were received in the past 5 years.
Final Self Study, October 2010 Page 36
UNR School of Community Health Sciences
From the preceding revenues, the school provided support to the program ranging from about
$700,000 in 2005-2006 to about $968,000 in 2008-2009, the last year with complete data. Note that data on revenues and expenses for the 2010 fiscal year were incomplete as of this writing, so these amounts may be underestimated. Program expenditures include: the portions of faculty and staff salaries and operating funds devoted to supporting the Program; graduate assistantships allocated to MPH students; instructional support funds for contract faculty teaching courses to
MPH students, and grants and contracts that contribute to the program. Estimates of these amounts in the last 5 years are shown in Table 1.6.b. Only revenues and expenditures related directly to the MPH program are shown in the table; the methods used to estimate these amounts are explained briefly in footnotes to the table.
Table 1.6.b. Sources of Funds and Expenditures by Major Category, Fiscal Years 2005 to
2009.
2005-2006 2006-2007 2007-2008 2008-2009 2009-2010
Source of Funds
Tuition & Fees 0
State Appropriation 0
University Funds
Grants/Contracts
Indirect Cost
Recovery
766,649
262,545
6,036
0
0
880,071
410,021
5,404
0
0
928,792
2,776,329
4,090
0
0
960,344
1,362,980
7,408
0
0
848,513
488,532
4,912
Endowment
Gifts
Other (explain)
Expenditures
Faculty Salaries &
Benefits 1
Staff Salaries &
Benefits
2
Operations
3
0
0
0
681,990
5,320
0
0
0
709,940
7,933
0
0
0
770,844
8,424
0
0
0
848,590
12,107
0
0
0
821,451
15,126
Travel
Student Support
University Tax
Equipment
Other: Contract
Faculty
Other: Faculty
Startups
10,039
881
81,084
0
0
0
0
7,941
257
94,665
0
0
0
70,000
9,700
1,223
163,538
0
0
0
66,200
20,377
0
89,332
0
0
0
87,000
11,936
0
106,850
0
0
2,445
0
Notes:
1.
Faculty salaries and benefits estimated from the proportion of total faculty FTE dedicated to the program (see Tables 1.6.e and 4.1.a).
2.
Staff salaries and benefits estimated from the proportion of staff effort dedicated to supporting the program.
3.
Operating costs for the program are estimated to be 25% of the total cost of operations for the
School of Community Health Sciences plus program-specific expenses (e.g., student recruitment, accreditation)
Final Self Study, October 2010 Page 37
UNR School of Community Health Sciences
The revenues and expenditures shown in Table 1.6.b were estimated as follows: the portion of faculty salaries and benefits supporting the Program was estimated using the data on faculty effort that we used to construct Tables 1.6.e and 4.1.a (below); staff effort in support of the
Program was estimated from position descriptions submitted to the university personnel system, and operating costs are proportional to the faculty and staff effort allocated to the program, plus program-specific expenditures, such as graduate student recruiting and accreditation-related fees.
The grant and contract funds and income from indirect cost recovery correspond to the grants and contracts listed in table 4.1.c. and are considered to support the Program. Note that grant expenditures for costs other than graduate research assistantships are not included in Table 1.6.b, so program revenues and expenses may not add. The budgeted and expended amounts shown for contract faculty supporting the program and for student support are the actual amounts, rather than estimates.
State support for the program has remained fairly constant over the past 5 years. Although a number of new faculty members have been hired, others have retired or left the university, so there has not been a net increase. The amounts budgeted for operations have been essentially flat for the past 5 years, but as a result of state budget shortfalls the state operating budget was retroactively reduced by 5% in fiscal 2009 and in fiscal 2010 mandatory furloughs were imposed for classified staff and untenured faculty. In contrast, funding from grants and contracts has increased substantially, from about $260,000 in 2005-06 to over $1.3 million in 2008-9 (the last year with complete data).
1.6.c. If the program is a collaborative one sponsored by two or more universities, the budget statement must make clear the financial contributions of each sponsoring university to the overall program budget. This should be accompanied by a description of how tuition and other income is shared, including indirect cost returns for research generated by public health program faculty who may have their primary appointment elsewhere.
Not applicable.
1.6.d. A concise statement or chart concerning the number (headcount) of core faculty employed by the program as of fall for each of the last three years.
Table 1.6.d. Headcount of Core Faculty (0.5 FTE or higher) by Specialty Area.
Epidemiology Social/Behavioral
Health
2007-2008 7 6
Total
13
2008-2009
2009-2010
Current Faculty
(October 2010)
8
8
6
5
6
6
13
14
12
1.6.e. A table showing faculty, students, and student/faculty ratios, organized by specialty area, for each of the last three years. These data must be presented in table format and include at least: a) headcount of primary faculty who support the teaching programs, b)
FTE conversion of faculty based on % time or % salary support devoted to the instructional programs, c) headcount of other faculty involved in the teaching programs
Final Self Study, October 2010 Page 38
UNR School of Community Health Sciences
(adjunct, part-time, secondary appointments, etc), d) FTE conversion of other faculty based on estimate of % time commitment, e) total headcount of core faculty plus other faculty, f) total FTE of core and other faculty, g) headcount of students in department or program area, h) FTE conversion of students, based on 9 or more credits per semester as full-time, i) student FTE divided by regular faculty FTE and j) student FTE divided by total faculty FTE, including other. All programs must provide data for a), b) and i) and may provide data for c), d) and j) depending on whether the program intends to include the contributions of other faculty in its FTE calculations.
Final Self Study, October 2010 Page 39
UNR School of Community Health Sciences
Table 1.6.e. Faculty, Students and Student/Faculty Ratios by Specialty Area
HC Core
Faculty
1
FTEF
Core
2
HC
Other
Faculty
1
FTEF
Other
2
Total
Faculty
HC
Total
FTEF
1) Academic Year 2007-2008
MPH – 7
Epidemiology
6.98
MPH --
Social/Behavioral
6
2
5.92 3
.73
0.79
9
9
7.71
6.71
Health
2) Academic Year 2008-2009
MPH –
Epidemiology
8 7.43 1
MPH --
Social/Behavioral
5 4.76
Health
3) Academic Year 2009-2010
3
.43
.75
9
8
7.86
5.51
8 7.63 0 0 8 7.63 MPH –
Epidemiology
4
MPH --
Social/Behavioral
Health
5
6 5.12 6 1.60 12 6.72
HC
Students
10
9
16
11
21
21
FTE
Students
9.56
6.83
12.72
16.06
14.05
9.17
3
SFR by
Core
FTEF
1.37
1.15
1.71
1.93
2.10
2.74
SFR by Total
FTEF
1.24
1.02
1.62
1.66
2.10
2.09
1.) Faculty are included in the head count where FTEF (calculated as explained in 2) > 0.5. 2.) Faculty FTE was estimated by dividing the number of hours each faculty member spent supporting the MPH program (advising MPH students, serving on MPH student committees, preparing for and teaching MPH courses, and research and service activities supporting the program) by the total hours in a standard work week (40 hours). 3.) Student FTE was calculated as full-time if enrolled in at least 18 credits during the academic year or 12 credits if employed as a graduate assistant. 4.) Includes 1 FTE dual MD/MPH student in epidemiology emphasis. 5.) Includes
2.83 FTE dual MD/MPH students in social/behavioral health emphasis.
Key:
HC = Head Count
Core = full-time faculty who support the teaching programs
FTE = Full-time-equivalent
FTEF = Full-time-equivalent faculty
Other = adjunct, part-time and secondary faculty
Total = Core + Other
SFR = Student/Faculty Ratio
Final Self Study, October 2010 Page 40
UNR School of Community Health Sciences
1.6.f. A concise statement or chart concerning the availability of other personnel
(administration and staff).
The school has two full-time administrative assistants who provide support for academic programs, in addition to other duties. Bonnie Coker is the assistant to the MPH program director. In that role, she records the transactions of the graduate program committee, processes applications to the MPH program, and assists in scheduling graduate courses. Ms. Coker is also
Assistant to the School of Community Health Sciences Director and has primary responsibility for maintaining the school’s financial accounts. Tara Burrows performs additional support functions for the program, including processing graduate assistant time sheets and payments for student stipends, maintaining files on students and alumni, and maintaining the program website.
Both administrative assistants and provide other support as needed, including general office functions. A part-time student employee assists with general office work. One other full-time staff member provides research and administrative support to the Center for Program Evaluation.
Although she does not work directly with MPH students, her work supports the program’s research mission.
Final Self Study, October 2010 Page 41
UNR School of Community Health Sciences
1.6.g. A concise statement or chart concerning amount of space available to the program by purpose (offices, classrooms, common space for student use, etc.), by program and location.
The Program has access to approximately 9700 sq. ft of administrative, faculty and research office space in the Lombardi Center on the main UNR campus. Details are shown in Table
1.6.g. and a brief description follows.
Table 1.6.g. Office, research and classroom space currently assigned to the SCHS
Description
Lombardi Recreation Center
Faculty office with window
Number Area (sq ft) Notes
14 1820 Average size 130 sq ft
Faculty office without window
Director’s office
Administrative offices
Grad student office
Conference room, 20 seats
Common/work room
Lecture room, 70 seats
Classroom, 40 seats
Seminar room, 15 seats
Research/LOA offices
Informatics Center
2
1
2
1
1
1
1
1
1
5
1
325
204
520
228
361
306
1596
720
385
750
280
9 workstations
Rm. 202
Rm. 205
Rm. 204
Rm. 214b
Average size 150 sq ft
Human subjects facility
Exercise physiology lab
Subotal
Applied Research Facility
Environmental health lab
Survey research lab
Mackay Science
Center for Program Evaluation
1
1
1
1
1260
866
9621
1000
1100
1000
ARF 315
ARF 205
Center for Ethics & Health Policy
Total
1000
12,171
Office and Administrative Space. Every full-time academic faculty member has a private office of approximately 130 sq. ft. with a telephone and networked personal computer with standard software. An administrative suite totaling 1100 sq. ft. includes offices for the school director, two administrative assistants and part-time student workers, and a staff work room. A 400 sq. ft. conference room with computer projection and video-conferencing capabilities is available for meetings and seminars. UNR IT provides timely administrative support for all technology issues including during emergencies.
Research Space. Five offices of about 150 sq. ft. each are available in the Lombardi Center for sponsored research projects. These offices typically provide work space for grant-supported graduate assistants. In addition to the preceding space in the Lombardi building, two affiliated centers, the Center for Program Evaluation, and the Nevada Center for Ethics and Health Policy,
Final Self Study, October 2010 Page 42
UNR School of Community Health Sciences occupy approximately 2000 sq. ft. in the Mackay Science building on the southern part of the main campus. Research laboratories are described below in section 1.6.h.
Classroom Space. Three classrooms are available to the program in the Lombardi building:
Room 204 (capacity 38 students), room 205 (capacity 70 students), and room 214b (capacity 15 students). Both of the larger rooms are “smart classrooms” equipped with networked computers connected to the internet, LCD projectors and document cameras. The school’s computer- and video-equipped conference room may also be utilized for teaching, including for distance learning. Classrooms in the Lombardi building are shared with the school’s undergraduate program and may be requested by other campus units when not in use. Recent growth in both the MPH program and undergraduate enrollment have increased the demand for instructional space, leading to some challenges in scheduling classes. Many graduate courses are offered in the evening to meet the needs of working professionals, and this also helps to ease the pressure on classroom space, and classes have also been scheduled in other university buildings. The school currently does not have its own instructional computer laboratory, but several such facilities are available on campus and are utilized for epidemiology and biostatistics courses.
Although the use of other campus space has made it possible to accommodate the need for more course sections, it reduces efficiency because of the increase in travel time for faculty and students.
Student Areas. State-supported graduate assistants have assigned carrels in a shared 250 sq. ft. office with 9 workstations. No other dedicated work space is available for graduate students who are not employed as research or teaching assistants. A common area (approximately 850 sq. ft.) with tables and chairs is provided on the second floor of the building, and students have very convenient access to the new Joe Crowley Student Union, which offers study space, restaurants, a bookstore and a convenience store, and to the IGT-Matheson Knowledge Center which has extensive areas for study and research.
The Program’s current space in the Lombardi Center is largely adequate for current needs, but it is being utilized to full capacity, with very limited opportunity for future expansion. More graduate student work space and a computer teaching lab are needed and access to additional classroom space is desirable. The university’s plans currently call for the School of Community
Health Sciences to move to new, large space after the 2010-2011 academic year, when several new buildings are scheduled to open.
1.6.h. A concise statement or floor plan concerning laboratory space, including kind, quantity and special features or special equipment.
Laboratory space is available to the program in the Lombardi Center and in the adjacent Applied
Research Facility (ARF). A human subjects facility used for clinical research is located on the ground floor of the Lombardi building. This laboratory is approximately 1200 sq. ft., including a private room for interviewing or examinations, and is equipped with clinical manipulation tables, a GE Dual Energy X-Ray Absorptiometer for measuring body composition, a Precor treadmill, and a Cosmed K4b2 portable metabolic system. An exercise physiology laboratory, also located in Lombardi, is used primarily for undergraduate teaching. A 320 sq. ft. lab the 2 nd
floor of
Lombardi is houses facilities for statistical data analysis used by the Nevada Center for Health
Statistics and Informatics. The lab has 6 computer work stations and a 16 TB memory size data analysis server.
Final Self Study, October 2010 Page 43
UNR School of Community Health Sciences
In the ARF, the School of Community Health Sciences controls a 1000 sq. ft. research laboratory that support activities relating to translational medicine, environmental and cellular physiology, histopathology, molecular biology, environmental toxicology, cell / tissue culture, and algal aquaculture. Specialized equipment is available for use by researchers in the school, the Division of Health Sciences, and other researchers in the UNR community, on a collaborative basis.
Research equipment maintained in the ARF ab includes: Microscopy - Zeiss Axioplan 2 imaging upright fluorescence microscope with Axiocam HRc high-speed camera and Axiovision 4.8 image processing software; Zeiss Axiovert 25 inverted fluorescence microscope with Axiocam
MRc high-speed camera and Axiovision 4.8 image processing software; Nikon SMZ-2T dissecting scope with Sony color camera; Custom-built three-channel confocal microscope based on Zeiss Axioplan 2 imaging upright microscope, with laser excitation lines at 488, 532, and
635nm. Electrophysiology - Patch clamp workstation based on Zeiss Axiovert 40CFL stand, with Siskiyou 4-axis micromanipulator, Axon Axopatch 200B and 1D amplifiers, and Axon
1200 / Clampex 8 A/D converter and data processing software; Vascular contractility workstation with (4) Radnoti tissue baths, WPI TBM-4 transbridge, and custom National
Instruments Labview data interface; Tissue clamp / stimulation workstation with Olympus dissecting scope, Grass S48 stimulators, Axon Geneclamp 500 amplifier, and Axon 1200 /
Clampex 8 A/D converter and data processing software. Molecular Biology / Cell Culture -
Cepheid SmartCycler four-color real-time quantitative PCR system; Applied Biosystems 7500 four-color real-time quantitative PCR system, Alpha Innotech gel imaging workstation; Esco
Class IIIb biosafety hood, liquid nitrogen storage, stacking Heraeus HeraCell incubators, -80C freezers, Zeiss Invertoskop inverted cell culture inspection microscope, numerous agarose,
PAGE, and Western blot electrophoresis setups. Histopathology - Shandon 620 cryostat;
Shandon Hypercenter XP tissue processing station. Aquaculture equipment - (2) Braun Biotech /
Sartorius Biostat B fermenters / custom photobioreactors supporting 2L and 5L culture vessels;
(1) Braun Biotech / Sartorius Biostat i fermenter / custom photobioreactor, supporting 2 x 10L culture vessels; B. Braun Biostat M 1L fermenter; B. Braun Biostat E 15L stainless steel fermenter system. Analytical equipment - Tecan Ultra384 fluorescence / luminescence / absorbance plate reader; Shimadzu UV-1601 UV-Vis Absorbance spectrophotometer; Cahn microbalance, various analytical balances, pH meters, and other miscellaneous equipment.
Also in ARF, is laboratory space for survey research and analysis of statistical data that is occupied by the Nevada Center for Health Statistics and Informatics. This includes an 800 sq. ft. data collection and survey lab in the Applied Research Facility, which has work areas, meeting space and 5 workstations equipped with PCs and software for Computer Assisted Telephone
Interview functions.
1.6.i. A concise statement concerning the amount, location and types of computer facilities and resources for students, faculty, administration and staff.
All full-time administrators, faculty and staff have their own dedicated, networked computer workstations. Two high-speed networked printers are available in the Lombardi Building and most faculty members also have local printers. All faculty and staff computers are connected to the Internet and are equipped with standard software for communication, word processing and data analysis. The university has site licenses for numerous software packages for such specialized tasks as statistical analysis, as well for general office use, and these are available for faculty, staff and students at no or reduced cost. The university also provides free email service
Final Self Study, October 2010 Page 44
UNR School of Community Health Sciences to employees and students. University-owned computers and software are maintained by the
University’s Information Technology staff at no cost to the program.
Computing facilities are available to students in several locations on campus. Graduate research and teaching assistants have access to a student office with 8 networked workstations on the second floor of the Lombardi Building. Graduate assistants working on research projects usually have access to additional computers in faculty research offices and laboratories.
In addition to the school’s on-site facilities, a fully equipped, state-of-the-art computer laboratory is available to students in the adjacent IGT-Matheson Knowledge Center.
There are more than 66 public and departmental computer labs across campus. All computers on the UNR domain require a login and can connect to the campus network by cable or wireless.
Computers vary from basic desktop workstations and checkout laptops to high-end systems for research and special projects. All computers supported by the campus IT staff are purchased through approved vendors, run the latest operating systems and security software, and receive regular maintenance at the start of each semester. Faculty, staff and administration office computers are available through the department or campus replacement program.
All students, faculty, staff, administration and guests have access to standard IT user support through a centralized Help Desk in the Mathewson-IGT Knowledge Center. The Help Desk is available by phone, email and a walk-up counter. Service requests that cannot be resolved immediately are recorded and maintained in an electronic work order system. Information on IT supported systems and user support, plus self-help documentation is available on the UNR IT website at http://www.it.unr.edu
1.6.j. A concise statement of library/information resources available for program use, including description of library capabilities in providing digital (electronic) content, access mechanisms and guidance in using them, and document delivery services.
The scope of the Mathewson-IGT Knowledge Center reaches far beyond its 295,000-square-foot size. As the pace of innovation and intellectual growth continues to flourish at the university, the
Knowledge Center is uniquely positioned as one of the most technologically advanced university libraries in the country, providing the discovery, acquisition, and access to diverse forms of knowledge that the university’s students and faculty need. Building highlights include: automated book retrieval system; reading rooms and quiet study-areas; computing laboratories and large format printing; wireless network and computer access throughout; smart classrooms and conference rooms.
Resources. The collection contains more than 1 million volumes of books and journals, 23,000plus e-journals and more than 50,000 e-books. Plus, hundreds of general and specialized research databases available online. More specifically, the collection boasts more than 600 electronic journal subscriptions relating to public health and many, many more general health sciences titles. The University of Nevada Savitt Medical Library (located just north of the school) has designated funds with which to purchase new titles in public health.
Guidance.
Research and Computing Help Desk: Recognizing the synergy between information and technology, the Knowledge Center has consolidated library research and computing help
Final Self Study, October 2010 Page 45
UNR School of Community Health Sciences into a single service point. The pooled expertise of library and information technology professionals aids library users in eliminating obstacles to access, empowering them with the tools and skills they will require to navigate the complex web of knowledge to which the
Knowledge Center hopes to function as a gateway. Library staff also provide assistance via phone, email and chat services to give students, faculty and staff a broad range of service options.
Library Services Desk. Continuing the theme of one-stop shopping, a single counter pulls together the related, yet often separated, roles of circulation, electronic reserves, and document delivery services.
@One Desk. The @One desk is staffed by both library and technical staff available to field any question that a computer lab user might have.
Other Instructional Assistance. Subject-specialist librarians are available upon request to provide one-on-one and in-class instruction in their areas of expertise.
Delivery Services: LINK+. LINK+ is a combined catalog of over 5 million unique books from participating libraries throughout California and Nevada. Users from member libraries electronically request an item not available in their own library and it is delivered to them for check out. Items usually arrive within 4 days and there is no charge to UNR faculty, students and staff to request or borrow LINK+ materials.
Document Delivery Services.
When library materials are not available in the University of
Nevada, Reno Libraries, library users may request those items through Document Delivery
Services. This service supplies books not available through LINK+ and articles not owned by the university libraries. This service is provided free of charge to UNR faculty, students and staff.
Access mechanisms.
Currently enrolled UNR students, faculty or staff members are eligible for off-campus access to licensed resources upon providing necessary identification. Wireless network and computer access is available throughout the Mathewson-IGT Knowledge Center.
1.6.k. A concise statement describing community resources available for instruction, research and service, indicating those where formal agreements exist.
The school has an extensive network of relationships with organizations that provide opportunities for instruction, research and service. The school has a formal contract, which is renewed annually, with the Washoe County District Health Department to facilitate student field placements and other collaborations. Agreements with other organizations are typically made on an ad hoc basis for the duration of specific projects.
The school is committed to collaborating with community organizations to fulfill its mission of teaching, research and service. The school seeks external partnerships at local, state, national, and global levels. Community ‐ based collaboration with the school takes a variety of forms including invited lecturers, opportunities for summer study abroad programs, community ‐ engaged research, service ‐ learning opportunities, community advisory board, and student field placement.
Final Self Study, October 2010 Page 46
UNR School of Community Health Sciences
The Washoe County District Health Department is located less than a mile from the university and the Nevada State Health Division is located 30 miles away in Carson City, NV. There are also a number of county health districts in the Eastern Sierra which is just across the state boarder in California. The Health Officer from Nevada County, California is a member of the school’s Advisory Board.
The students and faculty are involved with many community agencies in the Reno/Sparks area.
There are also opportunities for students to be exposed to rural settings in Nevada. For example, an MPH student did a field studies placement through the Quentin Burdick Rural
Interdisciplinary Training Program in which she worked with multi-disciplinary teams in Fallon,
Nevada. Also, students in the toxic communities class have traveled to rural communities in which mining sites are located to interview residents.
Public health personnel from the Washoe County District Health Department have served as guest lecturers in almost every MPH course. Other public health guest speakers include professionals from the Nevada State Health Division, area hospitals, the State Division of Aging
Services, Planned Parenthood, and MPH alumni. Guest lecturers are also frequently used in undergraduate courses to expose newer students to public health practice. Public health professionals, especially from the Washoe County District Health Department, have served as course instructors and are members of the school’s affiliate and adjunct faculty. Community affiliate faculty members have served on faculty search committees. Grants and contracts for research and service with the community are described in section 3.2.b.
1.6.l. A concise statement of the amount and source of “in-kind” academic contributions available for instruction, research and service, indicating where formal agreements exist.
The school faculty have sufficient time in their workload to fulfill the program’s mission, which includes teaching courses, mentoring students, and conducting research. Therefore, “in-kind” academic contributions have not been extensively needed for the school. All internship supervisors provide preceptor support to students without cost although many sites provide a student stipend and formal agreements for this support exist. Graduate assistant positions have been available to MPH students at locations which include UNR’s Gerontology Academic
Program, Sanford Center for Aging, the Center for the Application of Substance Abuse
Technologies, Department of Nutrition, School of Nursing, School of Medicine, and Center for
Ethics and Health Policy. Faculty throughout the university, but especially adjunct and affiliate faculty, serve on MPH students' culminating committees. The university also has teaching and research grants available.
1.6.m. Identification of outcome measures by which the program may judge the adequacy of its resources, along with data regarding the program’s performance against those measures for each of the last three years. At a minimum, the program must provide data on institutional expenditures per full-time-equivalent student, research dollars per fulltime-equivalent faculty, and extramural funding (service or training) as a percent of the total budget.
Final Self Study, October 2010 Page 47
UNR School of Community Health Sciences
Table 1.6.m. Selected Outcome Measures for Program Resources.
Outcome Measure 2007-2008 2008-2009
$62,228.74 $48,305.44 Expenditures per FTE
Student
Research Dollars per
FTE Faculty*
$173,520.56 $97,355.71
2009-2010
$36,462.44
$30,533.35
25% Extramural Funding
(service/training) per
Total Budget**
N/A 15%
*Only includes FTE for faculty who have research responsibilities. In addition, includes only those grants which contribute to program budget (e.g., direct and indirect costs received by school). Does not include grants in which faculty are project personnel or co-investigators and funding is housed in another department. Grants in which faculty are project personnel or coinvestigators are included in the school’s objectives data which explains why those figures may be higher.
**These percentages are calculated using grants awarded in the study years that have a service component divided by the total budget for that year.
1.6.n. Assessment of the extent to which this criterion is met.
This criterion is met. The Program has sufficient resources to support its activities.
Strengths
Faculty have been awarded increasing grant support in the past 5 years.
The program has secured university funds to support graduate assistants.
The program has secured university funds for new faculty startups.
The program enjoys more than the minimum faculty FTE in each specialty area.
The university has opened state of the art campus library facilities.
Suggested Improvements
The impact of state budget cuts may strain state-funded support.
The physical space at present is limited.
The SCHS should consider options to develop an alumni giving program and pursing endowments.
Final Self Study, October 2010 Page 48
UNR School of Community Health Sciences
2.0 Instructional Programs
2.1 Master of Public Health Degree. The program shall offer instructional programs reflecting its stated mission and goals, leading to the Master of Public Health (MPH) or equivalent professional masters degree. The program may offer a generalist MPH degree or and MPH with areas of specialization. The program, depending upon how it defines the unit of accreditation, may offer other degrees, professional and academic, if consistent with its mission and resources .
2.1.a. An instructional matrix (see Table 2.1.a.) presenting all of the program’s degree programs and areas of specialization, including undergraduate, masters and doctoral degrees, as appropriate. If multiple areas of specialization are available, these should be included. The matrix should distinguish between professional and academic degrees and identify any programs that are offered in distance learning or other formats. Non-degree programs, such as certificates or continuing education, should not be included in matrix.
Table 2.1.a. Instructional Matrix – Degree/Specialization.
Master of Public Health - Social/Behavioral Health
Master of Public Health - Epidemiology
Academic Professional
X
X
Joint Degrees
MD/MPH X
In addition to the degrees and specializations in Table 2.1.a., there are six students in other emphases which are not being submitted for accreditation review at this time. Due to a loss of faculty, we are no longer accepting students in health ethics, policy, and administration (3 students currently enrolled who were accepted previously) and environmental/occupational health (1 student enrolled previously accepted). There are 2 students previously accepted to the joint Master of Science in Nursing/MPH degree program. However, we are not accepting students into this degree at this time because the curriculum is being updated (see Section 2.10
Joint Degrees).
In collaboration with the University of Nevada Las Vegas (UNLV) School of Community Health
Sciences, we offer a joint PhD in environmental and occupational health. There are 2 students enrolled in this program. This program is currently not taking students and is not being submitted for accreditation review.
2.1.b. The bulletin or other official publication, which describes all curricula offered by the program. If the university does not publish a bulletin or other official publications, the program must provide for each degree and are of specialization identified in the instructional matrix a printed description of the curriculum, including a list of required courses and their course description .
Epidemiology Description. Epidemiology, the fundamental science underlying public health, is the study of the distribution and determinants of health and diseases, morbidity, injuries, disability, and mortality in populations. The epidemiology concentration is designed for students
Final Self Study, October 2010 Page 49
UNR School of Community Health Sciences seeking to acquire skills necessary for careers in descriptive and analytic epidemiology. Students enrolled in this area of emphasis will acquire the methodologic skills necessary to study a wide range of public health issues including: infectious disease, chronic disease, health care delivery, social and behavioral health, environmental health, and occupational health. Concentration courses emphasize basic and advanced epidemiologic principles and their application to current problems in public health and related disciplines. Students in the epidemiology concentration are expected to use appropriate methods to plan, implement, and conduct epidemiologic research.
Students are also expected to critically evaluate research methodology to assess validity and potential sources of bias. Students receive applied analysis training using common statistical packages and opportunities to analyze, interpret, and disseminate the results of epidemiologic investigations.
http://www.unr.edu/public-health/epi.html
Social and Behavioral Health Description.
Social and behavioral health examines the psychological, behavioral, social, cultural, and institutional factors that affect individual and population health. The social and behavioral health MPH concentration is designed for students interested in health promotion, health education, and the prevention and reduction of health disparities over the life course. Social/behavioral health researchers and practitioners solve public health problems through public health policy, services, and interventions at the individual, family, community, and societal level. In their concentration courses, students are trained to apply health promotion and behavior change theories to design, implement, and evaluate public health policies and programs.
http://www.unr.edu/public-health/soc_behav_health.html
MD/MPH Degree. http://www.cis.unr.edu/ecatalog/default.aspx?article_list_id=22379
Course Descriptions . http://www.ss.unr.edu/records/catalog//?prefix=CHS
2.1.c. Assessment of the extent to which this criterion is met.
This criterion is met.
Strengths
The MD/MPH provides a model for future collaboration with other departments (e.g., business). For example, minor overlap between the MPH program and the medical school curriculum was identified. This curriculum coordination was used as a guide for the current revisions to the dual nursing/MPH degree. We also have learned how to better serve students with different schedules. At the university level, course and curricular committees now have a model for understanding how future coordinated degree offerings between public health and other departments can be successful.
Suggested Improvements
We plan to review course and curricular descriptions on UNR website regularly for accuracy and completeness. The last review occurred in the summer of 2010 and the web’s catalog description of the MPH program was revised.
Based on discussion with our Advisory Board, the need to create more online courses for professionals working in rural Nevada is pressing and we have agreed to put three of the core courses online in the fall of 2011.
Final Self Study, October 2010 Page 50
UNR School of Community Health Sciences
2.2 Program Length .
An MPH degree program or equivalent professional master’s degree must be at least 42 semester credit units in length.
The MPH program is 43 credits for both the epidemiology and social/behavioral health emphases. The program length was approved by the appropriate UNR curricular committees in spring 2006 for students entering the program fall 2006. One student was admitted in the spring
2006 semester when the revisions were occurring but she completed the 43-credit epidemiology emphasis. Prior to that time, the MPH program was 39 credits.
2.2.a. Definition of a credit with regard to classroom/contact hours.
According to official policy from UNR’s Office of the Provost and as explained in the UNR catalog: “Described in semester credit hours, a credit is defined as three hours of work per week for one semester. Usually this work is made up of one period in class plus two hours of preparation for lecture-seminar classes, or three hours of laboratory classes.” This definition is available on the UNR catalog website at: http://www.cis.unr.edu/ecatalog/Default.aspx?article_list_id=16188 . Therefore, a course with 3 hours of lecture per week during a 15-16 week semester is equated with 3 student credit hours.
2.2.b. Information about the minimum degree requirements for all professional degree curricula shown in the instructional matrix. If the program or university uses a unit of academic credit or an academic term different than the standard semester or quarter, this should be explained and an equivalency presented in a table or narrative.
Tables 2.2.b.1. and 2.2.b.2. summarize the minimum requirements for the MPH professional degree, with emphases in epidemiology and social/behavioral health. The degree requires 13 credits of core courses and 30 credits each in the two emphases. Hence, the MPH degree
Program conforms to accepted standards regarding program length and objectives of the credentials. Students in the dual MD/MPH program must choose to complete either the epidemiology or social/behavioral health emphasis.
Final Self Study, October 2010 Page 51
UNR School of Community Health Sciences
Table 2.2.b.1 Master of Public Health Program Curriculum, Epidemiology Option (43 credit hours)
MPH Core
(21 hours)
CHS 700R – Research Methods for Public Health (1)
CHS 701 – Social and Behavioral Dimensions of Health (3)
CHS 712 – Epidemiology in Public Health (3)
Epidemiology
Required Courses
(12 hours)
CHS 725 – Health and the Environment (3)
CHS 755 – Health Policy and Administration (3)
CHS 780 – Biostatistics in Public Health (3)
CHS 703R – Applied Health Data Analysis (3)
CHS 708 – Epidemiology II (4)
CHS 709R – Epidemiologic Research Design and Planning (2)
CHS 753 – Health Informatics (3)
Practicum (6 hours) CHS 694 – Field Studies in Public Health (6)
Capstone (3 hours) CHS 695R – MPH Capstone (3)
Electives (students choose 6 hours from the following)
CHS 661 – Global Health (3)
CHS 706 – Social Epidemiology (3)
CHS 707 – HIV/AIDS Epidemiology (3)
CHS 722 – Epidemiology of Chronic Diseases (3)
CHS 723 – Epidemiology of Infectious Diseases (3)
CHS 724 – Environmental Epidemiology (3)
CHS 735 – Exposure Assessment and Control (3)
CHS 739 – Cancer Epidemiology (3)
CHS 740 – Epidemiology of Cardiovascular Disease (3)
CHS 742 – Epidemiology of Tropical Diseases (3)
CHS 748 – Epidemiologic Surveillance (3)
CHS 749 – Outbreak Investigation (3)
CHS 781 – Environmental and Occupational Risk Assessment (3)
CHS 782 – Analysis of Categorical Data (3)
CHS 783R – Regression and Multivariant Analysis in Health Sciences (3)
CHS 784 – Conduct and Analysis of Clinical Trials (3)
EAB 725 – Infectious Disease Epidemiology (online UNLV) (3)
EAB 745 – Epidemiological Surveillance (online UNLV) (3)
Final Self Study, October 2010 Page 52
UNR School of Community Health Sciences
Table 2.2.b.2. Master of Public Health Program Curriculum, Social and Behavioral Health
Option (43 credit hours)
MPH Core
(21 hours)
CHS 700R – Research Methods for Public Health (1)
CHS 701 – Social and Behavioral Dimensions of Health (3)
CHS 712 – Epidemiology in Public Health (3)
Social and
Behavioral Health
Required Courses
CHS 725 – Health and the Environment (3)
CHS 755 – Health Policy and Administration (3)
CHS 780 – Biostatistics in Public Health (3)
CHS 705 – Theoretical Foundations of Health Promotion (3)
CHS 720 – Program Planning and Grant Writing (3)
CHS 721 – Program Evaluation in Public Health (3)
(12 hours) CHS 746 – Cultural Diversity in Public Health (3)
Practicum (6 hours) CHS 694 – Field Studies in Public Health (6)
Capstone (3 hours) CHS 695R – MPH Capstone (3)
Electives (students choose 6 hours from the following)
CHS 605 – Spirituality and Health (3)
CHS 626 – Medical Anthropology (3)
CHS 627 – Toxic Communities and Public Health (3)
CHS 639 – Cross-Cultural Perspectives and Health (3)
CHS 648 – Research Ethics in Public Health (3)
CHS 660 – Disability Issues in Public Health (3)
CHS 661 – Global Health (3)
CHS 676 – AIDS: Psychosocial and Healthcare Concerns (3)
CHS 706 – Social Epidemiology (3)
CHS 707 – HIV/AIDS Epidemiology (3)
CHS 710 – Health Behavior Change (3)
CHS 711 – Advocacy in Health Promotion (3)
CHS 738 – Public Health and Aging (3)
CHS 791 – Seminar: Health Communication (3)
ECON 620 – Economics of Health Care and Health Policy (3)
EDSP 632 – Serving Individuals with Disabilities and their Families (3)
EDUC 753 – Advanced Qualitative Methods (3)
Human Development & Family Studies (HDFS) 637 – Death and Dying:
Family and Lifespan Perspectives (3)
HDFS 638 – Children and Families in a Multiethnic Society (3)
HDFS 658 – Families and Public Policy (3)
HIST 690B – Social History of Medicine in Modern Era (3)
NURS 630 – Aging and Health (3)
NUTR 720 – Public Health Nutrition (3)
NUTR 725 – Nutrition and Health (3)
PSY 641 – Abnormal Psychology (3)
PSY 642 – Psychology of Aging (3)
PSY 644 – Psychology of Exceptional Children (3)
PSY 748 – Community Psychology (3)
SOC 657 – Society and Health (3)
SOC 737 – Survey Research Methods (3)
SW 741 – Advanced Research – Data Collection and Analysis (3)
Final Self Study, October 2010 Page 53
UNR School of Community Health Sciences
2.2c. Information about the number of MPH degrees awarded for less than 42 semester credit units, or equivalent, over each of the last three years. A summary of the reasons should be included.
No student in either the epidemiology or social/behavioral health emphasis has graduated with less than 43 credits. Twelve students completing the discontinued generalist emphasis graduated with 39 credits (Table 2.2.c.). Two students completed the dual nursing MSN/MPH which only required 18 public health credits at that time. It is no longer an option to complete the MPH degree with less than 43 credits. The dual MSN/MPH is currently being revised and no students are being accepted into that emphasis until the curriculum has been updated.
Table 2.2.c. Students Graduating with fewer than 43 credits
Generalist Program MSN/MPH
2007 – 2008 8 1
2008 – 2009
2009 – 2010
4
0
1
0
TOTAL 12 2
There are two students in the dual emphasis with nursing accepted under the previous curricula of fewer than 43 credits remaining in the program who plan to graduate in May 2011. There is one remaining generalist student who is enrolled fall 2010 in 6 credits (PUBH 720 program planning and PUBH 705 theory) to replace older credits earned outside the 6-year timeline required by the university to complete a master’s degree. She will graduate this fall (December
2010) with more than 43 credits.
2.2.d. Assessment of the extent to which this criterion is met.
This criterion is met.
Strengths
The minimum requirements for the MPH degree are set forth and well publicized in university and program materials.
The program meets the accepted standards for program length. No students in epidemiology or social/behavioral health have graduated with less than 43 credits and all active degree programs meet the criteria.
Students are exposed to a solid core of public health coursework and have a variety of reviewed and approved options for electives across campus.
Suggested Improvements
Based on our analysis, the Graduate Program Director recommended we develop additional program materials to assist in recruiting students and increase information sources about the program for existing students. To help the school improve in this area,
UNR’s Graduate School has given $2,000 to the Director of Internal/External Relations
Final Self Study, October 2010 Page 54
UNR School of Community Health Sciences specifically for recruitment. A graduate assistant is now helping recruitment, especially among minority students and additional program materials have been produced.
The school’s curriculum has been reviewed and approved (pending successful CEPH accreditation) for entry into the Western Interstate Commission for Higher Education
(WICHE), Western Region Graduate Program (WRGP). This program makes highquality, distinctive graduate programs and healthcare-related programs available to students of the West at the resident tuition rate and WRGP helps place students in graduate programs, all designed around the educational, social, and economic needs of the West. To be included in WRGP, programs must meet the criteria of distinctiveness (if they are not related to healthcare) and quality.
Final Self Study, October 2010 Page 55
UNR School of Community Health Sciences
2.3 Public Health Core Knowledge. All professional degree students must demonstrate an understanding of the public health core knowledge.
MPH students develop a broad understanding of public health through a series of required MPH core courses. Tables 2.3.a.1 and 2 contain the course numbers and titles for the core courses.
These courses correspond to the five specialty areas of knowledge basic to public health
(biostatistics, environmental/occupational health, epidemiology, health policy/administration and social/behavioral health). In addition, all students are required to complete a 1-credit research methods course. An overall grade point average of 3.0 is required for completion of the degree.
To ensure competency in core public health knowledge, a grade of Bor higher is required for credit to be awarded in the core courses.
The academic departments and the MPH faculty developed areas of competency which all MPH students must master before graduating from the program. The competencies were reviewed and approved by all faculty and are available on the school website. The faculty instructing in the five core courses prepare and revise learning objectives for their specific core courses which link to the areas of competency for the MPH program (as do all faculty teaching required courses in both emphases). It is especially during the culminating experience (see Section 2.5) when students must demonstrate attainment of the competencies.
2.3.a. Identification of the means by which the program assures that all professional degree students have a broad understanding of the areas of knowledge basic to public health. If this means is common across the program, it need be described only once. If it varies by degree or specialty area, sufficient information must be provided to assess compliance by each.
Table 2.3.a.1. Course Progression for MPH in Epidemiology (Two Years: 43 Units).
Summer #1 (second term):
CHS 700R: Research Methods (1)
Credits
1
Year 1: fall semester
CHS 712: Epidemiology I (3)
CHS 780: Biostatistics (3)
CHS 701: Social/Behavioral (3)
Credits
9
Credits
3
Year 1: spring semester
CHS 709R: Epi Research & Planning
(2)
CHS 703R: Applied Analysis (3)
CHS 708: Epidemiology II (4)
CHS 755: Policy & Administration (3)
Credits
12
Summer #2:
CHS 694: Field Studies (3)
Year 2: fall semester
CHS 753: Health Informatics (3)
Epidemiology Elective (3)
CHS 694: Field Studies (3)
Credits
9
Year 2: spring semester
Epidemiology Elective (3)
Culminating Experience / Capstone (3)
CHS 725: Environmental Health (3)
Credits
9
Final Self Study, October 2010 Page 56
UNR School of Community Health Sciences
Table 2.3.a.2. Course Progression for the MPH in Social/Behavioral Health (Two Years: 43
Units).
Summer #1 (second term):
CHS 700R: Research Methods (1)
Credits
1
Year 1: fall semester
CHS 712: Epidemiology I (3)
CHS 701: Social/Behavioral (3)
CHS 705: Theory (3)
CHS 720: Program Planning (3)
Summer #2:
CHS 694: Field Studies (3)
Credits
12
Credits
3
Year 1: spring semester
CHS 721: Evaluation (3)
CHS 755: Policy & Administration (3)
CHS 746: Culture & Diversity in
Public Health (3)
Credits
9
Year 2: fall semester
CHS 780: Biostatistics (3)
Elective (3)
CHS 694: Field Studies (3)
Credits
9
Year 2: spring semester
CHS 725: Environmental Health (3)
Elective (3)
Culminating Experience / Capstone
(3)
Credits
9
CHS 700R: Research methods is an online class and students are not required to be on campus until the fall semester. Students are given information about the online class when accepted into the program and reminded prior to the start of courses.
Section 2.6 summarizes the competencies for all MPH students. Mechanisms for assessing the competency of students completing the program are described in Section 2.7.
2.3.b. Assessment of the extent to which this criterion is met.
This criterion is met.
Strengths
The school provides curricular methods to assure students are able to demonstrate understanding of public health core knowledge. The competencies associated with core knowledge are mapped to specific classroom assignments and activities.
Students are successfully moving through the core classes. Meetings with all core instructors take place twice each semester to review student progress and identify early any student learning issues.
Suggested Improvements
The competency
‐ based education has been firmly developed in the last year and this curricular overview must be carefully monitored for impact and effectiveness. The twice semester meetings of core teaching faculty to discuss student concerns and progress is one of our guides to evaluate the effectiveness of the core curriculum. These twice semester meetings also help us to monitor our curriculum and make recommendations to the graduate committee to increase the effectiveness of the core curriculum.
Final Self Study, October 2010 Page 57
UNR School of Community Health Sciences
2.4 Practical Skills. All professional degree students must develop skills in basic public health concepts and demonstrate the application of these concepts through a practice experience that is relevant to the students’ areas of specialization.
2.4.a. Description of the program’s policies and procedures regarding practice placements, including selection of sites, methods for approving preceptors, approaches for faculty supervision of students, means of evaluating practice placement sites, preceptor qualifications, and criteria for waiving the experience.
Practical public health skill development is an integral part of the MPH program, regardless of program concentration, requiring 270 hours (6 credit hours) of professional work experience in a public health agency (clerical- level work is not accepted). While students are encouraged to take these six credits in two consecutive semesters (3 credits each), the program is flexible regarding the time frame in which students complete the internship, provided that 45 hours of internship coincide with each credit.
Internship participation is required for all MPH students; no students receive waivers for the course. Students are responsible for locating and arranging their own internship experience, with support from their faculty advisor and the internship coordinator. Faculty advisors and the internship coordinator maintain ongoing communication with former site preceptors to facilitate new student placements and partnerships in state and local health departments and community agencies, and continuously work to foster new community relationships with potential preceptors in order to develop further student opportunities.
Working with their faculty advisor and the internship coordinator, students begin planning for the internship at least three months before the desired start date by examining interests, program concentration, competencies, and goals for the internship. Students locate sites and preceptors based on all of these factors. Once a site and preceptor are arranged, the student completes the
Memorandum of Understanding (MOU), a student learning contract outlining student goals, competencies to be addressed, and scope of work for the internship (see Appendix C for MOU; course overview provided in onsite resource file). Upon student completion of this document, it is reviewed and signed by the preceptor, faculty advisor, and internship coordinator to ensure common understanding among all parties in moving forward. Only then can the student begin work on the internship.
Internship emphasis is placed on developing an experience that will provide the student with opportunities to: enhance skills learned during coursework, develop new skills and experiences in which the student will be working in a professional capacity, address competencies, and evaluate the site and overall experience. Students are required to focus on six Association of
Schools of Public Health (ASPH) competencies during the internship coursework, three of which are pre-defined (one leadership [H-2] and two professionalism [J-5 and J-10]), and three of the student’s choice, to be determined by areas of special interest or an identified need to enhance specific skills, and which apply to the individual internship experience. In addition to the 270hour work requirement, students must complete two reports during their internship work. The mid-term and final reports require students to research the organization for which they are
Final Self Study, October 2010 Page 58
UNR School of Community Health Sciences working, describe their own role in addressing the agency’s mission and vision, and reflect on their progress in working toward the goals and competencies identified in the MOU.
Preceptors are approved by the faculty advisor and the internship coordinator, and qualifications are based on position in the organization and extent of public health background, including number of years in practice as well as educational degrees earned. In addition to overseeing student on-site work, preceptors provide mid-term (at 100 hours of internship completed) and final (at 250 hours) evaluations of student performance, strengths, areas for improvement, and readiness to enter the public health workforce (Preceptor mid-term and final student evaluations will be provided in onsite resource file).
The internship coordinator facilitates the internship course (CHS 694) and is responsible for overseeing students during their internships, including maintaining communication with the student and preceptor throughout the internship, establishing procedures, monitoring progress, assessing quality, and arranging for student and site evaluations. Faculty advisors serve in a supportive role for students throughout the internship process, assisting the student in the development of internship goals and competencies, locating a suitable placement site, and monitoring student progress.
Placement sites and preceptors are evaluated by the student on such topics as: relevance of the experience to student goals and competencies, professional work environment, engagement of preceptor and other agency staff, and strengths and weaknesses of the site for future internships
(Student Site Assessment will be provided in onsite resource file). The internship coordinator and faculty advisor also contribute evaluations from their perspectives of the effectiveness of each site and preceptor for the internship, and recommendation of the site for future placements.
2.4.b. Identification of agencies and preceptors used for practice experiences for students, by specialty area, for the last 3 academic years.
Table 2.4.b. MPH Internship Placements for Academic Years 2007-2010
Internship Site Preceptor
Epidemiology Emphasis
Bureau of Family Health Services, Nevada
State Health Division
Bureau of Community Health Services,
Nevada State Health Division
Gastroenterology Consultants/Nevada Colon
Cancer Coalition
Bureau of Family Health Services Nevada
State Health Division
National Institute of Environmental Health
Sciences
Washoe County Department of Juvenile
Services
Judy Wright Bureau Chief
Debra McBride, MBA Bureau Chief
John Gray, MD, FACP
Debra Wagler, MA
Jane Hoppin, ScD
Joseph Haas, MD
Final Self Study, October 2010 Page 59
UNR School of Community Health Sciences
Internship Site Preceptor
Epidemiology Emphasis
Clark County Department of Juvenile
Services
Renown Regional Medical Center
Division of Health Care Financing & Policy
Nevada State Health Division
Silver Sage Center for Family Medicine
Office of Health Statistics and Surveillance,
Nevada State Health Division
Carson City Department of Health and Human
Services
Fritz Reese
Bernadette Longo, PhD, MS
Mary Cotay, RN
Teresa Angermann, D.O.
Alicia Hansen, MS
Cortney Bloomer, MPH
Social/Behavioral Health Emphasis
Center for the Application of Substance
Abuse Technologies
Family Ties of Nevada (people with disabilities)
Washoe County Department of Juvenile
Services
University of California San Diego Pace
Project
Washoe County District Health Department
Eric Albers, PhD
Marcia O’Malley
Joseph Haas, MD
Greg Norman, PhD
Saint Mary's Regional Medical Center
WaterFit
TM
Fitness Education
Sanford Center for Aging
Northern Nevada HOPES (HIV/AIDS)
Washoe County Health District;
Environmental Health Division
Rural Western Coalition Partnership
Carson City School District/ Nevada State
Health Division
Leslie Elliott PhD, MPH
Mike Johnson, MS, Vice President,
Community Health and Mission
Integration
Mary Sanders, PhD
Teresa Sacks, MPH
Leah Thompson, MPH
Jeanne Rucker, REHS
Deborah Loesch-Griffin, PhD
Barbara Howe, MS RD
2.4.c. Data on the number of students receiving a waiver of the practice experience for each of the last three years.
Not applicable. No students have received a waiver.
Final Self Study, October 2010 Page 60
UNR School of Community Health Sciences
2.4.d. Data on the number of preventive medicine, occupational medicine, aerospace medicine, and public health and general preventive medicine residents completing the academic program for each of the last three years, along with information on their practicum rotations.
Not applicable. We are currently discussing the option of residency placements with the School of Medicine.
2.4.e. Assessment of the extent to which this criterion is met.
This criterion is met.
Strengths
In restructuring the internship course and requiring more student work hours, students and preceptors alike note the practicability of the changes, suggesting a greater opportunity for learning through the new hour requirements, and parallel to that, the internship site and preceptor are provided with a greater product.
Student internships are turning into employment opportunities.
With the addition of a 25% FTE internship coordinator in 2009, the internship has become more centralized and streamlined, creating a more standardized process.
Suggested Improvements
As noted above, the department was able to commit 25% FTE for an internship coordinator in 2009, to facilitate the MPH internship program, which has significantly improved processes. To further improve the program, however, an increase in FTE for this position is recommended. Providing at least 50% FTE, and preferably 100% FTE, for this position would substantially improve the coordinator’s ability to develop internships through engagement with students, preceptors, and faculty advisors, and would allow time for this person to advocate within the community for internship partnerships with a variety of organizations. Providing for greater coordinator time will become essential as the MPH program grows in size and develops greater visibility within the public health community.
Final Self Study, October 2010 Page 61
UNR School of Community Health Sciences
2.5 Culminating Experience. All professional degree programs identified in the institutional matrix shall assure that each student demonstrates skills and integration of knowledge though a culminating experience.
2.5.a. Identification of the culminating experience required for each degree program. If this is common across the program’s professional degree programs, it need be described only once. If it varies by degree or specialty area, sufficient information must be provided to assess compliance by each.
According to the Council on Education for Public Health (CEPH) all MPH students must demonstrate skills and integration of knowledge through a culminating experience. A culminating experience is one that requires a student to synthesize and integrate knowledge acquired in coursework and other learning experiences and to apply theory and principles in a situation that approximates some aspect of professional practice.
The capstone course was initiated in 2010 to formalize the culminating experience and emphasize professional development prior to graduation. Initial student and faculty evaluations were very positive, but highlighted the need to more closely integrate the field studies, professional paper, and capstone course. The importance of faculty advisor participation in all aspects of the culminating experience also became evident. The revised culminating experience structure was developed with student and faculty feedback and is presented below.
The MPH culminating experience at UNR has three components: 1) the internship/field studies;
2) the MPH professional paper; and 3) the capstone course. Through the MPH culminating experience students will demonstrate proficiency in public health knowledge and competencies.
Successful completion of all three components of the culminating experience is evidence that the
MPH graduate is prepared to become a public health professional.
After students complete their internship experience (described in section 2.4), they are prepared to complete their MPH professional paper and the capstone course.
MPH Professional Paper
Students complete a MPH professional paper that represents the culmination and mastery of the
MPH curriculum. The MPH professional paper is typically be based on the student’s internship experience, but occasionally it could be related to faculty-student research, or another field experience. Some examples of experience that could be the basis of the paper include: needs assessment, program planning, program evaluation, product or curriculum development, a research report (analysis of primary or secondary data), policy analysis, or grant development.
Before beginning the MPH professional paper, students must: 1) establish a professional paper committee; 2) obtain committee approval for their proposed paper topic; and 3) obtain committee signatures on their program of study. Please see the MPH professional paper approval form
(Appendix D) and timeline (Table 2.5.a.) for more information.
Final Self Study, October 2010 Page 62
UNR School of Community Health Sciences
Table 2.5.a.
MPH Professional Paper and Presentation Timeline (2010 / 2011).
Task
Completion of 6 field studies units
Deadline
Summer / Fall Before Capstone Enrollment
Establish committee:
-Chair, -Grad School Rep, -Agency Rep. (if possible) –Third committee member (if needed)
MPH professional paper orientation: Mandatory
Meeting
-Paper guidelines & due dates
-Professional writing
-Obtaining sources & citation
-Professional development topics for Capstone
Committee meeting to propose MPH professional paper topic
MPH professional paper description / approval form signed by committee members
Program of study (POS) signed by all committee members
September 15
October 13
October 31
October 31
October 31
Begin Literature Review
Spring Semester / Capstone Begins
Literature Review turned in to Chair
Chair provides feedback on Lit Review
Fall Semester & Winter Break
January 18
January 31
February 11
Methods and Results turned in to Chair February 28
Chair provides feedback on Methods and Results March 11
MPH professional paper (including discussion section) turned in to Chair for review
March 21
Chair works with student on final revision March 21 – April 1
Final professional paper committee review
Final Oral Presentation
Final revisions to culminating experience paper made based on committee feedback
Notice of Completion (NOC) form signed by committee members and turned into MPH graduate director
Notice of Completion (NOC) form signed by committee members and turned into graduate school
Graduation!!! All students make it ( :
April 4
April 18 – April 21
April 28
April 29
May 2
May 13
The professional paper committee must include:
The student’s academic advisor (committee chair)
AND
A graduate faculty member outside the School of Community Health Sciences (graduate school representative)
AND
A professional practice representative typically from the student’s field studies site
(encouraged, but not required)
OR
Final Self Study, October 2010 Page 63
UNR School of Community Health Sciences
Community Health Sciences.
Through the MPH professional paper students will:
If a professional practice representative is unavailable, a third committee member must be added. This committee member can be inside or outside the School of
Demonstrate effective written and oral skills for communicating with different audiences in the context of professional and public health activities (ASPH Competency F7)
Communicate epidemiologic information to lay and professional audiences (ASPH
Competency C8)
Apply evidence-based principles and scientific knowledge base to critical evaluation and decision-making in public health (ASPH Competency J3)
Analyze determinants of health and disease using an ecological framework (ASPH
Competency J6)
In addition, students will work with their faculty advisor to choose one competency within their area of emphasis and one cross-cutting competency that they will emphasize in their professional paper.
The MPH professional paper will typically be 25-30 pages (Double-spaced 12 pt. font and 1 inch margins), not including references and appendices. The professional paper should include the following:
Abstract: The abstract should be 250 words and should follow a structured format: background, methods, results, and conclusion.
Background: The background section should describe the significance of the public health issue being addressed. Public health theory and peer reviewed literature should be summarized to set the stage for the objectives or research questions that will be addressed in the professional paper. If appropriate the background section could also include a description of the organization or setting in which the project was carried out
(approximately 8-10 pages).
Methods: This section will vary depending on the nature of the student’s project but should clearly describe the what, where, when, and how of the project. For research projects, the methods section should include standard sub-headings such as: participants/procedures; measures; and analyses (approximately 2-5 pages).
Results: The results section should include the final product that was produced by the student. This section will vary in length and format depending on the nature of the project. For example, the results could include a summary of research findings, a program or evaluation plan, a grant proposal, a training curriculum, or policy analysis
(approximately 5-10 pages).
Final Self Study, October 2010 Page 64
UNR School of Community Health Sciences
Discussion: This section should summarize the main findings and the public health impact of the project. The results should be interpreted in the context of previous research and a clear discussion of implications for future research, program or intervention development, and policy should be included (approximately 5 pages).
References and Bibliography: Use a standard documentation style, such as APA or AMA
Guidelines.
Appendices: Appendices may be included, but will not count toward the page requirement.
If the work contributing to the professional paper involved human subjects, students must receive appropriate approval from the University of Nevada, Reno Office of Human Research
Protection. IRB approval must be obtained before any data collection with human subjects can begin.
Professional Paper Evaluation and Oral
Committees will use a standard rubric based on the MPH paper guidelines and competencies to evaluate the student’s MPH professional paper (see Appendix K). Students will orally present their professional paper to their committee, other MPH faculty, and MPH students during spring semester. A standard rubric will also be used to evaluate the oral presentation. Following the presentation and general questions from the audience, the committee will be given time alone to discuss whether the student has provided evidence of mastery of the MPH curriculum and competencies in their professional paper and presentation.
The MPH Capstone Course
The MPH Capstone Course will provide the structure students need to complete their professional paper and oral presentation. Students will be given the opportunity for peer evaluation on their MPH professional paper in the capstone course. In addition, students will receive points in the capstone course for meeting paper deadlines. This is intended to provide structure and peer-support as students complete their professional paper. However, papers will not be graded in the capstone course and the advisor/committee chair is responsible for ensuring that the student’s paper is of sufficient academic rigor for committee review and presentation.
The capstone course will also focus on public speaking and students will be given the opportunity to practice their presentation as a capstone assignment.
The capstone course will also address professional development. Special sessions and assignments related to professional development include: group facilitation and mediation, public speaking, how to be a good supervisor, resume development, how to land a job, public health ethics, and the future of public health as a profession. Near the end of the course students complete a competency assessment to identify competencies that need to be further developed.
Students use this assessment to develop a post-graduation professional development plan.
Through the MPH capstone course, students will:
Final Self Study, October 2010 Page 65
UNR School of Community Health Sciences
Embrace a definition of public health that captures the unique characteristics of the field
(e.g., population-focused, community-oriented, prevention-motivated and rooted in social justice) and how these contribute to professional practice (J9)
Value commitment to lifelong learning and professional service including active participation in professional organizations (J11)
Apply basic principles of ethical analysis (e.g. the Public Health Code of Ethics, human rights framework, other moral theories) to issues of public health practice and policy (J2)
One competency within area of emphasis (Epi/Biostats or Social/Behavioral) that needs development (student choice)
One cross-cutting competency that needs development (student choice)
2.5.b. Assessment of the extent to which this criterion is met.
This criterion has been met with commentary.
Strengths
The culminating experience has been revised with input from students and faculty. The culminating experience retains the positive aspects of a rigorous committee structure, but also promotes a cohort experience and shared learning experiences with the students.
The internship, professional paper, and the capstone course are integrated into a comprehensive culminating experience.
The competencies for the professional paper and the capstone course balance academic and professional development.
The committee approval and evaluation process for the professional paper is more formalized and advisor expectations are more clearly articulated.
Suggested Improvements
The culminating experience has been revised and will need to be closely evaluated.
Students graduating spring 2011 will conduct an anonymous evaluation of the culminating experience. In addition, faculty advisors and committee members will provide feedback on the process, new evaluation tools, and student mastery. The graduate committee will review all evaluation data and incorporate revisions in the next academic year.
Final Self Study, October 2010 Page 66
UNR School of Community Health Sciences
2.6. Required Competencies. For each degree program and area of specialization within each program identified in the instructional matrix, there shall be clearly stated competencies that guide the development of educational programs.
2.6.a. Identification of core public health competencies that all MPH or equivalent professional Master degree students are expected to achieve through their courses of study.
The MPH Program has identified public health competencies that all students must achieve by completing their core courses of study (biostatistics, environmental health, epidemiology, health policy and administration, social and behavioral health, research methods, field studies, and the capstone course). A competency subcommittee made up of MPH core course instructors and a student representative reviewed and adapted the competencies set forth by the Association of
Schools of Public Health (ASPH).
Core course instructors developed competency plans for each course. The competency plan linked the chosen competencies with readings, assignments, and assessment/evaluation methods.
Instructors noted whether the competency was introduced or practiced and identified culminating assessment activities for the course as a whole (Appendices E.1-E.8: Core Course Competency
Plans). The MPH Core Competencies are presented in Table 2.6.a.
Table 2.6.a. UNR MPH Core Competencies.
Domain: Biostatistics
A1. Describe the roles biostatistics serves in the discipline of public health
A2. Describe basic concepts of probability, random variation and commonly used statistical probability distributions
A3. Describe preferred methodological alternatives to commonly used statistical methods when assumptions are not met
A4. Distinguish among the different measurement scales and the implications for selection of statistical methods to be used based on these distinctions
A5. Apply descriptive techniques commonly used to summarize public health data
A6. Apply common statistical methods for inference
A7. Apply descriptive and inferential methodologies according to the type of study design for answering a particular research question
A9. Interpret results of statistical analyses found in public health studies
Domain: Environmental Health Sciences
B1. Describe the direct and indirect human, ecological and safety effects of major environmental and occupational agents
B2. Describe genetic, physiologic and psychosocial factors that affect susceptibility to adverse health outcomes following exposure to environmental hazards
B3. Describe federal and state regulatory programs, guidelines and authorities that control environmental health issues
B4. Specify current environmental risk assessment methods
B5. Specify approaches for assessing, preventing and controlling environmental hazards that pose risks to human health and safety
B6. Explain the general mechanisms of toxicity in eliciting a toxic response to various environmental exposures
Final Self Study, October 2010 Page 67
UNR School of Community Health Sciences
B7. Discuss various risk management and risk communication approaches in relation to issues of environmental justice and equity
B8. Develop a testable model of environmental insult
Domain: Epidemiology
C1. Identify key sources of data for epidemiologic purposes
C2. Identify the principles and limitations of public health screening programs
C3. Describe a public health problem in terms of magnitude, person, time, and place
C4. Explain the importance of epidemiology for informing scientific, ethical, economic and political discussion of health issues
C5. Comprehend basic ethical and legal principles pertaining to the collection, maintenance, use and dissemination of epidemiologic data
C6. Understand and apply the basic terminology and definitions of epidemiology
C7. Calculate basic epidemiology measures
C8. Communicate epidemiologic information to lay and professional audiences
C9. Draw appropriate inferences from epidemiologic data
-Understand causal inference and hypothesis testing;
-Describe the purposes, strengths, and weaknesses of various study designs;
-Identify random error and systematic error (bias)
C10. Evaluate the strengths and limitations of epidemiologic reports
D1. Identify the main components and issues of the organization, financing and delivery of health services and public health systems in the US and the global community.
D4. Identify and apply the basic policy process for improving the health status of populations.
D7. Discuss, understand, and apply quality and performance improvement concepts to address organizational performance issues.
D8. Discuss and apply "systems thinking" for resolving organizational problems.
Domain: Social and Behavioral Sciences
E1. Identify basic theories, concepts and models from a range of social and behavioral disciplines that are used in public health research and practice
E2. Identify the causes of social and behavioral factors that affect health of individuals and populations
E3. Indentify individual, organizational, and community concerns, assets, resources and deficits for social and behavioral science interventions.
E6. Describe the role of social and community factors in both the onset and solution of public health problems
E7. Describe the merits of social and behavioral science interventions and policies
E10. Specify multiple targets and levels of intervention for social and behavioral science programs and/or policies
Domain: Communication and Informatics
F7. Demonstrate effective written and oral skills for communicating with different audiences in the context of professional public health activities
Domain: Diversity and Culture
G3. Explain why cultural competence alone cannot address health disparity
G6. Apply the principles of community-based participatory research to improve health in diverse populations
Final Self Study, October 2010 Page 68
UNR School of Community Health Sciences
Domain: Leadership
H2. Describe alternative strategies for collaboration and partnership among organizations, focused on public health goals.
H5. Demonstrate team building, negotiation, and conflict management skills.
H6. Demonstrate transparency, integrity, and honesty in all actions
H8. Apply social justice and human rights principles when addressing community needs
Domain: Professionalism
J2. Apply basic principles of ethical analysis (e.g. Public Health Code of Ethics, human rights framework, other moral theories) to issues of public health practice and policy
J3. Apply evidence-based principles and the scientific knowledge base to critical evaluation and decision-making in public health.
J5. Promote high standards of personal and organizational integrity, compassion, honesty, and respect for all people
J6. Analyze determinants of health and disease using an ecological framework
J9. Embrace a definition of public health that captures the unique characteristics of the field (e.g. population-focused, community-oriented, prevention-motivated and rooted in social justice) and how these contribute to professional practice.
J10. Appreciate the importance of working collaboratively with diverse communities and constituencies (e.g. researchers, practitioners, agencies and organizations)
J11. Value commitment to lifelong learning and professional service including active participation in professional organizations
Domain: Program Planning
K7. Differentiate between qualitative and quantitative evaluation methods in relation to their strengths, limitations, and appropriate uses, and emphases on reliability and validity
2.6.b. A matrix that identifies the learning experiences by which the core public health competencies are met. If this is common across the program, a single matrix will suffice. If it varies by degree or specialty area, sufficient information must be provided to assess compliance by each.
Core MPH competencies are mapped to required courses demonstrating the learning experiences by which core public health competencies are met (Appendix F). Specific details on the learning and assessment activities for competencies in each course can be found in Appendices E.1-E.7.
2.6.c. Identification of a set of competencies for each program of study identified in the instructional matrix, including professional and academic degree curricula.
In addition to the core competencies, faculty and a student representative in each MPH area of specialization identified specific competencies for required courses. ASPH competencies were the foundation for this process, but additional competencies for each area of specialization were also developed. The competencies for each area of specialization are listed in Appendix H
(Epidemiology) and Appendix J (Social and Behavioral Health). Individual competency plans for required courses in Epidemiology (Appendices G.1-G.6) and Social and Behavioral Health
(Appendices I.1-I.5) were also developed by course instructors to describe the learning and assessment activities associated with each competency.
Final Self Study, October 2010 Page 69
UNR School of Community Health Sciences
2.6.d. A description of the manner in which competencies are developed, used and made available to students.
Competency Development. MPH core competencies were identified by a competency subcommittee consisting of faculty who teach required core courses and a student representative.
Core course instructors developed competency plans that mapped each competency to specific learning and assessment activities. This process encouraged thoughtful reflection on the course competencies, learning objectives, learning activities, and assessment methods. After all competency plans were developed, the competency subcommittee reconvened to approve individual course competency plans and to develop the matrix that maps all core competencies with the required courses (Appendix F). The core competency matrix was approved by faculty in the School of Community Health Sciences on April 7, 2010.
A similar process was followed for the development of area of specialization course competency plans and the competency matrix for each area of specialization. However, the competency subcommittees consisted of faculty and students in each area of specialization. The competency matrix for epidemiology (Appendix H) was approved by faculty in epidemiology and biostatistics on May 7, 2010. The competency matrix for social and behavioral health sciences
(Appendix J) was approved by faculty on May 5, 2010.
Competency Use. The core and area of specialization competencies form the basis for all MPH
Program curriculum development, assessment, and revision. Although this process has only begun, the competency mapping for each area of specialization helped identify gaps and duplication in our curriculum. The review of core and area of specialization competencies will continue on an annual basis.
Student progress in mastering the core and area of specialization competencies is assessed two times during the semester (before the drop date and near the end of the semester). This process was piloted spring semester 2010 and faculty found it to be a useful and objective process for monitoring student progress and identifying potential problems in required courses.
The competencies also form the basis for MPH Program evaluation. Beginning fall semester
2010 students will engage in a self-reflection of their mastery of practice competencies for all core and area of emphasis required courses. This self-reflection process was pilot tested in spring
2010 in two MPH core courses.
Finally, the competencies form the basis for student planning and participation in field studies and the culminating capstone course. Students select competencies to target for individual development during each course and complete self-assessment of chosen competencies.
Students in the capstone course also identify competencies that they plan to address through professional development after graduation.
Availability of Competencies to Students. All syllabi for MPH core courses and required courses for each area of specialization include the approved competencies. In addition, beginning fall semester 2010, individual instructors will make the competency plans available to students. This
Final Self Study, October 2010 Page 70
UNR School of Community Health Sciences gives students a clear indication of how the course competencies are linked to readings, assignments, and assessment activities.
All core competencies and areas of specialization competencies are available to students on the
MPH Program website, as well as in the student/advisor handbook. Beginning fall semester
2010, students will be informed of the required competencies and how they will be acquired and evaluated during orientation and individual meetings with their faculty advisors.
2.6.e. A description of the manner in which the program periodically assesses the changing needs of public health practice and uses this information to establish the competencies for its educational programs.
As discussed in Section 1.2 “Evaluation and Planning”, a comprehensive needs assessment of employers was conducted to determine whether there was interest and support for an MPH degree in the area. The results showed broad support for graduate-level public health training and reflecting that interest, since its inception, the program has attracted a large number of public health professionals in the area. Since that time, the annual employer survey (survey instruments provided in onsite resource file) has been the biggest source of information about skills needed by our graduates. The survey results demonstrate that employers of UNR MPH graduates value ethics, working collaboratively, cultural diversity, and strong written and oral communication skills. The MPH curriculum has specifically emphasized these skills and the competency committee selected competencies that will ensure that these areas are adequately covered in our required courses.
From 2000 to spring 2010 the SCHS alumni survey asked students to evaluate the usefulness of their coursework. In 2010, this survey will be revised to more completely capture our alumni’s evaluation of their competency attainment and the relevance of the existing competencies in their work. In addition, the previous college in which the SCHS was located had an Associate Dean for Workforce Development whose charge was to work closely with public health professionals to monitor their training needs. The Associate Dean held a series of forums in which input on educational training priorities was obtained (see Appendix L).
To ensure that the SCHS competencies reflect the changing needs of public health practice, prioritized competencies were distributed to four representatives from the Nevada State Health
Division for their review and input. In five years, we will conduct a more representative statewide survey of public health practitioners to identify the competencies and skills they believe are essential for MPH graduates.
Finally, faculty enrolled in the 2009-2010 Great Basin Public Health Leadership Institute participated in a roundtable session with public health practitioners to identify recent workforce development needs. The participants emphasized the importance of students’ understanding the business of public health such as budgeting, grant proposal writing, and the structure of the public health system in Nevada including its political pressures and how to work with the state legislature. These results support a 2006 needs assessment of the NSHD that was conducted by
UNLV and the Great Basin Public Health Leadership Institute. The results have been shared with representatives of the SCHS competency committee and clearly indicate a continuing need
Final Self Study, October 2010 Page 71
UNR School of Community Health Sciences and interest in MPH coursework by state employees. Respondents were particularly interested in training that could be applied to a degree or certificate program. In addition, respondents were interested in on-site and online training options. These are two areas in particular in which the
SCHS could effectively fulfill the NSHD staff’s needs in the future.
2.6.f. Assessment of the extent to which the criterion is met.
This criterion is met.
Strengths
A thorough competency-based curriculum developed with broad input is in place.
Competencies underlie the entire curriculum.
Suggested Improvements
Further evaluation of the competencies is needed. For example, the number of competencies may be too high. Instructors have struggled with assessing whether students are mastering every identified competency. The competencies were first developed with the core public health faculty. They were then instituted in all required epidemiology and social/behavioral courses. Instructors of these latter courses are still becoming familiar with the competency assessment process. To make sure the competency-based curriculum is fully implemented and evaluated by all faculty, problems must be discussed and future assistance may be needed for faculty. How best to make this happen is an ongoing discussion among faculty. However, faculty appreciate the benefits of good assessment (including multiple measures), as it helps them to determine if the competencies were mastered.
A more recent and thorough needs assessment of employer-identified competencies needs to be conducted. In fall 2010, a taskforce was developed to conduct another needs assessment. The taskforce includes the school’s Director of the Center for Program
Evaluation and the division’s Director of Internal/External Affiars.
Final Self Study, October 2010 Page 72
UNR School of Community Health Sciences
2.7 Assessment Procedures. There shall be procedures for assessing and documenting the extent to which each student has demonstrated competence in the required areas of performance.
2.7.a. Description of the procedures used for monitoring and evaluating student progress in achieving the expected competencies.
Every required MPH and area of specialization course has a competency plan (described in section 2.6). The competency plan includes assessment and evaluation methods that serve the basis for monitoring whether students are achieving expected competencies (e.g., exams, assignments, papers, projects, and final course grades). Using the evaluation methods identified in the competency plans, faculty members meet twice a semester to assess student progress in mastering the core and area of specialization competencies (before the drop date and near the end of the semester). Competency assessment data from fall semester 2009 and spring semester
2010 for the core MPH courses are presented in Appendices E.1 –E.8. Beginning fall semester
2010 all core and area of specialization course instructors will have students provide selfreflection of attainment of course competencies. This student self reflection was piloted in two core course during spring 2010 and provided valuable feedback for the core course instructors.
The internship preceptor completes a student evaluation based on competencies identified in the
Memorandum of Understanding (MOU) (see section 2.4 Practical Skills). In addition, students establish an MPH professional paper committee (student advisor, graduate school representative, and internship preceptor (when available)) that evaluates students’ achievement of course- and student-identified competencies using a standard evaluation tool and approves their final paper and presentation (Appendix K) based on the student’s ability to synthesize public health knowledge and apply it to the solution of public health problems.
2.7.b. Identification of outcomes that serve as measures by which the program will evaluate student achievement in each degree program, and presentation of data assessing the program’s performance against those measures for each of the last three years.
Final Self Study, October 2010 Page 73
UNR School of Community Health Sciences
Table 2.7.b. Student Achievement Outcomes, Targets, and Data for Last 3 Years.
1) Goal: “To prepare future public health practitioners, researchers, educators and leaders.”
Objective 2): Education/Training
2007 to 2008
Data
92% 2a. By 2011, 90% of MPH students will receive grades of B or higher as evidence of partial attainment of core MPH and emphasis-specific competencies.
2b. By 2011, 95% of MPH students will receive approval of their culminating project proposal by their committee on the first attempt.
New objective: data not yet available
2c. By 2011, 30% of MPH students will be involved with faculty in research activities.
14%
2008 to 2009 2009 to 2010
Data Data
84% 86%
New objective: data not yet available
21%
New objective: data not yet available
22%
2d. By 2011, 10% of current MPH students or graduates within the last 5 years will be the primary author or a co-author on a publication (peerreviewed).
2e. By 2011, 20% of current MPH students or graduates within the last 5 years will be the primary author or a co-author on a presentation at a scientific conference (peer-reviewed).
2f. By 2011, 35% of MPH students will be involved in leadership roles and providing service to the community or university.
8%
11%
100%
5%
13%
90%
12%
13%
73%
Final Self Study, October 2010 Page 74
UNR School of Community Health Sciences
2.7.c. If the outcome measures selected by the program do not include degree completion rates and job placement experience, then data for these two additional indicators must be provided, including experiential data for each of the three years. If degree completion rates, in the normal time period for degree completion, are less than 80%, an explanation must be provided. If job placement, within 12 months following award of the degree, is less than 80% of the graduates, an explanation must be provided.
Table 2.7.c.
Alumni Achievement Outcomes, Targets, and Data for Last 3 Years.
2007 to 2008 2008 to 2009 2009 to 2010
Data Data Data
1) Goal: “To prepare future public health practitioners, researchers, educators and leaders.”
Cont.
Objective 3): Graduation/Post-Graduation
3a. By 2011, 90% of full-time MPH students will complete their degree within 3 years of matriculation.
3b. By 2011, 75% of MPH graduates will become employed in public health or settings closely related to their degree within 6 months of graduation.
71%
92%
75%
*Historical graduation rate is 80% within three years. Three years have not yet elapsed for this cohort.
57%
N/A
*This cohort just entered in fall 2009.
Data not yet available
8% 29% 3c. By 2011, 5% of MPH graduates will be admitted to a program for further academic training (PhD, MD, etc.).
3d. By 2011, 10% of MPH graduates will have local or national leadership positions in public health.
15% 14%
Data not yet available
Data not yet available
3e. 60% of employed UNR MPH graduates are located in Nevada and the
Intermountain West by 2011.
75% 86% Data not yet available
Final Self Study, October 2010 Page 75
UNR School of Community Health Sciences
All but 1 student accepted within the last 7 years has met the university requirement of 6 years to complete the master’s degree which is a rate well over 90%. Historically, 80% of students have completed the degree within 3 years which is the school’s target for students as listed in objective 3a. Prior to the 2007-2008 cohort, the time-to-graduation rate for full-time students entering in 2005 was 100%, 70% in the 2006 cohort, and 71% for the 2007 cohort. Because our cohort size is small, our rate drops below 80% as a result of a few students. For example, 2 of the 10 students entering in 2006 did not continue the program beyond the first semester and the third student who did not finish left for medical school. Of the remaining 7 students, all finished within 3 years (70%). The curriculum was revised to encourage more efficient matriculation of the students in part based on concerns about time to graduation.
2.7.d. A table showing the destination of graduates for each of the last three years. The table must include at least the number and percentage of graduates by program area each year going to a) government (state, local, federal), b) nonprofit organization, c) hospital or health care delivery facility, d) private practice, e) university or research institute, f) proprietary organization (industry, pharmaceutical company, consulting), g) further education, h) non-health related employment, or i) not employed. See CEPH Data
Template D.
Final Self Study, October 2010 Page 76
UNR School of Community Health Sciences
Table 2.7.d. Destination of Graduates by Program Area for Each of the Last 3 Years.
Government
# %
Nonprofit Health Care Private
Practice
# % # % # %
University/
Research
# %
Proprietary Further
# %
Education
#
Non-
Health
Related
% # %
1) Academic Year 2007-2008
MPH -
Epidemiology
2 15% 0 0%
MPH-Social
Behavioral/Health
0 0% 0 0%
0 0%
0 0%
0
0
MSN/MPH*
MPH –
Generalist*
2) Academic Year 2008-2009
MPH -
Epidemiology
0 0%
MPH-Social
Behavioral/Health
0 0% 0 0% 1 8%
1 8% 1 8% 1 8%
0 0%
0 0%
0 0%
0 0%
0
0
0
1 13% 0
MSN/MPH*
MPH –
Generalist**
0 0% 0 0%
1 13% 0 0%
0 0% 0
1 13% 0
3) Academic Year 2009-2010
MPH - 2 14% 0 0% 0 0% 0
Epidemiology
MPH-Social 0 0% 0 0% 0 0%
Behavioral/Health
*Not accepting students into this area of emphasis
**No longer offering this area of emphasis
0
0%
0%
0%
0%
0%
0%
0%
0%
0%
0%
0
1
0
1
0%
0%
0
8% 0
0
1 13% 0
1 0% 0
1 13% 0
7% 0
4 29% 0
0%
0%
0%
0%
0%
0%
1 8% 0 0%
0 0%
0 0% 0 0% 0 0%
2 15% 2 15% 0 0%
1 13
%
0 0%
0 0%
1 13
%
0% 4 29
%
0% 2 14
%
0 0%
0 0%
0 0%
0 0%
0 0%
0 0%
0 0%
Not
Employed
# %
0 0%
0 0%
0 0%
1 8%
0 0%
0 0%
0 0%
0 0%
0 0% 0 0%
0 0% 1 7%
Final Self Study, October 2010 Page 77
UNR School of Community Health Sciences
MPH program alumni have obtained positions at the highest levels of government such as the
Nevada State Epidemiologist, the Director of the Carson City Health and Human Services, and the Director of Indian Health Services, Office of Public Health for 24 states. They have also obtained leadership positions in nonprofit and private settings such as Carson Tahoe Regional
Medical Center, the Center for Health at Saint Mary's Regional Medical Center, and Nevada
Energy (power company). Apart from two students who are focusing on family or young children, we are not aware of any alumni who does not have a job utilizing their MPH training.
We believe that our alumni’s success is one of the strongest outcomes of our program.
2.7.e. In public health fields where there is certification of professional competence, data on the performance of the program’s graduates on these national examinations for each of the last three years.
Since 2000, we have tracked 5 MPH alumni who completed the Certified Health Educator
Specialist Exam (CHES). Our alumni have a 100% pass rate.
2.7.f. Data describing results from periodic assessments of alumni and employers of graduates regarding the ability of the program’s graduates to effectively perform the competencies in a practice setting.
Tables 2.7.f.1. and 2.7.f.2. present the results from the employer and alumni surveys conducted by UNR’s Office of Assessment. Overall, the feedback on the program is positive; however the results should be interpreted cautiously as the response rates are very low so comments are more anecdotal.
Table 2.7.f.1. Employer Survey 2002-2009 (N=5)
% responding “Very” or
“Somewhat Prepared”
“How prepared were UNR MPH graduates to…
…carry out writing tasks
…express themselves orally
100%
90%
…use quantitative methods
…develop solutions to work-related problems
…think critically
…work cooperatively on a team
…use computers or other technology
90%
100%
100%
100%
100%
…work in a culturally diverse environment
…consider the ethical implications of his/her behavior
100%
100%
“Generally, how satisfied are you with this graduate?” 100% responded “Very” or
“Somewhat Satisfied”
Final Self Study, October 2010 Page 78
UNR School of Community Health Sciences
Table 2.7.f.2. Alumni Survey 2007-2009 (N=11)
% responding “Excellent” or “Good”
Overall quality of program
Program preparation for career path
73% (8/11)
82% (9/11)
Level of student to faculty interactions
Quality of advisement
91% (10/11)
45%
(55% responded “fair” in 2007-2008; in
2009, 100% of respondents rated it as
“excellent” or “good”)
2.7.g. Assessment of the extent to which this criterion is met.
This criterion is met.
Strengths
The program has thorough assessment procedures to monitor student performance in the classroom, during fieldwork and in the culminating experience.
Grade Point Averages of entering students generally meet or exceed program requirements and the majority of students are progressing through the curriculum with a grade of B or higher.
The time to complete degrees is at 80% measured since the inception of the program.
Graduates have high employment and continuing education rates and have obtained leadership positions in the public health field. Our alumni are doing exceptionally well professionally. Their willingness to assume leadership positions is especially encouraging as demonstrated by the board of directors for the Nevada Public Health
Association (many are UNR MPH alumni).
Suggested Improvements
Response rates for both the alumni and employer surveys need to be increased. To address this, in fall 2010, the school’s Center for Program Evaluation agreed to oversee the assessment of the graduate program which should help increase responses.
The employer and alumni survey questions are not as specific as needed to assess competencies associated with epidemiology vs. social/behavioral health. Separate surveys may be needed.
Encourage graduates to take the CHES. To accomplish this, the CHES and other certified exams (CPH) have been discussed in MPH classes. Advisors, in particular, have been discussing the importance of these certifications. One current student will be sitting for the CEPH exam in October 2010.
Final Self Study, October 2010 Page 79
UNR School of Community Health Sciences
2.8 Academic Degrees. If the program also offers curricula for academic degrees, students perusing them shall obtain a broad instruction to public health, as well as an understanding about how their discipline-based specialization contributes to achieving the goal of public health.
Not applicable.
Final Self Study, October 2010 Page 80
UNR School of Community Health Sciences
2.9 Doctoral Degrees. The program may offer doctoral degree programs in the future, if consistent with its mission and resources.
Not applicable.
Final Self Study, October 2010 Page 81
UNR School of Community Health Sciences
2.10 Joint Degrees. If the program offers joint degree programs, the required curriculum for the professional public health degree shall be equivalent to that required for a separate public health degree.
2.10.a. Joint Degree Programs Offered. Identification of joint degree programs offered by the program and a description of the requirements for each.
SCHS is approved to offer two post
‐ baccalaureate joint degree programs: the (master of science in nursing) MSN/MPH and the MD/MPH.
In addition to the joint degrees, we collaborate with two other groups on campus. With the
College of Business, an MBA student may have a core emphasis in health care administration and policy. We also collaborate with the School of Medicine Family Practice Residency
Program to coordinate the scheduling of MPH courses and we provide advisement of suggested course progression for their residents; however there is no combined Family Practice Residency
Program/MPH program.
MD/MPH. Our first four MD/MPH students started with us in fall 2009, one year earlier than we expected. Initially in our discussions with the University of Nevada School of Medicine
(UNSOM), the plan was for medical students to start a MPH program of study (POS) after their third year of medical school and their clinical clerkships. However, a new faculty member, Dr.
Jason Crawford, who arrived from a joint MD/MPH program in Arizona, created much enthusiasm around the MPH for medical students. He suggested that the students start earlier
(after their second year), before starting their clinical clerkships, so that they would have their background in public health before going out into clinical medicine. We all agreed to go forward with an earlier start with the understanding that we would assess the results after the experience was concluded.
For the MD/MPH, we created an accelerated one year POS for any MPH student (including medical students) wanting to get all coursework completed for the MPH in one year, then the field studies and capstone course would follow in year 2.
There is a 6-unit overlap with the medical students in their clinical rotations which will have a public health emphasis and therefore, may be used for their MPH internship credits. Upon completion of the clinical rotations, the students will return for the following spring semester to complete their MPH capstone course. Apart from the 6-unit overlap, MD/MPH students are required to complete all other requirements just like other MPH students, and to demonstrate attainment of all identified public health competencies.
The success and enthusiasm for this dual degree has now created the impetus for Family Practice
Residents to obtain their MPH during their residency time and POS have been created for these two students as well who started in spring 2010.
Overall, these two programs have elevated our student diversity to a higher level, increased the collaborative nature of public health discussions, and supported students with broader academic interests to be part of the public health profession.
Final Self Study, October 2010 Page 82
UNR School of Community Health Sciences
MSN/MPH. In the original version of the dual MPH/MSN degree program approved in 2004,
MSN students took the core MPH courses, then completed a joint professional project with the
MPH and MSN programs. They were not required to complete a specialization within public health which was a concern for faculty. We also heard feedback from alumni with this dual degree that they did not do enough coursework in the MPH side of the dual degree.
In the current version (in the process of curricular approvals), the students in this program select a specialization in both the MSN-nursing educator, clinical nurse leader (CNL), and family nurse practitioner (FNP) as well as the MPH-epidemiology and social behavioral health. There is a 6 credit overlap in the area of field studies (internship) with the MSN clinical experiences in
NURS 760. However, there must be a public health emphasis in what their experiences are in their clinical experience. As with the MD/MPH, the MSN/MPH students are required to complete all other requirements expected of the other MPH students, and to demonstrate attainment of all identified public health competencies.
Until the new curriculum is approved, we are not accepting students into this dual degree program. This is why we are not submitting the dual MSN/MPH as part of the accreditation unit at this time. However, there is a close working relationship with UNR’s Orvis School of Nursing and we are committed to making this program of study available and meaningful for those students who might choose this dual degree. We will apply for accreditation review of this program at a future date.
2.10.b. Assessment of the extent to which this criterion is met.
This criterion is met.
Strengths
Our joint degree programs offer curriculum flexibility and excellent faculty advisement.
The support from faculty and administration is strong in both Orvis School of Nursing and UNSOM for these programs. The students in the dual programs benefit from the departments working well together.
The culture of the Division of Health Sciences is supportive of interdisciplinary teamwork and educational training.
Suggested Improvements
SCHS should obtain appropriate approvals for the revised MPH/MSN curriculum and submit them for review by CEPH. Since the prelimary self-study was submitted in June, the revised curriculum has been approved by UNR curricular committees.
The SCHS should continue to develop and implement assessment strategies for the entrance/timing of the MD/MPH program. As an example, the student feedback on entering between the 2 nd
and 3 rd
year of medical school has been positive. Originally, the plan was to have students begin the MPH curriculum after their 3 rd year of medical school. The students recommended that they start at the end of the 2 nd
year so as not to interrupt their clinical training. Faculty incorporated this feedback and based on feedback from students and UNSOM faculty, it appears to be working.
The SCHS should look to develop future dual degrees with College of Business, School of Social Work, Department of Political Science, and Behavioral Psychology.
Final Self Study, October 2010 Page 83
UNR School of Community Health Sciences
The SCHS should implement a BS/MPH program in order to capture our best and brightest undergraduates in Community Health Sciences. It is part of the undergraduate committee’s plan for spring 2011.
The SCHS should devote faculty time for marketing the programs and for further joint degree development. Because resources were identified to assist with assessment, faculty have more time to market the program. In terms of program development, contacts have been made at other schools to learn more about BS/MPH programs as we develop our own BS/MPH program.
Final Self Study, October 2010 Page 84
UNR School of Community Health Sciences
2.11 Distance Education or Executive Degree Programs. If the program offers degree programs using formats of methods other than students attending regular on-site course sessions spread over a standard term, these degree programs must a) be consistent with the mission of the program and within the program’s established areas of expertise; b) be guided by clearly articulated student learning outcomes that are rigorously evaluated; c) be subject to the same quality control processes that other degree programs in the university are; and d) provide planned and evaluated learning experiences that take into consideration and are responsive to the characteristics and needs of adult learners. If the program offers distance education or executive degree programs, it must provide needed support for these programs, including administrative, travel, communication, and student services. The program must have an ongoing program to evaluate the academic effectiveness of the format, to assess teaching and learning methodologies and to systematically use this information to stimulate program improvements.
Not applicable.
Final Self Study, October 2010 Page 85
UNR School of Community Health Sciences
3.0 Creation, Application and Advancement of Knowledge
3.1 Research. The program shall pursue an active research program, consistent with its mission, through which its faculty and students contribute to the knowledge base of the public health disciplines, including research directed at improving the practice of public health.
3.1.a. A description of the program’s research activities, including policies, procedures and practices that support research and scholarly activities .
All of the tenure- and research-track faculty members affiliated with the Program are involved in research. Tenure-track faculty typically dedicate 40% effort to research during the academic year and often do more research during the summer months. Research-track faculty devote a larger proportion of their time to research, usually 50-90%, depending on funding and other duties.
The norm for most members of the faculty is to conduct empirical research. This typically requires grant support and results in publications in peer-reviewed scientific journals. However, there is considerable variation reflecting the range of academic disciplines that make up the program and the backgrounds of individual faculty members, as shown in table 3.1.c. Much of the research conducted by the faculty involves graduate students, typically acting as research assistants. Student research is addressed in more detail in 3.1.e.
For the faculty as a group, both production of scholarly publications and grant support have increased markedly since 2006. This trend is a result of increasing average individual productivity, rather than to increasing faculty size, as the number of faculty members has been essentially constant over this period. Research support is obtained from a variety of federal, state, university and foundation sources, with federal grants and state contracts accounting for the largest amounts of funding. Recent funding sources include: the National Institute for
Occupational Safety and Health (NIOSH), the National Institute of Environmental Health
Sciences (NIEHS), the NIH Center for Research Resources, the Centers for Disease Control and
Prevention (CDC), the Nevada State Health Division, and the Nevada Trust Fund for Public
Health. A number of these projects are community based; these are described in detail in 3.1.b.
Faculty publications in peer-reviewed journals have also increased. Faculty have published their research in respected public health journals, including: American Journal of Epidemiology;
American Journal of Health Behavior, American Journal of Public Health, Archives of
Physiology and Biochemistry, Biometrika, Epidemiology, Environmental Health Perspectives,
International Journal of Health Services, Journal of American Statistical Association, Journal of
Physical Activity and Health, and Occupational and Environmental Medicine.
Faculty involvement in research is highly valued by the School of Community Health Sciences and by the university. Faculty members regularly enter their research accomplishments, including publications, presentations, grant applications, and grant and contract awards into the university’s online database (Digital Measures). Research productivity, along with teaching and service is assessed in both annual evaluations of individual performance and recommendations for merit pay. At the end of each calendar year, Digital Measures is used to generate an annual report summarizing activities and output for the year. The report is the basis of evaluations conducted jointly by a faculty personnel committee, the school director and the vice president.
Evaluations emphasize the importance of scholarship and specifically encourage activities that
Final Self Study, October 2010 Page 86
UNR School of Community Health Sciences contribute to public health knowledge. Evaluations for promotion and tenure also consider research: excellence in research is one of the bases for promotion and granting of tenure.
Faculty research is supported in several other ways. The standard teaching load for most tenuretrack faculty members at the University of Nevada, Reno is three courses per semester.
However, faculty in research-intensive programs (usually those with doctoral degrees) have a reduced load of two courses per semester. Similarly, research-active faculty in the School of
Community Health Sciences normally teach two courses per semester to facilitate greater engagement in research. Newly-hired faculty members typically receive start-up funds to help them establish a research program at the university. The amount of start-up support varies with the discipline and is provided by the office of the vice president for research, the Office of the
Provost, and the vice president for health sciences. The School of Community Health Sciences also assigns state-supported graduate assistants to junior faculty members to help with research.
The university normally offers funds for pilot projects intended to lead to extramural grant applications to junior faculty on a competitive basis, although these grants have not been available in the past 2 years because of budget cuts.
The university also encourages research with several types of financial incentives. A 7.25% share of indirect cost receipts is returned to externally-funded investigators; these funds are deposited in a university account and may be used at the investigator’s discretion for legitimate professional needs, such as books, travel, conference registration and student support. In addition, academic faculty on nine-month contracts may use salary support from grants to fund overload on non-contracted days, most of which occur during the summer. Overload is compensated at the faculty member’s daily rate (equal to academic year salary divided by the number of contracted days). The number of days available for overload is slightly less than half of the number of contracted days, so faculty members with sufficient grant funds can increase their salaries substantially by conducting funded research during the summer.
3.1.b. A description of current community-based research activities and/or those undertaken in collaboration with health agencies and community-based organizations.
Formal research agreements with such agencies should be identified.
The school is committed to community
‐ based research and has a number of projects with most providing opportunities for student involvement. This research is sponsored by federal and state organizations including the National Institutes of Health, the Centers for Disease Control and
Prevention, and the Nevada State Health Division .
The school is home to the Center for Program Evaluation (formerly named the Center for
Partnership Evaluation to emphasize its commitment to community-based partnerships). The
Center has a number of community partners which are listed below in Table 3.1.b. and which include formal agreements to provide community-based evaluation research.
Final Self Study, October 2010 Page 87
UNR School of Community Health Sciences
Table 3.1.b. Community Partners at the Center for Program Evaluation.
Boys and Girls Clubs in Reno and the TahoeCarson City Manager’s Office
Truckee area
Children’s Cabinet Children’s Collaborative of Tahoe-Truckee
City of Las Vegas Neighborhood Services
Department
Community Chest, Incorporated
Community Services Agency Head Start
Program
Clark County Community Resources
Management Division
Community Council On Youth
Douglas County Sheriff’s Office
Douglas County School-Based Partnership
Team
Duck Valley Indian Reservation
Eastern Sierra Institute for Collaborative
Education
Fallon Paiute-Shoshone Tribe
Food Bank of Northern Nevada
Education Collaborative of Washoe County,
Inc.
Family Resource Centers in Washoe and
Storey Counties and the Tahoe-Truckee area
Fort McDermitt Paiute/Shoshone Tribe
Healthy Communities Coalition
International Visitors Council of Northern
Nevada
Job Opportunities In Nevada
I Can Do Anything Even Start Program
Inter-Tribal Council of Nevada
Join Together Northern Nevada
Lyon County Human Services Department Lyon County School District
National Association of Minority Contractors Nevada Commission for National and
Nevada Department of Education
Community Service
Nevada Department of Employment, Training and Rehabilitation
Nevada Health Division’s Bureau of Family
Health Services
Bureau of Community Health, HIV/AIDS
Prevention Care and Surveillance Program
State WIC Program
Nevada Museum of Art
Northern Nevada International Center
Nye Communities Coalition
Reno-Sparks Indian Colony
Tahoe-Truckee Unified School District
United States Department of Agriculture
Nevada Literacy Coalition
Nevada Service-Learning Partnership
Northern Nevada Literacy Council
Partnership of Community Resources
Storey County School District
UC Berkeley Lawrence Hall of Science
United Way of Northern Nevada and the Sierra
Washoe County Public Health Department Washoe County School District
The school is also home to the Nevada Center for Health Statistics and Informatics and
Biostatics which has formal agreements for community-based research with the State of Nevada
Health Division.
In addition to community-based work, the school is also heavily involved in interdisciplinary work with colleagues at the Division of Health Sciences (including medicine, nursing, nutrition, social work, and the Center for the Application of Substance Abuse Technologies) and with colleagues at other units within the university (e.g., social psychology, environmental sciences,
Center for Research Design & Analysis).
Final Self Study, October 2010 Page 88
UNR School of Community Health Sciences
Table 3.1.c. lists examples of community-based research and to highlight some recent examples:
One faculty member (Devereux/social/behavioral health) is working with the School of
Medicine, the Nevada Cancer Institute, and the Nevada Colon Cancer Partnership to evaluate a colon cancer screening program and beginning fall 2010, with the Nevada Hispanic Services to identify barriers to colon cancer screening and to map assets within their community with which to address the barriers. Both studies are community engagement projects in which all phases of the research have been designed in partnership with the community, training in conducting research is provided to the community, and dissemination of results focuses first on community outlets.
Julie Smith-Gagen (epidemiology) is collaborating with the Washoe Tribal Health Center
(WTHC), Great Basin Primary Care, Alpine County California Health Department and Mono
County California Health Department to provide justification and data to support funding for the
WTHC to become a Federally Qualified Health Department. The tribe decided to extend services to non-native community members upon seeing a need within the community. To formally document this need, the team assessed the health, health behaviors, and utilization of care of Tribal members currently using the WTHC, as well as non-Natives currently using the
WTHC and the general population of Douglas, Alpine and Mono County to identify unmet needs in the community. A second project of Dr. Smith-Gagen is a collaboration with the Washoe
Tribal Healing Center to assess the mental health, health behaviors and historical trauma in the community in order to develop culturally sensitive mental health interventions for the Native
Community. The team developed a culturally sensitive survey instrument by meeting with community members, employees and administrators of the Washoe Tribal health Center as well as clinicians and social workers with Native experience. In addition, tribal community members were trained to collect the data.
As a final example, another faculty member (Constantino, social/behavioral health) is working with the Washoe County District Health Department as part of an ACHIVE (Action
Communities for Health, Innovation and EnVironmental change) community. The purpose of an
ACHIEVE community is to create sustainable environmental and/or policy change to improve the health of the community. The faculty works with a coalition of stakeholders within the community to support the changes identified.
3.1.c. A list of current research activity of all primary and secondary faculty identified in
4.1.a and 4.1.b., including amount and source of funds, for each of the last three years. This data must be presented in table format and include at least the following: a) principal investigator, b) project name, c) period of funding, d) source of funding, e) amount of total award, f) amount of current year’s award, g) whether research is community based, and h) whether research provides for student involvement.
Final Self Study, October 2010 Page 89
UNR School of Community Health Sciences
Table 3.1.c. Research Activity of Primary and Secondary Faculty from fall 2007 to spring 2010.
Project Name Principal Funding Source Funding Period Amount Amount
Investigator &
Department
Start/End Total
Award
Current
Year
2007-2008
Community
Based
Y/N
Student
Participation
Y/N
Cancer Registry
Analysis
Childhood
Asthma Prev
Analysis
Women’s Health
Analysis
Cohort
Analysis/Cancer
Studies
Chrysotile: New
Exposure
BRFSS: Diabetes
Crosstab
Effect of NV
Clean Indoor Air
Nevada WIC
Analysis
Autism Database
Analysis
Evaluation of
DETR Rehab
Services
Exercise
Prescription
Yang EPI
Yang EPI
DHHS-CDC/NV-
DHHS-HD
DHHS-HRSA-
NSHE-UNLV
1/2007-2/2007
1/2007-7/2008
$21,216
$32,569
Y
Y
Yang EPI DHHS-CDC/NV-
DHHS-HD
Loomis EPI DHHS-
NIH/UNIV OF N.
CAROLINA
2/2007-6/2008 $46,000.00
1/2007-12/2008 $43,800.00
Y
Loomis EPI DHHS-
CDC/UNIV OF
Yang EPI
N. CAROLINA
DHHS-CDC/NV-
DHHS-HD
1/2007-9/2008
1/2008-3/2008
$36,652.00
$ 15,012.00
NV-DHHS-HD 7/2007-6/2009 $165,047 Elliott,
Loomis (Co-
PI) EPI
Yang EPI
$83,524.00
Yang EPI
DOA-FNS/NV-
HD
8/2007-9/2008 $53,920.00
NV-DHHS-ODS 7/2007-12/2008 $48,153.00
Y
Y
Y
Yang (Co-PI)
EPI
Angermann
EPI
NV-DOETR-RD
NV-DHSS-HD
1/2007-12/2008 $31,546
7/2007 – 6/2009 $220,812 $109,826.0
Y
Y
Y
Y
Y
Final Self Study, October 2010 Page 90
UNR School of Community Health Sciences
Project Name Principal
Investigator &
Department
Funding Source Funding Period
Start/End
Study-YR 2
Gender
Differences in
Health
Community
Health
Nurse/EPSDT
Physician
Train/EPSDT
Billing
Parent Usage of
EPSDT:
Outreach
BRFSS Diabetes
Module Analysis
M. Elliott,
Yang (Co-PI)
EPI
Yang, Smith-
Gagan (Co-
PI) EPI
Yang, Smith-
Gagan (Co-
PI) EPI
Yang, Smith-
Gagan (Co-
PI) EPI
Yang EPI
NSF
DHHS-ACF/NV-
DHHS
DHHS-ACF/NV-
DHHS
DHHS-ACF/NV-
DHHS
DHHS-CDC/NV-
DHHS-HD
7/2008-6/2009
7/2008-6/2009
7/2008-6/2009
7/2008-6/2009
7/2008-1/2009
Amount
Total
Award
$187,344
$81,000
$61,650
$201,150
$11,718
2008-2009
ENV Arsenic &
Diabetes Melitus
Chrysotile &
Lung Cancer Yr
1
BRFSS/Native
Amer Over
Sample
BRFSS/Core
Analysis &
Report
Evaluation of
Loomis EPI DHHS-NIH-
UNIV.OF N.
CAROLINA
DHHS-CDC Loomis,
Hsieh (Co-PI)
EPI
Yang (Co-PI)
EPI
DHHS-CDC/NV-
DHHS-HD
Yang EPI
Yang EPI
DHHS-CDC/NV-
DHHS-HD
NV-DOETR-RD
8/2008-5/2010
8/2008-5/2010
10/2008-8/2009 $64,000
5/2008-3/2009
$39,731
$710,641
$42,500
1/2009-12/2009 $5,987
Final Self Study, October 2010 Page 91
Amount
Current
Year
$81,523
Community
Based
Y/N
Student
Participation
Y/N
Y
Y
Y
Y
Y
Y
Y
Y
Y
Y
Y
Y
UNR School of Community Health Sciences
Project Name Principal
Investigator &
Department
Funding Source Funding Period
Start/End
Amount
Total
Award
DETR Rehab
Services
Community
Health
Nurse/EPSDT
Physician
Train/EPSDT
Billing
Parent Usage of
EPSDT:
Outreach
Hyperoxia &
Oxidative Stress
Assessing the
HIV Prevention
Needs of Men
Who Have Sex
With men in
Nevada: A
Strategic
Planning
Proposal
Yang, Smith-
Gagan (Co-
PI) EPI
Yang, Smith-
Gagan (Co-
PI) EPI
Yang, Smith-
Gagan (Co-
PI) EPI
Angermann
EPI
Clements-
Nolle (Co-PI)
EPI
DHHS-ACF/NV-
DHHS
DHHS-ACF/NV-
DHHS
DHHS-ACF/NV-
DHHS
OHIO
UNIVERSITY
CDC
Supplemental
Grant PS04-012 through the
Nevada State
Health Division
7/2009-6/2010
7/2009-6/2010
7/2009-6/2010
$72,495
$55,177
$180,029
5/2009 – 6/2010 $30,453
2008-2009 $52,846
Amount
Current
Year
Y
Community
Based
Y/N
Student
Participation
Y/N
Y
Y
Y
Y
Y
Y
Y
Final Self Study, October 2010 Page 92
UNR School of Community Health Sciences
Project Name Principal
Investigator &
Department
Funding Source Funding Period
Start/End
2009-2010
Amount
Total
Award
Diabetes
Prevention &
Control
Family to Family
Eval
Family Resource
Center Eval
Christiansen
SBH
Anstee SBH
Christiansen
SBH
DHHS-CDC/NV-
DHHS-HD
DHHS-
HRSA/Family
Ties of NV
Washoe County
School District
Higher
Education
Service Learning
Evaluation
Nevada
Conservation
Corps
Americorps and
Volunteer
Program
Evaluation
Christiansen
SBH
Christiansen
SBH
Nevada
Volunteers
Great Basin
Institute
PIRC Evaluation Christiansen
SBH
PIRC Evaluation Christiansen
SBH
WCDS APMR
Technical
Assistant
Washoe County
School District
Christiansen
SBH
Anstee SBH
Washoe County
School District
Washoe County
School District
Washoe County
School District
Washoe County
School District
05/2009-
03/2010
08/2009-
05/2010
07/2009-
09/2011
10/2009-
06/2010
07/2010-
09/2010
08/2009-
09/2009
$23,000
$5,000
07/2009-
06/2010
$6,700
7/2009-9/2010 $23,000
$30,000
$30,000
$10,000
$3,250
10/09-6/2010 $49,000
Final Self Study, October 2010 Page 93
Amount
Current
Year
$17,500
Community
Based
Y/N
Student
Participation
Y/N
UNR School of Community Health Sciences
Project Name Principal
Investigator &
Department
Funding Source Funding Period
Start/End
Amount
Total
Award
Title II
Evaluation
Technical
Assistance
Diabetes
Prevention &
Control
Gender
Differences in
Health
Tribal
Management
Grant/Type 2
Diabetes
Washoe Tribal
Health Center
Latino Cancer
Survivors
Christiansen
SBH
Elliott, Yang
(Co-PI) EPI
Smith-Gagan,
Yang (Co-PI)
EPI
DHHS-CDC/NV-
DHHS-HD
NSF
DHHS-HIS-
WASHOE
TRIBE NV & CA
05/2009-
03/2010
8/2009-8/2011
$23,000
$105,821
12/2009-6/2010 $18,390
Smith-Gagan
EPI
Smith-Gagan
EPI
Devereux
(Co-PI) SBH
DHHS-
HRSA/WASHOE
TRIBE NV&CA
UNIV OF CA,
LOS ANGELES
NIH/NCRR
11/2009-
3/1/2010
1/2010 –
11/2010
$13,000
$20,000
9/2009-8/2011 $680,000 Colon Cancer
Screening
Program
Navigator
Evaluation
Algal-Based
Renewable
Energy
Angermann
EPI
DOE-NSHE-DRI 11/2009 –
10/2010
$100,000
Amount
Current
Year
Y
Y
Y
Y
$340,000 Y
Community
Based
Y/N
Student
Participation
Y/N
Y
Y
Y
Y
Final Self Study, October 2010 Page 94
UNR School of Community Health Sciences
3.1.d. Identification of measures by which the program may evaluate the success of its research activities, along with data regarding the program’s performance against those measures for each of the last three years. For example, programs may track dollar amounts of research funding, significance of findings (eg, citation references), extent of research translation (eg, adoption by policy or statute), dissemination (eg, publications in peerreviewed publications, presentations at professional meetings), and other indicators.
The Program has established specific goals and objectives (Table 3.1.d) by which research success is measured. The four objectives assessing peer-reviewed publication, conference presentations, grant submissions, and grant awards are tracked annually using data submitted by the faculty via the Digital Measures database described previously. Data on the amount of grant awards are supplemented by information from the University Office of Sponsored Projects.
The objectives pertaining to publication and growth in research awards have been met in advance of the December 2011 target date. The two objectives related to conference presentations and the number of faculty submitting grant proposals have not yet been achieved, but it appears likely that they will be by the end of 2011.
Table 3.1.d. Measures by which the program evaluates the success of its research activities with data for the last 3 years.
2) Goal: “To develop the knowledge base for public health through research.”
2007 to 2008
Data
2008 to 2009
Data
2009 to 2010
Data
75% 71% 63%
Objectives:
1.
At least 60% of faculty will publish an article in a peer-reviewed journal by 2011.
2.
At least 70% of faculty will present research results at a conference by
2011.
88% 71% 59%
3.
At least 70% of faculty will submit one proposal for grant funding by
2011.
4.
Number of new external fund awards and amount of awards per
FTE will increase 5% by 2011.
69%
31%
$187,299 per faculty FTE
>5% increase
71%
43%
$92,312 per faculty FTE
75%
44%
$84,671 per faculty FTE
2006-2007 Baseline:
3 faculty received grants
Total amount = $261,090
$18,649 amount/faculty FTE
Other measures of research success are evaluated annually for individual faculty members, as described above. The indicators considered in annual evaluations of research activity are directed primarily toward scholarly publication and grant support. For publication, the number and types of scholarly publications, the faculty member’s role as an author, and, for journal
Final Self Study, October 2010 Page 95
UNR School of Community Health Sciences articles, the journals in which they appear are considered. Some faculty members contribute to public health reports or other professional documents, and these are also considered in performance evaluations. The impact of publications is difficult to assess in the short-term, but narrative evidence of impact, such as influence in science or policy-making is considered when available. Highly-cited papers and particularly influential ones are noted in evaluations for promotion and tenure where the longer time span facilitates evaluating the impact of publications.
Grant support is also considered in faculty evaluations. All faculty members are encouraged to pursue external research support, while recognizing that there is considerable variation among disciplines in the need for research support and the amounts likely to be obtained. The magnitude of grant awards is considered to be less important than success in securing the funds needed to support a high-quality research program.
3.1.e. A description of student involvement in research.
Student involvement in developing new public health knowledge is a priority of the Program.
The opportunity to be involved in research and scholarly publication is an important component of graduate training, allowing students to practice skills they learn in the classroom.
The faculty provide many opportunities for students for scholarly work, through both independent work and in a faculty partnership mentoring capacity. Research training of graduate students is accomplished by performing well in graduate courses, the mentoring relationship with a faculty member, acting as a research assistant of a faculty member. Master’s professional projects may also involve research.
Many MPH students gain research experience through formal research assistantships. Graduate research assistants are involved in all phases of research and carry out a wide variety of activities, such as:
Collecting data by administering surveys, interviews, or running research protocols
Coding and entering data into a
Using computer skills such as word processing, spreadsheet, scheduling and statistical analysis software
Participating in preparation of
spreadsheet or statistical analysis program
Conducting literature reviews and document research
Developing and proposing new research ideas and IRB applications
Participating in the methodological development of a research project, including study designs, modeling
submissions for local or regional conferences and, if accepted, working on poster or oral presentations for professional conferences
Participating in preparing a manuscript to submit the results of your collaborative research to a scientific journal and statistical inference.
Mentorship and research assistantships also allow the student to work one-on-one with a faculty member, enabling the student to gain skills and knowledge that aren't easily learned in the classroom, such as research attitude and generation of research ideas.
Final Self Study, October 2010 Page 96
UNR School of Community Health Sciences
3.1.f. Assessment of the extent to which this criterion is met.
This criterion is met.
Strengths
Program faculty and students are active in contributing to the knowledge base of public
health.
Program research activity enhances the training of the public health students.
Public health research from the SCHS has been regularly published in peer-reviewed scientific journals.
Research projects by faculty and students have been awarded extramural funding.
SCHS research projects have often included community partners.
MPH students have been honored for their research work, both within the university and professional organizations.
Suggested Improvements
The program should identify strategies for involving more faculty in extramurally funded research activities. Such research support would provide excellent training opportunities for students, would enhance recognition of the school, and would shore up resources during a period of potentially wavering state funds.
Faculty should continue to seek external funding and publish their research.
Final Self Study, October 2010 Page 97
UNR School of Community Health Sciences
3.2 Service. The program shall pursue active service activities, consistent with its mission, through with faculty and students contribute to the advancement of public health practice.
3.2.a.Description of the program’s service activities, including policies, procedures and practices that support service. If the program has formal contract or agreements with external agencies, these should be noted.
As a land grant university, UNR maintains a commitment to community and public service programs through dissemination of knowledge to the community, collaboration with the public and private sectors, and provision of assistance to state and local governments. The UNR
Division of Health Sciences (DHS) mission statement also illustrates a commitment to service;
“[DHS] is tied together by the need to find solutions for and help people towards improving their health and well-being through education, research, clinical care and public service” (DHS draft bylaws).
The mission of the School of Community Health Sciences, “to develop, disseminate, and apply knowledge with an ecological approach to protect and promote the health of populations statewide and worldwide,” highlights a commitment to service, and one of our five core values is
Community and Collaboration. Goals adopted by SCHS demonstrate our commitment to engaging in professional and scholarly service and contributing to positive changes in the health of Nevadans. Our mission, vision and goals are satisfied through numerous activities and commitments of the CHS faculty and are supported through the university’s and school’s encouragement and expectations of both faculty and student involvement in service activities.
Personnel policies. Faculty of the University of Nevada, Reno are evaluated annually on teaching, research and service activities. The university by-laws state that “an academic faculty member being recommended for appointment with tenure must receive a "satisfactory" rating or better in the area of service, which may include, but not be limited to [italics added to community service elements]:
(A) Membership and participation in professional organizations;
(B) Ability to work with faculty and students in the best interests of the academic community and the people it serves , and to the extent that the job performance of the academic faculty member's major unit may not be otherwise adversely affected;
(C) Service on university or system committees;
(D) Recognition among colleagues for possessing integrity and the capacity for further significant intellectual and professional achievement; and
(E) Recognition and respect outside the System community for participation and service in community, state, or nationwide activity.
At the DHS level, the expectation for faculty members to participate in service includes
“community, professional, unit, division, and university service” (draft DHS bylaws) All SCHS faculty have service obligations that are outlined in annual role statements upon which they are evaluated. Although service activities for SCHS faculty generally include membership and chair positions on SCHS, Division of Health Sciences and university committees, faculty are also expected and encouraged to engage in both scholarly and community service outside the university. The SCHS personnel committee is in the process of drafting new annual evaluation guidelines that provide more specific language regarding the expectation of external service
Final Self Study, October 2010 Page 98
UNR School of Community Health Sciences
(including both scholarly and community service) for all tenured professors, tenure-track professors who have completed at least two years toward tenure, and lecturers.
Structural service promotion. The graduate curriculum requires that all students complete a six credit (270 hour) internship, which includes a service-learning component. Examples of past student internship projects are identified in section 3.2.d. below. In 2009 SCHS hired a 25% FTE internship coordinator to oversee student internships and ensure that internship placements fulfill the service learning requirement and other requirements. The student internship is discussed in more detail in section 2.4. Students are also engaged in service through the Public Health Club, an active student organization, and through voluntary participation in faculty-led service activities. The school’s commitment to student involvement in service is also demonstrated by the 3-credit field studies course that is required of all students receiving a Bachelor of Science degree in Community Health Sciences. MPH students are kept informed of community events and opportunities for service through a bulletin board and a WebCampus webpage that allows for mass email distribution. An undergraduate field study project has provided a thorough listing of all opportunities for employment, internships and service in the Northern Nevada area and is published on FaceBook.
As of July 2010 SCHS houses two centers that have ongoing partnerships with community organizations and agencies. The Center for Program Evaluation and the Center for Health
Statistics & Informatics are primarily involved in research, but their links to the community provide us with capacity to develop additional service-related collaborations.
3.2.b. A list of the program’s current service activities, including identification of the community groups and nature of the activity, over the last three years.
CHS faculty has both volunteered been invited to serve on local, regional and international committees. Committee membership of CHS faculty includes: the Regional Transportation
Commission Bicycle Pedestrian Advisory Committee, Nevada Multicultural End-of-Life Care
Coalition, The Indian Health Board of Nevada Youth Suicide Prevention Steering Committee,
Autism Coalition of Nevada, Biophysical Society, National Toxicology Program, Elder Count
Nevada Advisory Committee, North America Public Health Forum, International Institute of
Anticancer Research (IIAR), and the International Society for Environmental Epidemiology.
In addition to committee membership, CHS faculty have served in leadership positions for a variety of organizations such as the Nevada State Maternal and Child Health Needs Assessment
Steering Committee, Nevada Behavior Risk Factor Surveillance System Advisory Committee;
Nevada AIDS Foundation Advisory Board; Rocky Mountain Psychological Association; North
American Public Health Forum; Scientific Committee on Epidemiology of the International
Commission on Occupational Health; American Public Health Association: Ethics Forum;
Nevada Public Health Association; the Nevada POLST Initiative, a statewide effort to improve the transfer of patients between health care facilities; the epidemiologist position for the
Northern Nevada HIV Prevention Planning Council and membership on the Nevada Substance
Abuse Epidemiology Workgroup.
Final Self Study, October 2010 Page 99
UNR School of Community Health Sciences
With tight budgets creating an historical challenge for public entities, collaborations are critical to the full development of many programs and projects. MPH faculty have developed relationships and collaborations with the Washoe County School District, the state’s second largest school district, to provide content for continuing education credit for physical education;
Washoe County Health District supporting the Childhood Obesity Forum; health literacy programming for the Nevada Geriatric Education Center, providing geriatric curriculum for the
Veteran’s Affairs system.
Communities are often best reached in large numbers through the media. The growth, ubiquity and diversity of multimedia provide an opportunity to serve and engage the community at its convenience and in a manner best suited to the individual. The messages of public health can now be disseminated in a diverse array of formats. CHS faculty media interviews, for example, may be accessed later online, sent to others as links, transcribed and emailed or broadcast as
MP3, streaming audio or imbedded on websites. CHS is pleased that its public health interviews have been captured by KUNR radio (Nevada Secretary of State’s Living Will Lockbox project -
Hardwick, HIV in Prisons and Jails - Clements-Nolle, a gastroschisis study - Elliott) and ABC
News, 13 Las Vegas (Triage in Pandemics - Klugman) and may continually engage new audiences.
Although the message of public health may now be disseminated in a variety of ways, the message must be continually updated, verified and evaluated. As with any profession, it is left to the professionals in that field to assure standards of excellence. Therefore, it is important that academic public health professionals participate in the review and evaluation of public health publications, grants and programs. To that end, CHS faculty have provided review and evaluation for numerous journals such as Occupational and Environmental Medicine and the
American Journal of Public Health and to organizations such as the American Society of
Bioethics and the Humanities; University of Texas Health Science Center; Ministry of
Development, General Secretariat for Research and Technology, Greece. Current and recent faculty grants with a service component are provided in Table 3.2.b.
Final Self Study, October 2010 Page 100
UNR School of Community Health Sciences
Table 3.2.b. Extramural Grants/Contracts with Service Component for Each of the Last 3 Years.
Project Name Principal Investigator & Funding Source Funding Community Group
Department Period
Start/End
Loomis (PI) EPI ASIS International 2007-2008 ASIS International Preventing Gun Violence
In The Workplace
Community Health
Nurse/EPSDT
Yang, Smith-Gagan
(Co-PI) EPI
DHHS-ACF/NV-DHHS 2008-2009 Nevada State Health Division;
Nevada Division of Health
Care Financing and Policy
Physician Train/ EPSDT
Billing
Yang, Smith-Gagan
(Co-PI) EPI
DHHS-ACF/NV-DHHS 2008-2009 Nevada Medical Association;
Nevada State Health Division;
Nevada Division of Health
Care Financing and Policy
Parent Usage Of EPSDT:
Outreach
Yang, Smith-Gagan
(Co-PI) EPI
Community Health Nurse/
EPSDT
Physician Train/ EPSDT
Billing
Parent Usage Of EPSDT:
Outreach
Assessing The HIV
Prevention Needs Of Men
Who Have Sex With Men
In Nevada: A Strategic
Planning Proposal
Yang, Smith-Gagan
(Co-PI) EPI
Yang, Smith-Gagan
(Co-PI) EPI
Yang, Smith-Gagan
(Co-PI) EPI
Clements-Nolle
(Co-PI) EPI
DHHS-ACF/NV-DHHS 2008-2009 Nevada State Health Division;
Nevada Division of Health
Care Financing and Policy
DHHS-ACF/NV-DHHS 2009-2010 Nevada State Health Division;
Nevada Division of Health
Care Financing and Policy
DHHS-ACF/NV-DHHS 2009-2010 Nevada Medical Association;
Nevada State Health Division;
Nevada Division of Health
Care Financing and Policy
DHHS-ACF/NV-DHHS 2009-2010 Nevada State Health Division;
Nevada Division of Health
Care Financing and Policy
CDC Supplemental Grant
PS04-012 through the
Nevada State Health
Division
2008-2009 Northern Nevada
HIV/AIDS/STD Planning
Council
Final Self Study, October 2010 Page 101
UNR School of Community Health Sciences
Project Name Principal Investigator &
Department
Funding Source
Colon Cancer Screening
Program Navigator
Evaluation
Tribal Management
Grant/Type 2 Diabetes
Washoe Tribal Health
Center
West Region
Epidemiologist
Devereux (Co-PI) SBH
Smith-Gagan, Yang
(Co-PI) EPI
Smith-Gagan EPI
NIH/NCRR
DHHS-HIS-WASHOE
TRIBE NV & CA
DHHS-HRSA/WASHOE
TRIBE NV&CA
Assessing Pre-Schoolers
Motor Skills
Project Play
Leadership Coach For
Community Health Action
Response Team (CHART)
Clements-Nolle EPI
(epidemiologist on project);
Center for the Application of Substance Abuse
Technologies (grant PI)
Constantino SBH (trainer);
Southern Area Cooperative
Extension (grant PI)
Constantino SBH
SAMSHA/CSAP
USDA/NIFA/AFRI
Constantino SBH (coach);
Washoe County District
Health Department (grant
PI)
Unfunded project to engage elementary-school youth in physical activity at a community school
NACCHO/CDC
ACHIEVE (Active
Communities for Health,
Innovation, and
EnVironmental ChangE)
Funding
Period
Community Group
Start/End
2009-2011 Nevada Cancer Institute;
12/2009-
6/2010
Nevada Colon Cancer
Partnership
Washoe Tribe of Nevada and
California
11/2009-
3/1/2010
Washoe Tribe of Nevada and
California
2009-2014 State leaders and community prevention practitioners in 11 states, six pacific jurisdictions, and six tribes (The West
Region).
2009-2013 Cooperative Extension –
Southern Nevada area
2009-
2010 -
Jessie Beck Elementary School
Washoe County District Health
Department
Final Self Study, October 2010 Page 102
UNR School of Community Health Sciences
3.2.c. Identification of measures by which the program evaluates success of its service efforts, along with data regarding the program’s performance against those measures for each of the last three years.
Table 3.2.c. Service-related goals and objectives, and data on performance from 2007-2010.
4) Goal: “To engage with multiple communities through professional and scholarly service.”
Objectives:
1.
By 2011, 40% of faculty will co-author reports and publications with colleagues at other units on campus.
2.
By 2011, 30% of faculty will co-author reports, publications, and presentations with community members.
3.
By 2011, 15% of faculty will provide workshops, trainings and continuing education opportunities to public health professionals.
4.
By 2011, 15% of faculty will provide technical assistance to the community, including but not limited to, program evaluations, consulting, data analysis, grant partnerships.
5.
By 2011, 10% of UNR faculty is members of community boards or committees.
6.
By 2011, 10% of UNR SCHS committees will include a community member.
Data Source 2007 to 2008
Data
Digital Measures 56%
Digital Measures and Staff Survey
Digital Measures
Digital Measures
Digital Measures
Program Director
25%
17%
22%
56%
N/A
2008 to 2009
Data
21%
36%
19%
25%
63%
N/A
2009 to 2010
Data
31%
35%
32%
26%
47%
17%
Final Self Study, October 2010 Page 103
UNR School of Community Health Sciences
3.2.d. A description of student involvement in service.
Although many students entering the MPH program already have a strong history of service, the
MPH curriculum, the Public Health Club, internships and research all encourage and support student service. Including service as a component of the MPH curriculum provides students with exposure to the variety of opportunities available to them. However, it is also critical that students pursue such service on their own, recognizing the value that service brings to the community and themselves. SCHS MPH students have demonstrated their independent commitment to service through numerous community activities. They have been involved in
Global Voice Volunteering, a Virginia City, NV program to provide volunteers to a variety of community projects; offered sports injury prevention programs to local high schools; served on the advisory board of the Reno Housing Authority, served as Secretary for Sierra Nevada
Journeys, a non-profit organization providing experiential education to the local school district; and have been involved with the WIC mobile dental van.
Several courses currently incorporate service activity into the curriculum. Dr. Clements-Nolle has provided a variety of service experience to her students in her classes CHS 476/676: HIV-
Psychosocial and Health. Students have been involved in HIV testing and outreach, the Larry
Bryant Event Fashion Show Benefit, AIDS Memorial, the National Women and Girls HIV/AIDS
Day and World AIDS day (using red ribbons to raise awareness for HIV/AIDS on campus in
2008). In 2009 students from this course developed a chapter of Hope for Hoops, raising $4000 for AIDS orphans in Africa, raising the second largest amount of 50 such events. Other courses apply course work to service, such as Ms. Fitch’s CHS 720: Program Planning and Grant
Writing in which students develop program plans for community organizations and agencies. As an aspect of their courses, students have also hosted a smoking cessation event (CHS 695), provided data analysis (CHS 725, CHS 753) and evaluated community agencies and federally funded grant projects (CHS 720, CHS 721).
The Public Health Club established by our MPH students has also provided opportunities for a variety of community activities. The club has sponsored food drives, a triathlon, and annual events associated with Public Health Week and World AIDS Day.
Internships serve a variety of purposes, one of which may be including service. Prior to our current internship and capstone curriculum, students had the option of developing projects. Many of these involved service and represent the vastness of the scope of public health, for example:
Weapons of mass destruction preparedness training presented to Northern Nevada physicians and nurses, implementation of a school-wellness program, development of a fund for dental care for homeless high school students, assessment of Planned Parenthood Mar Monte’s Teen Talk program, development of a community health report card and analysis of participants in the
Tahoe Adaptive Ski School. Such a variety of experiences expose students to areas of public health they may not have otherwise explored or considered.
Many MPH students have had an opportunity to engage in research and publish with a faculty mentor. Some of these efforts involve community service. Examples include: medication therapy management program for seniors, nutrition in the garden at a local elementary school, conducting a needs assessment at a community-based organization for people living with
HIV/AIDS, and providing a training session about working with older adults for community
Final Self Study, October 2010 Page 104
UNR School of Community Health Sciences health workers.
3.2.e. Assessment of the extent to which this criterion is met
Strengths
The faculty demonsrates extensive involvement in service activities.
Opportunities and expectations for service are incorporated in the SCHS curriculum.
Technology and new procedures have improved communication and dissemination of student service opportunities, e.g. through the Webcampus system.
Suggested Improvements
The program needs improved tracking of student and faculty professional and community service activities. One suggestion is to ensure faculty highlight these activities in their yearly evaluations. Utilizing the Center for Program Evaluation to assist in the evaluation and tracking of program objective’s should help greatly.
The program should increase the time and expand the role of the internship coordinator to allow for creation and maintenance of a formal mechanism for coordinating and monitoring student service opportunities.
The school could modify faculty annual evaluation guidelines to include more specific directions on requirement for service to the community and distinguish it from universityrelated service. The personnel committee will review this for the 2010 evaluation cycle.
The program could encourage more presentations and publications based on service activities. Having these activities more formally recognized in faculty evaluations will be a major source of encouragement and subsequent professional faculty community service.
Final Self Study, October 2010 Page 105
UNR School of Community Health Sciences
3.3 Workforce Development. The program shall engage in activities that support the professional development of the public health workforce.
As the state’s historic land-grant institution, the University of Nevada, Reno has an explicit mission to disseminate education, consultation, and research across the state.
3.3a. A description of the program’s continuing education activities, including policies, needs assessment, procedures, practices, and evaluation that support continuing education and workforce development strategies.
Policies and Institutional Support.
SCHS Level
The school’s mission statement includes five goals, with the fourth goal being “to engage with multiple communities through professional and scholarly service.” This goal includes engaging the public health workforce in training and development activities. Objective 3.3 provides a measurable outcome of workshops, training, and continuing education activities.
The self-study committee devised and began to execute a plan to support workforce development. Improvements in formal support included raising awareness among the faculty of the importance of engaging in workforce development and potentially offering additional incentives and rewards for the activity. The topic was brought to the faculty steering committee and specific development activities will be discussed at a faculty bi-annual retreat.
University Level
Workforce development for the State of Nevada is a core mission of this university. UNR offers a vigorous extended studies program; the involvement of SCHS is outlined below. The
University of Nevada School of Medicine, also part of the Division of Health Sciences, administers a state-wide program that offers an extensive, state-of-the-art infrastructure for teleconferencing and CME/CEU seminars. The university also offers various settings for workforce development activity including lecture series. Below in section 3.3d specific participation in these are listed.
Associate Dean for Workforce Development
The UNR Division of Health Sciences, which houses the MPH program, hired an associate dean in 2005 to lead workforce development initiatives. The Associate Dean for Workforce
Development served the units of the division, with primary emphasis on public health. The position was funded through a grant from the State of Nevada Health Division. The associate dean’s mandate was “to promote public health workforce recruitment, retention and improvement throughout the university and the professions utilized in public health and social services agencies.”
The projects and activities undertaken by the associate dean included:
In March 2007, created and proposed a plan to develop a series of professional development programs and certificate program for state public health workers to be offered by the SCHS. The proposal was presented; a preliminary needs assessment was conducted; and an action plan for
Final Self Study, October 2010 Page 106
UNR School of Community Health Sciences implementation was developed. Although the State did not follow through with implementation due to severe budget crisis in state and lack of funding for employee development activities, the findings are still valid and will be pursued when funds become available.
Facilitated and convened a statewide workforce development task force for the Department of
Health and Human Services for the State of Nevada, as per the request of its Director (spring
2007). This resulted in a joint meeting of all state agency directors and university administrators from both UNR and UNLV. A survey of needs and action plans were created for joint collaborations.
As directed by the administrator of the State of Nevada Health Division, the associate dean was asked to conduct a strategic communication needs analysis and facilitate a forum with all stakeholders in the state, including local health district personnel and state officials, to formulate strategic relationship building plan and strategies in spring 2008.
Served as a consultant and facilitator for an organizational development intervention to strengthen personnel and develop leadership competencies for staff and administrators in the
Nevada Early Intervention Services unit of the Division of Health (June 2008).
State and Regional Level
The state capital and many state health agencies are located in Carson City, about 30 miles away from the UNR campus. In addition, Reno traditionally serves as a central hub for many of the rural sections of the state. This provides the potential for the MPH program to become a convenient training center for the public health workforce. We have many connections with the state government and have placed many MPH graduates in positions there. However, no formal training programs are established and much more can be done to serve workforce development imperatives. Other state and regional support systems include the Great Basin Public Health
Leadership Institute, explained below in 3.3d.
National Level
The new public health exam and other new credentials requirements may create a new demand in the state for workforce development training. The movement towards credentialing will raise the priority of workforce development activity and should promote demand for training from the
MPH program. For example, the need for training will potentially strengthen linkages with the
State Health Division.
Needs Assessment. The program has examined and utilized the results of needs assessments provided by the University Division of Health Sciences and by the state government and others in the state (see below).
2006 Survey Results
The Nevada State Health Division published the results of a survey of the public health workforce in 2006. Data were collected in 2005 by the Nevada State Health Division in collaboration with the UNLV’s School of Community Health Sciences. The survey found that
99% of the workforce was interested in additional training on various topics and in various settings. Ninety-three percent (93%) sought additional training for job knowledge and skills,
Final Self Study, October 2010 Page 107
UNR School of Community Health Sciences while 79% said it was required for their current positions. On-site training was most preferred
(46%); off-site workshops were the second preference (24%); and, 21% preferred a certificate program offered by the university.
When asked how likely they were to participate in a certificate program, 33% of workers were very likely; 20% somewhat likely; and, 26% likely, for a total of potential interest among 79% of state public health workers. The most requested certificate topic was health care administration
(43%), followed by public health leadership (38%), and principles of public health (37%).
Forum for Healthy Nevada
In response to this report, a forum with state government officials was convened in January 2007 by the UNR health sciences associate dean for external relations (attached in Appendix L). This was entitled “Forum for Healthy Nevada” and the major goal was workforce development.
Participants included the Director of the UNR School of Community Health Sciences, the
Director of the State Division of Health and Human Services, and many others. Preparing a diverse workforce emerged as a main theme of this meeting, and plans were made for several next steps, including proposals to the legislative session. The state then entered a severe budget crisis, but these efforts have built an institutional foundation with a capacity for further action.
Future Needs Assessment
Plans for future needs assessment were discussed at the fall 2010 faculty retreat. A taskforce was identified and one faculty member and one member from the Division of Health Sciences have agreed to work on this.
Procedures, Practices, and Evaluation: The program collects data on workforce development activity via the electronic annual review system. Pursuant to program goal 3.3, the program will define workforce development activity as offering certificate programs, continuing education, and lectures to the public health workforce. As a goal, the program will expect activity from
15% of faculty members each year. The program will assess workforce development activity with every annual performance evaluation. Language on how to more accurately reflect workforce development activities was provided for the 2009 annual evaluation. The program will re-evaluate its workforce development activity every fall faculty retreat.
3.3.b. A description of certificate programs or other non-degree offerings of the program, including enrollment data for each of the last three years.
Certificate program wholly administered by the MPH program:
Certificate program in Health Care Ethics
The Graduate Certificate in Bioethics provides an opportunity for graduate students and working professionals in the health care fields to gain knowledge and skills in the specialized area of bioethics. The program seeks to teach students the core competencies called for by the American
Society for Bioethics and Humanities. These objectives include (1) ethical assessment skills, (2) process skills, and (3) interpersonal skills. This program provides a specialization that can be productively used to enhance one's current career or to supplement work in another degree.
Courses are offered in evening, weekend, intensive, and web-based formats in addition to
Final Self Study, October 2010 Page 108
UNR School of Community Health Sciences traditional class meetings. Students must have a B (3.0) or better average in each course to earn the certificate and all course work must be completed within 5 years of matriculation. Approved electives can count for both the MPH degree and the health care ethics certificate when relevant for the student’s program of study. In the last five years, one MPH student has obtained the ethics certificate.
Extended studies courses supported by the MPH program:
The University Extended Studies program is a mechanism for continuing professional education.
The office markets courses taught at non-traditional times to the community. Faculty from the
MPH program have offered courses through extended studies. For example, the MPH program planned to offer “Health Care Management, Public Health and Health Policy in Canada” in summer 2010, to be taught by affiliate faculty and listing the school’s course number. The course was to be offered in Toronto, Canada but due to low course enrollment was canceled. It is being planned again for Summer 2011.
Certificate programs affiliated with / partly supported by the MPH program:
Certificate programs in Gerontology:
The Gerontology Academic Program prepares student scholars from a variety of disciplines to provide the highest quality of service to Nevada’s elder population. The Gerontology Certificate
Program has been deemed a Program of Merit by the Association for Gerontology in Higher
Education. UNR administers the 24-credit gerontology certificate program in the Division of
Health Sciences. In addition, an online distance-learning certificate program is administered by several Nevada campuses in partnership. The University of Nevada, Reno and the University of
Nevada, Las Vegas in concert with Nevada State College and the Nevada Geriatric Education
Center offer an online option for their respective certificate programs. Approved electives can count for both the MPH degree and the gerontology certificate when relevant for the student’s program of study. Six MPH students have obtained the gerontology certificate.
3.3.c. A list of the continuing education programs offered by the program, including number of students served, for each of the last three years. Those that are offered in a distance learning format should be identified.
3.3c.1. Summary Table of Students Served in Continuing Education Programs.
Number of
Students
2007-2008
190
2008-2009
40
2009-2010
227
Final Self Study, October 2010 Page 109
UNR School of Community Health Sciences
Table 3.3.c. Students Served in Continuing Education Programs: Detailed Information.
Faculty Organization # of
Participants
Professional or
Academic
Description
Mel
Minarik
Truckee
Meadows
Community
College
45 Professional 8-06 Faculty Development Week--Celebrate What's
Right with the World
8-07 Faculty Development Week--Leadership
Craig
Klugman
Craig
Klugman/D
Freedman
University
Medical Center
Southern Nevada
Renown
75
70
Professional
Professional
"Professional Inoculation" looking at medical professionalism and dealing with the health care crisis in Nevada brought on by Southern Endoscopy crisis.
Critical Reflections on Evidence of Effectiveness and
Ethics in the Management of Tuberculosis."
Mel
Minarik
Nevada Mental
Health Assn.
Dan Cook Stanford
GRECC
Geriatric Core
Curriculum
Series
40
20
Academic
Professional
Current research in spirituality and health.
Medication Therapy Management and Health
Literacy. Palo Alto CA and Reno NV, CEUs
Dan Cook Nevada Geriatric
Education
Center, Faculty
Training Series
Dan Cook Washoe County
Health District
25
100
Professional
Professional
Medication Management, Health Literacy, and Aging.
Reno NV and 6 other locations by interactive video,
CEUs certified
Kristen
Clements-
Nolle
SAMHSA/CSA
P Center for the
Application of
Prevention
25 Academic
Year
2007
2008
2008
2008
2009
2009
"How 'Big Food' Markets to Children," Washoe
County Obesity Forum to statewide audience of public health and other professionals receiving CEU's.
Minority AIDS Initiative Cohort VIII Grantees Joint
Kickoff Meeting: The Strategic Prevention
Framework Needs Assessment and Epidemiology.
CEU’s awarded.
2009
2009
Final Self Study, October 2010 Page 110
UNR School of Community Health Sciences
Faculty Organization # of
Participants
Technologies
(CAPT):
Professional or
Academic
Description
Kristen
Clements-
Nolle
Academic Using Data for Decision Making in the Pacific
Jurisdictions. CEU’s awarded.
Kristen
Clements-
Nolle
SAMHSA/CSA
P Center for the
Application of
Prevention
Technologies
(CAPT):
SAMHSA/CSA
P Center for the
Application of
Prevention
Technologies
(CAPT):
21
36 Academic Epidemiology Technical Assistance Workshop with
SPF SIG Cohort III/IV Tribes
Year
2010
2010
Final Self Study, October 2010 Page 111
UNR School of Community Health Sciences
Other activities open to the public health professional workforce include Lecture Series such as the Division of Health Sciences Grand Rounds, public talks sponsored or co-sponsored by the school. Examples include a talk by a visiting scholar (Alice Eagly) in March 2010 on women and leadership co-sponsored with the PhD program in Social Psychology.
A recent example (September 2010) of a professional development opportunity is a webinar given by an epidemiology faculty on “The Prescription Drug Use Epidemic and
Prevention: How can Prescription Drug Monitoring Programs Help?” with Peter Kreiner, PhD and John Eadie, MPA from the Prescription Drug Monitoring Program Center for Excellence, at
Brandeis University. This presentation reached 37 participants and Continuing Education credits were awarded.
3.3.d. A list of other educational institutions or public health practice organizations, if any, with which the program collaborates to offer continuing education.
Washoe County Health District (e.g. Obesity Forum fall 2009)
Nevada Public Health Association
Northern Nevada Chapter of the Nevada Public Health Association
State of Nevada Health Division:
Although we do not have any formal training programs, we have many formal and informal relationships between the MPH program and the State Health Division. Several UNR MPH graduates now work there. Many of these working relationships involve research and technical support activity, but workforce training activity has been limited. In 2006, an associate dean at the Division of Health Sciences designed and proposed a certificate program in public health management in partnership with the State Health Division. The plan included state support for the participants, and for the training to be embedded in official job descriptions. Unfortunately this plan has not yet been implemented in part due to the recent economic situation of the state.
Nevada Geriatric Education Center:
The Nevada Geriatric Education Center (NGEC) was established in October 1992, joining a nationwide network of similar centers. The NGEC is currently receiving grant funds from the
Health Resources and Services Administration for the Department of Health and Human
Services. The NGEC is committed to improving the health care delivered to older adults by providing education, information and resources to health professionals and faculty. The NGEC administers several ongoing statewide lecture series that offer workforce development education, often with CEUs. Dr. Cook from the faculty has contributed lectures to the health literacy and aging series, for example.
Renown Regional Medical Center
Truckee Meadows Community College
Nevada Mental Health Association
Palo Alto Geriatric Research Education and Clinical Center:
The Reno Veterans Administration hospital participates in the Stanford GRECC, which offers continuing education including a geriatrics lecture series. For example, Dr. Cook from our faculty gave a lecture in 2009.
Final Self Study, October 2010 Page 112
UNR School of Community Health Sciences
Great Basin Public Health Leadership Institute:
Faculty participate in trainings and provide service activities to the Great Basin Public Health
Leadership Institute which is a workforce development nonprofit organization developed in partnership by Nevada and Utah’s public health professionals.
Pacific Public Health Training Center:
Nevada is included in the region served by the federally-funded PPHTC. Examples of utilization of this resource are unknown, but it exists as a potential vehicle for workforce development. In fact, the training modules could support or supplement local plans for trainings.
Northwest Center for Public Health Practice:
Nevada is not included in the region served by this federally-funded project, but Northern
Nevada and rural Nevada may feel a cultural and geographic affinity to the work of this center.
Examples of utilization of this resource are unknown, but it is potentially a resource for workforce development.
3.3.e. An assessment of the extent to which this criterion is met.
The criterion is met, with commentary.
The program has met its internal goals. Workforce development activity occurs, but is not supported systematically with planning. The program has room to expand its workforce development activity and should do so in order to strengthen the program and to improve public health in Nevada.
Strengths:
The committee found that substantial and various workforce training activity occurs through the efforts of faculty with diverse backgrounds and interests. Reporting procedures were recently improved using the electronic annual review system already in place. Additionally, the self-study committee on workforce development implemented an agenda to raise awareness among the faculty and to devise institutional support and other incentives that will encourage workforce training.
Suggested Improvements:
Beyond the explicitly stated goal of the program, the self-study found few structural or system-level supports for workforce development activity. Workforce training has not been systematically organized or specifically supported by formal policies, procedures or planning. The program should consider making this area a priority for enhancement in the planning cycles ahead. For example, the program might bring to fruition a public health continuing education course, possibly in coordination with the state health division, as early steps have already been taken towards this goal.
Enhanced alumni relations to identify the demand for appropriate training activity.
Develop existing or new certificate programs, with online components, that will provide greater outreach to the statewide workforce.
Final Self Study, October 2010 Page 113
UNR School of Community Health Sciences
Workforce development activities might be specifically rewarded or incentivized somehow among the faculty, such as being listed among the criteria for excellence during annual reviews.
Final Self Study, October 2010 Page 114
UNR School of Community Health Sciences
4.0 Faculty, Staff and Students
4.1 Faculty Qualifications. The program shall have a clearly defined faculty which, by virtue of its distribution, multidisciplinary nature, educational preparation, research and teaching competence, and practice experience, is able to fully support the program’s mission, goals and objectives.
4.1.a. A table showing primary faculty who support the degree programs offered by the program. It should present data effective at the beginning of the academic year in which the self-study is submitted to CEPH and should be updated at the beginning of the site visit.
This information must be presented in table format and include at least the following: a) name, b) title/academic rank, c) FTE or % time, d) tenure status or classification*, e) gender, f) race, g) graduate degrees earned, h) discipline in which degrees were earned, i) institutions from which degrees were earned, j) current teaching areas, k) current research interests, and l) current and past public health practice activities. *Note: classification refers to alternative appointment categories that may be used at the institution. See CEPH
Data Template F.
Table 4.1.a lists faculty qualifications for the SCHS. The table includes a couple research assistant professors but all have primary appointments within the school. The school has an appropriate mix of junior and senior faculty and sufficient faculty numbers to support the epidemiology and social/behavioral health emphases.
Faculty come from diverse educational backgrounds and institutional environments in order to provide a breadth of training experiences for students.
Final Self Study, October 2010 Page 115
UNR School of Community Health Sciences
Table 4.1.a. Current Core Faculty Supporting Degree Offerings of Program by Specialty Area.
Kristen
Clements-Nolle
Leslie Elliott
John Hsieh
Associate
Professor
Assistant
Professor
Professor
Tenured
Tenure
Track
Tenured
1.0 F White,
Non-
Hispanic
.98 F White,
Non-
Hispanic
.72 M Asian
MPH
PhD
MPH
PhD
PhD
University of
California at
Berkeley
University of North
Carolina at Chapel
Hill
University of North
Carolina at Chapel
Hill
Social
Behavioral;
Epi.
Occupation al Health
Nursing;
Epi.
Biostats.
Epidemiolgy
HIV/AIDS
Advanced
Epi.; Chronic disease Epi.
Health
Analysis;
Advanced
Biostatistics
HIV/AIDS substance use, suicide, and inter- personal violence
Occupationa l and enviro. health
Life table analysis; multivariable methods; survival analysis
Senior
Epidemi- ologist San
Francisco
Department of Public
Health
Senior
Epidemi- ologist,
Washoe
County
Health
District
Senior Public
Health
Scientist,
Health and
Welfare
Canada
Final Self Study, October 2010 Page 116
UNR School of Community Health Sciences
Mingen Lu
Julie Smith-
Gagen
Assistant
Professor
Tenure
Track
Assistant
Professor
Tenure
Track
1.0 M Asian MS
PhD
PhD
1.0 F White,
Non-
Hispanic
MPH
PhD
Shanghai
Normal
University
Shanghai,
China;
NE
University
Boston;
University of Iowa,
Iowa City
Mathmtics
Mathmtics
Biostatstics
Biostatistics;
Applied
Health
Analysis
University of South
Florida;
University of
California at Davis
Generalist;
Epi.
Cancer Epi.
Panel count data analysis, survival data analysis,
Longitudinal data analysis, multivariate survey method- ology
Methods to determine the distribution and determinants of cancer with viral etiology or co-factor involvement
; disparities
Wei Yang Professor Tenure
Track
1.0 M Asian MD
MS
PhD
Nanjing
Medical
College,
China; U
Nevada,
Reno
Medicine;
Nutrition;
Enviro.
Sciences and Health
Enviro.
Health;
Informatics
Final Self Study, October 2010 Page 117
Enviro. Epi.;
Health informatics;
Behavior risk factors
Occupational
Medicine
Physician;
Clinical Epi.;
State Chief
Biostatcn
UNR School of Community Health Sciences
Judith Sugar
Nora
Constantino
Daniel Cook
Associate
Professor
Associate
Professor
Assistant
Professor
Tenured .52 F White,
Tenure
Track
Non-
Hispanic
Tenured .93 F White,
Non-
Hispanic
.72 M White,
Non-
Hispanic
MA
PhD
MS
PhD
FAC
SM
York
University
Toronto,
Canada
Social and
Behavioral
Health; psychology
Aging
University
Nevada,
Reno;
Univ. of
Southern
California
Physical
Education;
Exercise
Physiology
Social
Behavioral
Health
PhD City
University of New
York,
Graduate
Center
Political
Science
Scientific
Writing,
Health
Policy,
Tobacco
Control
Paul Devereux Associate
Professor
Tenured .93 M White,
Non-
Hispanic
MPH
PhD
San Jose
State
University
University of
Nevada,
Reno
Commnity health education;
Social
Psychology
Social
Behavioral
Health
Michelle
Granner
Assistant
Professor
Tenure
Track
1.0 F White,
Non-
Hispanic
MS
PhD
Florida
State
Univ.;
University of South
Carolina,
Arnold
Nutrition and Food
Sciences;
Health
Promotion,
Education, and
Program
Planning;
Evaluation;
Health
Behavior
Theory
Final Self Study, October 2010 Page 118
Gerontology retirement health literacy
Physical activity across the lifespan
Health and safety regulation and policy
Social isolation, emotion and aging, cancer screening
Promotion of physical activity, nutrition, and weight manage- ment; CBPR
UNR School of Community Health Sciences
Mel Minarik Lecturer Non-
Tenure
Track
1.0 F White,
Non-
Hispanic
MPH
PhD
School of
Public
Health
University of
Nevada,
Reno;
University of
California
Los
Angeles
Behavior
Health
Service
Manage- ment;
Eductnl.
Leadership evaluation
Health Policy and Admin.
Personal leadership,
Health service continuum, org. behavior / devlpmt.; spirituality and health
Hospital admin.;
Medical records administrator
Final Self Study, October 2010 Page 119
UNR School of Community Health Sciences
4.1.b. If the program uses other faculty in its teaching programs (adjunct, part-time, secondary appointments, etc), summary data on their qualifications should be provided in table format and include at least a) name, b) title/academic rank, c) title and current employment, d) FTE or % time allocated to teaching program, e) gender, f) race, g) graduate degrees earned, h) disciplines in which degrees were earned, and i) contributions to the teaching program. See CEPH Data Template G.
Part-time instructors who were hired on a per course basis in the last 3 years are reflected as other faculty in Table 1.6.e. Table 4.1.b.1. shows current other faculty. The school has identified a number of well-qualified public health personnel who support the program, however we do not need to depend on other faculty to support our mission. Adjunct and affiliate faculty who receive salary support from outside the school and who have most typically served on MPH student committees are not listed in Table 1.6.e. This faculty complement brings extensive practical experience to the school by serving as instructors, lecturers, mentors, and collaborators.
The school also has long-standing collaborative relationships for teaching and research with other colleges and schools at UNR and with academic colleagues and practitioners throughout the community and state. Table 4.1.b.2. is a listing of adjunct and affiliate faculty. There are no formal agreements with affiliate faculty. Adjunct faculty are required to sign contracts each year and typically provide support in a specific area (e.g., collaboration on a grant-funded research project).
Final Self Study, October 2010 Page 120
UNR School of Community Health Sciences
Table 4.1.b.1. Current Other Faculty Used to Support Teaching Program (Adjunct, Part-Time, Secondary, etc.).
Department/Specialty
Area
Name Title/Academic
Rank
Title &
Current
Employer
FTE Gender Race or
Ethnicity
Highest
Degree
Earned
Discipline Teaching Areas
Trudy
Larson
Interim Director;
Professor
School of
Medicine;
SCHS
.25 F White,
Non-
Hispanic
MD
Social/Behavioral
Health
Jamie
Anstee
Marie
Boutte
Elizabeth
Christiansen
Peggy
Dupey
Evaluation
Coordinator,
Administrative
Faculty
Associate
Professor
Director; Center for Program
Evaluation
Administrative
Faculty
Associate
Professor
SCHS
SCHS
SCHS
.24 F
.32 F
.15 F
Associate
Dean,
Admissions and Student
Affairs;School of Medicine
.43 F
White,
Non-
Hispanic
White,
Non-
Hispanic
White,
Non-
Hispanic
C
MA,
PhD
MS,
MA,
PhD
PhD
MA
PhD
Pediatrics and
Pediatric
Infectious
Disease
Microbiology,
Pediatric Student
Clinical
Training,
Clinical
Reasoning in
Medicine,
HIV/AIDS
Education
Social
Psychology
Program
Evaluation
Methods
Comm.
Health
Nursing
Anthropology
Medical
Anthropology;
Toxic
Communities
Social
Psychology
Program
Evaluation
Methods
Education and
Sociology;
Counseling and
Educational
Psychology
Cultural
Diversity
Final Self Study, October 2010 Page 121
UNR School of Community Health Sciences
Social/Behavioral
Health
Amy Fitch Lecturer
Epidemiology
SCHS .20 F
Jennifer
Bennett
Internship
Coordinator,
Administrative
Faculty
University of
Nevada
School of
Medicine;
SCHS
SCHS
.25 F
.40 M Jeff
Angermann
Research
Assistant
Professor
White,
Non-
Hispanic
White,
Non-
Hispanic
MPH
MPH
Epi and
Biostatistics
Program
Planning;
Evaluation
Public Health
Leadership
Internship
Course
White,
Non-
Hispanic
PhD Enviro.
Chemistry and
Toxicology
Public health biology; environmental health
Final Self Study, October 2010 Page 122
UNR School of Community Health Sciences
Table 4.1.b.2. UNR School of Community Health Sciences Adjunct & Affiliate Faculty.
Adjunct/Affiliate Faculty at UNR
Economics Wendel Jeanne Ph.D.
Environmental Sciences & Health Miller Glenn Ph.D.
Sanford Center for Aging
Social Psychology
Sacks
Murray
Teresa
Colleen
M.P.H.
Ph.D., F.T.
Medicine
Medicine/Center for Education and Health
Services Outreach
Medicine/Center for Education and Health
Services Outreach
Medicine/Center for Education and Health
Services Outreach
Medicine
Nursing
Nursing
Brown
Ford
Charles
L.D.
Caroline
Patty
Packham John
Jennings
Ruchala
Hubbert
Nursing Running
Benedict
Omaye
Elliott
Stewart
Shadley
M.D., M.P.H.
M.P.H.
Dr.P.H., M.P.H.
Ph.D.
Enid
Patsy
Ann
Alice
Jamie
Stanley
Marta
M.P.H., C.H.E.S.
DNSc, R.N.
Ph.D., R.N.,
C.T.N.
Ph.D., R.N.,
A.P.N.
Ph.D., R.D.
Ph.D.
Ph.D.
Mary White Ph.D.
Meri Ph.D.
Nutrition
Nutrition
Sociology/Social Psychology
Sociology/Social Psychology
Center for the Application for Substance
Abuse Technologies
Nursing
Nevada System of Higher Education
Community Members
Concentra
Washoe County Health District
Washoe County Health District
Program Evaluation Consultant
Washoe County Health District
Program Evaluation Consultant
Nevada State Health Division
Nevada State Health Division
Desert Research Institute
Desert Research Institute
Longo
Trevisan
Khan
Todd
Bernadette Ph.D., R.N.
Maurizio M.D., M.S.
Amy M.D., M.P.H.
Randall
Anderson Mary
Hunsberger Dina
Hadayia Jennifer
McConnell Sara
Whitley Richard
Azzam Ihsan
Zielinska Barbara
Chow Judy
Dr.P.H.
M.D., M.P.H.
Ph.D., M.P.H.
M.P.A.
M.P.A.
M.S.
M.D., M.P.H.
Ph.D.
Ph.D.
Final Self Study, October 2010 Page 123
UNR School of Community Health Sciences
Adjunct Faculty
Medicine
Medicine
WCHD
St Mary's Regional Medical Center
University of Alexandroupolis, Greece
Sanders Mary
Crawford Jason
Chen Lei
Barella Lisa
Panagiotidis Mihalis
Ph.D.
M.D., M.P.H.
Ph.D.
Ph.D., M.B.A.
Ph.D.
4.1.c. Description of the manner in which the faculty complement integrates perspectives from the field of practice, including information on appointment tracks for practitioners, if used by the program.
Faculty members comprise former public health practitioners and are well integrated with the public health practice community. Faculty participate and serve as executive board members for the Nevada Public Health Association, and the Northern Nevada Chronic Disease Coalition, as examples.
A major way faculty integrate practice is the use of course guest lecturers from public health practice professionals. In addition, students travel to public health practice sites in the community and provide service as part of coursework. Public health professionals serve as members of student committees and we have obtained approval from the University’s graduate school to allow each student committee to contain 1 member to be a representative from a community agency (most typically, the internship preceptor). The student’s culminating project must be a collaboration with a public health community group. Applied scholarly work is as important to successful promotion and tenure as is theoretical or lab-based work.
4.1.d. Identification of outcome measures by which the program may judge the qualifications of its faculty complement, along with data regarding the performance of the program against those measures for each of the last three years.
As examples from Table 4.1.d., faculty have met or exceeded the program’s objectives in regards to being members of community boards/committees, providing technical assistance to the community, publishing, and increasing grant funding. Other objective targets which have not been met every year include publishing/presenting with community members and being recognized for leadership.
Final Self Study, October 2010 Page 124
UNR School of Community Health Sciences
Table 4.1.d. Goals and objectives related to faculty performance.
2) Goal: “To develop the knowledge base for public health through research.”
Objectives:
1.
At least 60% of faculty will publish an article in a peer-reviewed journal by
2011.
2.
At least 70% of faculty will present research results at a conference by 2011.
3.
At least 70% of faculty will submit one proposal for grant funding by 2011.
4.
Number of new external fund awards and amount of awards per FTE will increase
5% by 2011.
2007 to 2008 2008 to 2009 2009 to 2010
Data Data
75% 71% 63%
88%
69%
31%
$187,299 per faculty FTE
71%
71%
43%
$92,312 per faculty FTE
59%
75%
44%
$84,671 per faculty FTE
>5% increase
2006-2007 Baseline:
3 faculty received grants
Total amount = $261,090
$18,649 amount/faculty FTE
3) Goal: “To be recognized for leadership in innovative approaches to public health”
Objectives:
1.
At least 25% of faculty holding positions on advisory boards, review panels, study sections, editor positions, and other influential bodies by 2015.
2.
30% of faculty will share health-related information with community or media by
2011.
4) Goal: “To engage with multiple communities through professional and scholarly service.”
Objectives:
1.
By 2011, 40% of faculty will co-author reports and publications with colleagues at other units on campus.
2.
By 2011, 30% of faculty will co-author reports, publications, and presentations with community members.
2007 to 2008 2008 to 2009 2009 to 2010
Data Data
39%
17%
38%
19%
21%
37%
2007 to 2008 2008 to 2009 2009 to 2010
Data Data
56%
25%
21%
36%
31%
35%
Final Self Study, October 2010 Page 125
UNR School of Community Health Sciences
Objectives: cont’d
3.
By 2011, 15% of faculty will provide workshops, trainings and continuing education opportunities to public health professionals.
4.
By 2011, 15% of faculty will provide technical assistance to the community, including but not limited to, program evaluations, consulting, data analysis, grant partnerships.
5.
By 2011, 10% of UNR faculty is members of community boards or committees.
6.
By 2011, 10% of UNR SCHS committees will include a community member.
2007 to 2008 2008 to 2009 2009 to 2010
Data Data
17%
22%
56%
N/A
4.1.e. Assessment of the extent to which this criterion is met.
This criterion is met.
19%
25%
63%
N/A
32%
26%
47%
17%
Strengths
There are sufficient numbers of faculty with the appropriate expertise to provide a quality
MPH program with emphases in social/behavioral health and epidemiology.
The faculty receive external funding to support their research, are involved with the community, are recognized as leaders, and are contributing to the field with presentations and publications.
Suggested improvements
Recent faculty retirements and attrition have reduced the number of senior faculty.
Future hires should focus on attracting high quality senior-level faculty. For this to happen, a strong champion for the SCHS needs to communicate our needs to the university administration. It is therefore important that our search for a permanent director result in the identification of a strong public health leader.
Final Self Study, October 2010 Page 126
UNR School of Community Health Sciences
4.2. Faculty Policies and Procedures . The program shall have well-defined policies and procedures to recruit, appoint and promote qualified faculty, to evaluate competence and performance of faculty, and to support the professional development and advancement of faculty.
4.2.a. A faculty handbook or other written document that outlines faculty rules and regulations.
The UNR faculty governing documents are available at http://www.unr.edu/facultysenate/govdocs/
A handbook for part-time faculty is also available at http://www.unr.edu/provost/ . The university bylaws are available at http://www.unr.edu/facultysenate/bylaws/index.html
4.2.b. Description of provisions for faculty development, including identification of support for faculty categories other than regular full-time appointments.
There are numerous opportunities and support for faculty, although there have been some cuts in recent years due to budget considerations. Junior Faculty in tenure-track positions are eligible for research grants of up to $15,000 offered by the university and three school faculty have received grants. There are identified mentors at the school and college level for junior faculty.
Until 2009, an Excellence in Teaching Program provided training and classroom observations.
To supplement this program, the school has had lunch brown bag meetings with senior and junior faculty to discuss classroom management and teaching issues, and instituted a peer classroom observation procedure in which all school faculty participate in observing and providing feedback to other school faculty.
Each year, the University gives out a $5,000 Excellence in Research Award, a Foundation
Professor honor for excellence in teaching and research, a $5,000 Distinguished Community
Outreach Award, an advisor award, a faculty mentor award, and $10,000 in F. Donald Tibbits
Teaching Awards. All full-time university faculty and staff (advisor award) are eligible. In 2008,
Kristen Clements-Nolle was the runner-up for the Tibbits Teaching Award. The Division of
Health Sciences also has a teaching award and faculty in the school have been nominated multiple times and Nora Constantino won the award in 2007. The Nevada System of Higher
Education also gives out advisor, teaching and research awards to all member institutions consisting of UNLV, and the Desert Research Institute.
Sabbatical and development leaves are available to academic and administrative faculty after 6 years of service and every 10 years thereafter. This program enables faculty to be reassigned to projects that lead to professional advancement in instructional, service, or research areas. The program permits reassignments that may be for one-half year or less at full base salary, or more than one-half year up to one full year at two-thirds base salary. In recent years, three faculty have taken leaves to obtain public health leadership training, pursue novel scholarship, and to author a book on Veterans exposed to atomic matter. Faculty exchange programs are available and one faculty member will be teaching in Mexico during the 2010 summer months. Research and departmental funds are used to bring seminar speakers to campus and there are funds for faculty and staff to attend professional conferences, meetings, and workshops. There are opportunities for non-tenure track appointments and two faculty are currently supported as research assistant
Final Self Study, October 2010 Page 127
UNR School of Community Health Sciences professors. New tenure-track faculty are provided start-up funds obtained from the Vice-
President for Research Office to support the successful launch of their research efforts.
The school also has 5 adjunct and 29 affiliate faculty (see section 4.1.b). Affiliate faculty are people the school has identified as content experts in public health who have played a role
(or could help) in the development and direction of the SCHS. This designation also represents the school’s support for them and their work. Affiliate faculty typically are people who have taught in our program or have been involved in some other way. Potentially, they are people who could serve as resources for students (as committee members for MPH students, for example). Affiliate faculty may also act in an advisory role in guiding the school’s direction and development. There are no formal obligations or responsibilities associated with this designation. To become affiliate faculty, a nominee’s CV is circulated for approval by a vote of the faculty at large. Approval of appointments for affiliate faculty do not require support of the
Division of Health Sciences or other levels of the university administration.
See below for a listing of adjunct and affiliate faculty.
Mentorship.
Assigning mentors has been both formal and informal. In the formal process, the school’s director pairs junior faculty with senior faculty matched on the research and teaching needs of the junior faculty. In one case, a junior faculty member received two mentors (one for research and one for teaching). Mentoring involves providing guidance to junior faculty on how to protect their time, reviewing manuscripts, providing information about campus, connecting the junior person to colleagues, and conducting classroom observations. In the past, informal lunch gatherings between senior and junior faculty were set up to address classroom management strategies. Senior faculty acknowledge their mentoring activities in their yearly evaluations.
Informally, senior faculty have provided support for teaching and research, especially to junior faculty in the same emphasis (e.g., biostatistics). To formalize this process again, the interim director has been meeting with junior faculty to appoint a formal mentor based on the junior faculty’s suggestions. This process will be included in the school’s bylaws. The division has assisted by providing orientations to new faculty which have included tours of the region and introductions to community partners. Finally, junior faculty meet every year with the dean and director to discuss progress toward tenure.
4.2.c. Description of formal procedures for evaluating faculty competence and performance.
Each January, faculty members submit annual review documents summarizing their accomplishments in teaching, research, and service for the previous calendar year to the school’s personnel committee. The committee reviews the document and assesses strengths and weaknesses, and recommends a ranking of excellent, commendable, satisfactory or unsatisfactory to the school director. These evaluations are used by the school and university administration for retention, tenure and merit raise decisions.
The school’s policies and procedures for evaluating faculty for tenure and promotion are included in our bylaws (Appendix M). Tenure track faculty must be tenured by the end of their sixth year as an untenured assistant professor. An applicant for tenure, promotion, or both must submit a file containing required evidence of performance in teaching, research, and service, plus
Final Self Study, October 2010 Page 128
UNR School of Community Health Sciences supporting materials. Materials related to teaching performance include student and peer teaching evaluations, and summaries of courses taught and students advised. Evidence of research and scholarship includes a compilation of peer-reviewed papers, other publications, research grant production, and presentations at scientific meetings. Also, at least five external reviews of the candidate’s research are obtained from well-known scholars in the candidate’s field. In addition, the file includes evidence of service to the school, the university, the community, and the candidate’s profession.
Initially, the file is reviewed by the school’s Promotion and Tenure Committee, which consists of faculty members in the school. Applications for tenure alone are reviewed by committee members at or above the current faculty member’s rank, and applications for promotion are reviewed by committee members at or above the rank sought. Tenure at or promotion to associate professor requires that the candidate be rated excellent in scholarship or teaching, and at least good in the other areas (teaching or service). Tenure at or promotion to professor requires that the candidate be rated excellent in scholarship, excellent in either teaching or service, and good or excellent in the other category. All school committee members are required to vote by written ballot; these ballots and justifications are added to the file. From there the packet is evaluated by the division promotion and tenure committee and then the university committee. All materials are forwarded to the vice president of health sciences, and the VP must write a letter of evaluation for inclusion in the file. The entire file is forwarded to the provost’s office. Since
2005, all four school faculty who applied for tenure successfully obtained promotion and tenure.
4.2.d. Description of the processes used for student course evaluation and evaluation of teaching effectiveness.
All courses are evaluated by students every semester. In the last year, a web-based course evaluation form was introduced and the school has a 78% response rate from students. Since junior faculty currently in the tenure-track process began their tenure period with a paper-andpencil evaluation format, the personnel committee decided to retain that procedure for junior faculty to maintain consistency in their evaluation method. In the future, all faculty will be evaluated using the online form.
Course evaluation forms will be provided in the onsite resource file. In addition, faculty conduct course evaluations throughout the semester rather than obtaining feedback only at the end of the semester when the course is over. In addition to assessment at the end of the semester, a number of faculty integrate student evaluation opportunities throughout the course. Faculty who receive lower student evaluations (typically below 3.5 on a 5-point scale) work with the director and/or the personnel committee to establish a development plan to improve their teaching.
4.2.e. Description of the emphasis given to community service activities in the promotion and tenure process.
An applicant for tenure, promotion, or both must submit evidence of providing external service to the community in addition to providing internal service to the school, division or the university. The community may include local, national or international entities and community service activities may involve governmental and non-governmental agencies, industry, professional associations and periodicals. The kind and amount of community service expected
Final Self Study, October 2010 Page 129
UNR School of Community Health Sciences vary with rank of tenure/promotion sought. Those seeking tenure or promotion to associate professor are expected to have demonstrated participation in public-health related community service such as membership/leadership in regional professional organization, presentations or publications based on community service activities with community co-authors, volunteering to help with a community event, or technical assistance to a community-based organization. Those seeking tenure or promotion to professor are expected to have demonstrated service engagement on national or international level in addition to local services such as manuscript or grant review for national or international journals or agencies, on national advisory committees, on editorial board of periodicals, national media interviews regarding public health issues or events.
4.2.f. Assessment of the extent to which this criterion is met.
This criterion is met.
Strengths
There are a number of faculty development opportunities.
There are clear guidelines for faculty recruitment, evaluation and promotion.
Suggested Improvements
The program might include more explicit instructions for community service activities in the faculty promotion and tenure process. Faculty are concerned that there is not strong institutional support for their community-related activities in their evaluations. To help formalize this process, faculty have suggested more explicit procedures in promotion policies. The School of Medicine is a good source for these expectations and their policies will be reviewed by the personnel committee.
Final Self Study, October 2010 Page 130
UNR School of Community Health Sciences
4.3 Faculty and Staff Diversity. The program shall recruit, retain, and promote a diverse faculty and staff, and shall offer equitable opportunities to qualified individuals regardless of age, gender, race, disability, sexual orientation, religion, or national origin. In addition, our school recognizes the contributions to diversity of those from urban, rural, and frontier communities.
4.3.a. Summary demographic data on the program’s faculty, showing at least gender and ethnicity; faculty number should be consistent with those show in the table in 4.1a. Data must be presented in a table format. See CEPH Data Template H.
Table 4.3.a. Summary Demographic Data for Current Core & Other Faculty.
Core Faculty Other Faculty TOTAL
# % # % # %
Male
African American
Caucasian
Hispanic/Latino
Asian/Pacific Islander
Native American/Alaska
Native
Unknown/Other
International Male
5
0
2
0
3
0
0
0
42
17
25
1
1
14
14
6
3
3
32
16
16
Female
African American
Caucasian
Hispanic/Latino
7
0
7
0
58
58
6
6
86
86
13
13
Asian/Pacific Islander
Native American/Alaska
Native
Unknown/Other
International
0
0
0
0
TOTAL 12 7 19
In addition, 25% of current core faculty are gay/lesbian/bisexual/transgender (GLBT).
68
68
100%
Final Self Study, October 2010 Page 131
UNR School of Community Health Sciences
4.3.b Summary demographic data on the program’s staff, showing at least gender and ethnicity. Data must be presented in table format. See CEPH Data Template I.
Table 4.3.b. Summary Demographic Data for Staff.*
Caucasian Male
African American Male
Hispanic/Latino Male
Asian/Pacific Islander Male
Native American/Alaska Native Male
Unknown/Other Male
Staff TOTAL
International Male
African American Female
Caucasian Female
Hispanic/Latino Female
Asian/Pacific Islander Female
Native American/Alaska Native Female
Unknown/Other Female
International Female
TOTAL 4
3**
1
3**
1
4
* Staff are those individuals not defined as students or faculty
**Includes one part-time
Table 4.3.b. includes one staff member who works at the Center for Program Evaluation.
4.3.c. Description of policies and procedures regarding the program’s commitment to providing equitable opportunities without regard to age, gender, race, disability, sexual orientation, religion or national origin.
The MPH Program values the importance of a diverse faculty, staff, and student body, and follows procedures that are consistent with the policies of the university and those that are reflected in the school’s mission, goals, and objectives. Objectives to guide us in meeting this goal are listed in Table 4.3.f.
Equal Employment Opportunity Statement. The University of Nevada, Reno is committed to
Equal Employment Opportunity/Affirmative Action in recruitment of its students and employees and does not discriminate on the basis of race, color, religion, sex, age, creed, national origin, veteran status, physical or mental disability, or sexual orientation. The University of Nevada,
Reno employs only United States citizens and aliens lawfully authorized to work in the United
States. Women and under-represented groups are encouraged to apply. (University
Administrative Manual, Revised January 15, 2010, p. 110).
Affirmative Action Plan
The University of Nevada, Reno is a federal government supply and service contractor, subject to the affirmative action requirements of Executive Order 11246, the Rehabilitation Act of 1973 as amended, and the Vietnam Veterans’ Readjustment Assistance Act of 1974, Section 4212.
Final Self Study, October 2010 Page 132
UNR School of Community Health Sciences
Because the University has $50,000 or more in annual contracts with the federal government and employs 50 or more employees, we are required to prepare annual written Affirmative Action
Plans for minorities and women, for covered veterans, and for persons with disabilities.
Failure to comply with these laws and their implementing regulations, which are enforced by the
Office of Federal Contract Compliance Programs (OFCCP), can result in debarment of the
University from future contracts and subcontracts.
Affirmative Action is a term that encompasses any measure adopted by an employer to correct or to compensate for past or present discrimination or to prevent discrimination from recurring in the future. Affirmative Action goes beyond the simple termination of a discriminatory practice.
As stipulated in federal regulations, a prerequisite to the development of a satisfactory
Affirmative Action Plan (AAP) is the evaluation of opportunities for protected group members, as well as an identification and analysis of problem areas inherent in their employment. Also, where a statistical analysis of the employee workforce reveals a numeric disparity between incumbency and availability of minorities or women, an adequate AAP details specific affirmative action steps to guarantee equal employment opportunity. These steps are keyed to the problems and needs of protected group members. For minorities and women, such steps include the development of hiring and promotion goals to rectify the disparity between incumbency and availability.
Responsibility for the development of the Affirmative Action Plan resides with the Office of
Human Resources. Communication of placement goals and action oriented programs shall be communicated to the various constituencies. (University Administrative Manual, Revised
January 15, 2010, p. 116).
Sexual Harassment. It is the policy of the University of Nevada, Reno that the sexual harassment of students, employees, and users of university facilities is unacceptable and prohibited. This stance is consistent with the university’s efforts to maintain equal employment opportunity, equal educational opportunity, nondiscrimination in programs, services, and use of facilities, and the Affirmative Action program. In keeping with this policy, the University of Nevada, Reno is undertaking a plan of action to protect employees, students, and users of university facilities from sexual harassment and to rid the University of such conduct. For a complete copy of the
Sexual Harassment Policy, see Section 1,911. (University Administrative Manual, Revised
January 15, 2010, p. 110). These policies are also posted on the University’s website and available for review during the site visit.
4.3.d. Description of recruitment and retention efforts used to attract and retain a diverse faculty and staff, along with information about how these efforts are evaluated and refined over time.
Faculty. Recruitment of faulty is an ongoing process for the SCHS. To ensure students are receiving the best education, the school is committed to recruiting the best and most qualified candidates. External recruitment has taken the form of advertisements on the university’s website, at various conferences (i.e., APHA, Nevada Public Health Association), in relevant professional journals (depending on budget and timeline), and on targeted diversity sites
(available at UNR’s office of Human Resources website
Final Self Study, October 2010 Page 133
UNR School of Community Health Sciences http://www.unr.edu/hr/documents/employment/DiversityOutreach_AdvertisingResourcesInfo.do
c ).
The university’s Human Resources office works to support all of the colleges and schools in recruiting and retaining strong minority candidates for faculty positions. The school makes a specific effort to recruit diverse candidates, although it is limited by the available applicant pool.
The demographics of Northern Nevada also influence the decisions of potential job applicants from diverse backgrounds.
The Search Chair guides the committee on their responsibilities related to EEO/AA goals, the importance of applying a uniform process to all applicants and the desired end result which could be a ranking of applicants or a selection of those deemed appropriate to hire for the position (Faculty
Human Resources Recruitment Manual, p. 6). The search committee’s responsibilities toward diversity include complying with OFCCP (Office of Federal Contract Compliance Programs), which ensures due consideration for under-represented groups (UNR Faculty Human Resources Recruitment
Manual, Appendix F, p. 46) available at: http://www.unr.edu/hr//documents/employment/recruitmentmanualfinalinfo.doc
The Faculty Search Rules are sensitive to the ways in which the conduct of a search can influence the diversity of the applicant pool and of candidates hired. In addition, three distinct rules within the faculty search process directly address diversity ( bolded within the list below).
The Faculty Search Rules (listed below) can be found in the University Administrative Manual,
Revised January 15, 2010, pp. 166-167.
Faculty Search Rules. The University of Nevada, Reno is committed to Equal
Opportunity/Affirmative Action in recruitment of its faculty. The university adheres to all federal and state laws and regulations and our policy is to hire the most qualified applicant. The following policies have been established to ensure a fair and equitable search process that conforms to applicable laws, regulations, and policies.
1. Search committees should be diverse (there should be representation from underrepresented groups).
2. Search committee members, the chair, and the coordinator must disclose any relationship with candidates to the search chair. This includes, but is not limited to teacher/student, research collaboration, professional association, or personal relationship.
3. All searches must be open for a minimum of four weeks.
4. The following Recruitment/Outreach Guidelines must be met by the search committee: a. Advertisement/posting in two sites, with at least one diversity publication/website.
b. Fifteen additional contacts by the committee to include: i. Individuals (professional contacts) ii. Institutions of higher education iii. Listservs iv. Discipline publications (journals, newsletters)
5. For administrative positions, minimum qualifications must match the Position Description
Questionnaire (PDQ).
6. The EEO Summary Report must be distributed to the search committee by the search coordinator when the search closes to applicants or before interviews are conducted.
Final Self Study, October 2010 Page 134
UNR School of Community Health Sciences
7. The screening process (including interview questions) must be job related and standardized for all candidates.
8. HR approval is required at the following stages of the process: a. Initial requisition (request for fill)
b. Applicant pool
c. First interview
d. Second interview
e. Request to offer/compliance form
9. The search coordinator must update the status in e-SEARCH whenever a candidate declines an interview or a job offer.
10. The search coordinator is required to submit justification on the compliance form in e-
SEARCH for salary offers over the acceptable mid-range.
11. The signed pre-employment certification must be submitted with the new hire paperwork for the successful candidate.
12. Campus interviews must be conducted with at least two finalists unless waived by the HR department.
13. References must be verified in at least the candidate(s) selected for the position.
14. Documents that are specified in the Recruitment Manual must be uploaded to the e-
SEARCH system at the conclusion of the search. Any documents that are not able to be uploaded to e-SEARCH must be retained by the department for three years.
Faculty Retention. The school attends to the development and retention of all faculty members.
New faculty are supported through a mentoring program within the school whereby new faculty are paired with more senior faculty and encouraged to attend university- and division-sponsored tenure and promotion activities. All faculty are evaluated annually, with extensive third, fourth, and fifth year reviews. Within the school, teaching is peer-reviewed and feedback is provided annually. The school encourages and supports collaborations and service responsibilities across the school, the Division of Health Sciences, and the university as a way to enrich opportunities for diversity.
Staff Recruitment and Retention. All appointments must be approved by University’s Business
Center North (BCN) Human Resources office and comply with Affirmative Action and State of
Nevada requirements. Job announcements are posted on NV APPS, BCN Human Resources, and
WorkReno.com websites. Included on these websites is the University of Nevada, Reno Equal
Employment Opportunity Statement, which is listed in section 4.3c. The compliance checklist for hiring includes questions regarding the diversity of the interview panel, and diversity of the applicant pool. Given that the school has only three staff positions (two administrative staff positions and one student worker), we have been somewhat successful in achieving a diverse staff through our hiring of student workers.
Plans/efforts to Increase Diversity of Program Faculty. Although our faculty are diverse in terms of gender, age, sexual orientation, research interests, country of origin and other factors, we would also like to be reflective of underrepresented minorities within the U.S., namely Latinos and African Americans. We have increased our efforts to attract a diverse candidate pool in our faculty searches but because diversity is one of our values, we have discussed additional plans to
Final Self Study, October 2010 Page 135
UNR School of Community Health Sciences increase our faculty diversity. This issue has been addressed at our fall 2010 planning retreat and faculty meetings. The self-study subcommittee for faculty diversity also met this fall to discuss plans in more detail and consulted other units on campus and other organizations with diverse employees about their efforts.
In reflecting on this issue, we first acknowledged that we may need to have more efforts in place than other schools because the minority racial/ethnic composition of the Reno/Sparks area is not high relative to other job markets which makes it harder to attract diverse candidates. In addition, UNR does not have the same resources to attract high quality diversity candidates as do other schools.
We are currently searching for a permanent school director and a junior-level epidemiologist and our diversity plans this year have focused on these faculty searches. In addition to our previous efforts which included sending recruitment letters directly to diversity candidates and programs with centers addressing health disparities, we are also going to: 1) send recruitment materials to
Historically Black Colleges, schools which have programs for Native Americans such as
Stanford, Dartmouth, and tribal colleges such as in Montana, Oklahoma 2) ask our job applicants how their work contributes to diversity as part of the interview process, and 3) as a means of recruiting, continue our individual faculty effort of talking about our inclusive environment to our racially diverse colleagues and to those we meet at meetings such as APHA. For example, job announcment were provided to people working closely with tribal colleges at a regional
SAMHSA meeting held at UNR in October 2010.
The Division Director of Internal/External
Relations and school steering committee member, Richelle O’Driscoll, has agreed to follow up with UNR administration to identify how UNR promotes its support of diversity to job applicants
(e.g., materials directed toward diversity candidates on the university webpage). If there are additional materials needed, school faculty have volunteered to serve on a taskforce to address this. In their yearly evaluations, faculty and staff will reflect on how they have contributed to the school’s values including diversity. Finally, we plan to increase the racial/ethnic diversity of our school’s advisory board.
4.3.e. Description of efforts, other than recruitment and retention of core faculty, though which the program seeks to establish and maintain an environment that supports diversity.
The school is supported in its diversity efforts by various programs throughout the university.
Three programs on campus focus on diversity and offer undergraduate majors or minors, master’s degrees, certificates, or specialization (see list below). The Gender, Race, and Identity
Program is dedicated to assuring that UNR students develop a deep understanding of the impact of race, class, ethnicity, and gender on their identities, as well as their society. This Program has several core faculty and over 30 affiliate faculty drawn from many departments on campus:
Anthropology, Basque Studies, Community Health Sciences, Computer Science and
Engineering, Counseling and Educational Psychology, Curriculum, Criminal Justice, Educational
Specialties, English, Foreign Languages and Literature, Geography, History, Music and Dance,
Philosophy, Political Science, Psychology, Social Work, and Sociology. Three members of our school (Boutté, Cook, and Sugar) are Faculty Affiliates of this program.
Developmental Disabilities Program
Undergraduate Interdisciplinary
Minor
Final Self Study, October 2010 Page 136
UNR School of Community Health Sciences
Graduate Interdisciplinary
Specialization
Gender, Race, and Identity Program
Women’s Studies: Undergraduate
Major and Minor
Ethnic Studies: Undergraduate
Minor
Holocaust, Genocide and Peace
Studies: Undergraduate Minor
Religious Studies: Undergraduate
Minor
Gender, Race, and Identity: M.A.,
Graduate Certificate
Gerontology Programs
Undergraduate Minor
Gerontology Certificate
A number of additional academic programs and resources are available to engage and nurture faculty, staff, and student diversity, including:
Center for Basque Studies
Center for Excellence in
Developmental Disabilities
Center for Holocaust, Genocide and
Peace Studies
Center for Student Cultural Diversity
Disability Resource Center
Latino Research Center
Office of International Students and
Scholars
Sanford Center for Aging
University Studies Abroad
Consortium (USAC)
Veteran Services and
Admissions/University Veterans’
Coalition
Program Efforts to Maintain an Environment Supportive of Faculty Diversity.
Program faculty acknowledge that this is an area where more attention is needed; however all faculty and staff are committed to promoting an inclusive environment. To that end, there have been no concerns raised from any faculty, staff or student that their diversity of opinion, background, or experience is not supported or welcome. Having some diversity (race/ethnicity,
GLBT) among the faculty and staff helps support inclusiveness.
Beyond the existing racial/ethnic composition of our faculty, faculty diversity is supported through research activities. For example, faculty are working with Latino, Native American,
African American, LGBT, older adult and rural populations, examining racial/ethnic disparities in reporting of study participants, and examining issues affecting incarcerated populations. Posters promoting our value of diversity are displayed throughout our school and how our policies might affect low-income and racial/ethnic minorities is considered when making decisions. Faculty are also encouraged to become part of university committees and community organizations which promote diversity. Establishing a more formal mentoring process for junior faculty is one plan which would help in this area.
The program must also insure that new faculty are included in the Alliance of Racial Minorities.
The Alliance of Racial Minorities, in concert with the President’s at University of Nevada, Reno and Truckee Meadows Community College, host an annual luncheon to welcome new faculty and staff of color from these institutions. Not only is the luncheon a way of saying welcome and creating new networks, it is also a way of expressing appreciation for individual talents and offering the assistance of the ARM community if there are questions or concerns.
The goal of this alliance is to assist with the retention of faculty and staff of color.
Final Self Study, October 2010 Page 137
UNR School of Community Health Sciences
4.3.f. Identification of outcome measures by which the program may evaluate its success in achieving a diverse faculty and staff, along with data regarding the performance of the program against those measure for each of the last three years.
Table 4.3.f. Outcome Measures, Targets, and Data for Faculty and Staff Diversity.
5) Goal: To expose students to diversity in multiple venues.
Objectives:
1.
Faculty and staff are representative of women, underrepresented minority, and other diverse groups in the relevant labor markets* by 2015.
Relevant Labor Market Targets:
Women: Faculty:54%; Staff: 46%
Minority: Faculty:16%; Staff: 21%
2.
Efforts to recruit diverse faculty and staff will increase by 5% for each new hire.
3.
By 2011, 50% of faculty address issues affecting underrepresented populations in
2007 to 2008 2008 to 2009
Data Data
Women:
Faculty: 50%
Staff: 67%
Minority
Faculty: 17%
Staff: 50%
No Search
50%
Women
Faculty: 56%
Staff: 100%
Minority
Faculty: 19%
Staff: 25%
No Search
59%
2009 to 2010
Data
Women
Faculty: 65%
Staff: 83%
Minority
Faculty: 15%
Staff: 50%
3 specific efforts
58% their work.
*The relevant labor markets used for comparison are Washoe County Labor Force for staff and
Public Health PhD Graduates for faculty (ASPH, 2004).
No faculty searches occurred during the academic years 2007-2008 and 2008-2009. For the search in 2009-2010, the above policies on recruiting a diverse faculty were followed. Three additional efforts were undertaken to specifically attract a diverse labor market (as reflected in
Table 4.3.f.). Personal solicitationss from the school’s director were made to program directors and faculty who either offered training in health disparities at their institutions (e.g., housed a
Center for Health Disparities) or who specialized in research in minority health issues.
Secondly, search announcements were sent to people listed in the Directory of Women and
Minority Doctoral Researchers who had public health backgrounds. Finally, search advertisements were placed in publications which addressed issues of minority health and with
DHHS’s Office of Minority Health. UNR’s EEO race summary of applicants for this search showed: 4 Non-Disclosed, 14 Asian, Native Hawaiian, Pacific Islander, 4 African American, 2
Latino/Hispanic, and 9 White.
4.3.g.Assessment of the extent to which this criterion is met.
This criterion is met.
Strengths
Our faculty are diverse in terms of age, gender, ethnicity, sexual orientation, religion, and national origin. Currently, there is an equal number of male and female faculty.
The University has policies in place to facilitate recruitment and retention of diverse faculty.
Final Self Study, October 2010 Page 138
UNR School of Community Health Sciences
The school, through specific activities and mentoring, encourages and maintains a productive environment for recruitment and retention of minority faculty (see 4.3.d,
4.3.e).
We have been successful at recruiting and retaining student workers from diverse backgrounds.
The school is committed to increasing the diversity of its faculty and staff.
Suggested Improvements
In addition to increasing diversity in its tenure-track ranks, the school should consider clinical faculty and adjunct appointments as a means to diversify its faculty. However, the school can only hire from a pool of qualified applicants, and securing a diverse pool is challenging for the university as a whole.
Our current diversity does not fully reflect the ethnic diversity of the community, which contains individuals who are Native American and Hispanic. In terms of staff, we are currently limited to two full-time administrative staff positions and one student worker to support the school’s operations (compared to center staff).
Another strategy will be to recruit more diverse students into the program (i.e., Native
American, African American, and Hispanic individuals), and offer encouragement and support for them to apply for doctoral programs. These students would add diversity to the pool of qualified candidates for faculty recruitment.
The school should engage in ongoing data collection and annual review of these indicators toward the objective of diversifying the faculty, staff, and students.
Final Self Study, October 2010 Page 139
UNR School of Community Health Sciences
4.4 Student Recruitment and Admissions. The program shall have student recruitment and admissions policies and procedures designed to locate and select qualified individuals capable of taking advantage of the program’s various learning activities, which will enable each of them to develop competence for a career in public health.
4.4.a. Description of the Program’s recruitment policies and procedures
Recruitment Policy.
The University of Nevada Reno School of Community Health Sciences
Master of Public Health Program recruits qualified and dedicated students with a diverse range of interests, educational and work related backgrounds, to bring into their programs of study a vast repertoire of experiences and motivations for advancing their public health careers. We value the backgrounds of our students and know that they contribute to classroom and experiential learning for the student, their colleagues, and faculty in the program.
Therefore, in both our recruitment and selection process we recognize and value diversity in our
MPH student body the MPH program. We adhere to the university's affirmative action and equal opportunity policies and all of its requirements in admission activities. Our program admits qualified students regardless of race, ethnicity, religion, sex, sexual orientation, national origin, disability, or veteran’s status. Further details will be discussed in section 4.5.
Recruitment Procedures.
The responsibility and activities of recruitment for MPH students are multidimensional and involve many people including:
Graduate Director – based upon applicant inquiries, meets with all applicants face-to-face when possible before applications are completed;
The Graduate Faculty and Graduate Committee – integral in recruiting and retaining our students by engagement with students in their areas of interest;
“Graduate Special” students – graduate students not enrolled in the MPH program but who take our core courses as a way of evaluating the program’s potential for them
UNR Graduate School staff who attend certain graduate school fairs in other states (e.g., diversity fairs);
Our current MPH students who participate through word of mouth and answering requests from potential applicants;
Our Website;
Our collaborative academic programs – University of Nevada School of Medicine and
Orvis School of Nursing;
Academic Fairs – both at UNR and at other non-MPH Universities;
Career fairs – locally, for students coming back into academics to become more marketable;
Community Health Sciences undergraduate students – the large undergraduate program represents a source of motivated successful students who are interested in the MPH; the
Graduate Director annually visits 400-level classes for recruitment purposes;
County/State Health Department Seminars and Outreach;
APHA/NPHA meetings, booths and workshops/student presentations;
Other undergraduate students from UNR – from networking and advertisement of classes;
Faculty networks – in-state and out of state;
Final Self Study, October 2010 Page 140
UNR School of Community Health Sciences
Internships – MPH students meet others who are interested in their work;
Word of mouth – students, faculty, preceptors, professional networks throughout the community;
Business networking by the Graduate Director in monthly community meetings – this effort reaches out to non-traditional students who are in the workplace, some who are not even currently in the health field;
Alumni referrals – as alumni numbers grow, so do referrals;
Social Networking – by students and through the Facebook MPH Group.
We continue to look for unique opportunities to recruit students in different areas as identified by our current students, colleagues, alumni, and other community support networks.
4.4.b. Statement of admissions policies and procedures.
The graduate committee annually reviews admission requirements for the MPH program to insure its consistency with our program’s mission, modifying as necessary.
Admissions are for fall semesters only with a final deadline of February 15 for applications. This deadline represents a change from a twice-yearly admissions process and was instituted to assist students in staying on course progression for graduation.
The Graduate School receives and processes their required materials (transcripts and official test scores) from the student in their information system, Nolij.
Then, the graduate director (via the
Administrative Assistant by accessing Nolij ) receives other materials (see 7, 8, 9 below) from the applicant. The student’s folder, when complete is forwarded to the graduate director.
Then monthly, at least two members of the graduate committee will evaluate any complete applications for admission. There must be agreement by both members for admission. If not, a third member will also review the application and could refer it to the monthly graduate committee for review.
For MPH students approved for admission, notifications by email are then sent out by the graduate director for acceptance to those students with requests for any additional information as well as instructions for their enrollment in classes and their advisor. In addition, for students who are not admitted, an email is also sent to them as well indicating the areas that need further strengthening for a future admission. In concert, our administrative assistant notifies the
Graduate School as well through the Nolij computer-based information system.
Admissions Policies. Qualifications for admission to the Master's Program in Public Health:
Please note: Prospective students must meet the University of Nevada, Reno (UNR) and School of Community Health Sciences requirements for graduate status: http://www.unr.edu/grad/prospective/apply.asp
which includes graduating with a bachelor’s degree with a GPA or 2.75 or higher.
Once the admission qualifications for UNR are met, an application for admission to the MPH program may be made.
Final Self Study, October 2010 Page 141
UNR School of Community Health Sciences
Admissions criteria:
1.
Completed an undergraduate degree from an accredited college/university.
2.
Undergraduate grade point average (GPA) of 3.0 or higher on a 4-point scale.
3.
Graduate Record Exam (GRE) general test. We expect that students will achieve a minimum score of 1000 between the math and verbal portions of the exam. For additional information: http://www.gre.org
. The university’s institutional code to receive GRE test score reports is 4844. Other standardized exams such as the MCAT, LSAT, GMAT,
DAT are allowable in place of the GRE. For students with terminal degrees (Ph.D.,
Ed.D.) and professional degrees (M.D., D.D.S.), the GRE requirement is waived.
4.
(For International Students) A minimum TOEFL score of 500. For additional information: http://www.toefl.org
. The university’s institutional code to receive TOEFL test score reports is 4844.
5.
Provided 3 letters of recommendation specifying the student’s interest and suitability for the MPH program.
6.
Provide a sample of academic writing for review of writing abilities.
7.
Provide an “admissions essay” discussing why they are choosing to pursue an MPH and which specialization they are interested in – epidemiology or social behavioral health.
In addition, pre-requisite coursework is required for admission into the MPH Program.
Applicants will have:
1.
Completed undergraduate or graduate courses in statistics. Statistics must be completed prior to taking CHS 780: Biostatistics in Public Health and CHS 712: MPH
Epidemiology. The MPH student may be able to take a statistics course in summer school prior to starting their progression of study in fall.
2.
Students who have not completed an undergraduate patho-physiology course must complete CHS 200 - Public Health Biology, a course that grounds a student in health science. It is preferable that the student have this background/course before applying, but with the Graduate Director approval, this course can be taken after admission is approved.
While relevant work in the health field is not required for admission into the program, evidence of this helps ensure a proper alignment and knowledge of public health values consistent with our MPH program. However, we also do encourage students with non-health related backgrounds to inquire about the program and if appropriate, to apply. It adds to the diversity of experiences of students who will now choose public health as a future direction without having had that background in their past.
4.4.c. Examples of recruitment materials and other publications and advertising that describe, at the minimum, academic calendars, grading, and the academic offerings of the program.
Online recruitment materials:
UNR MPH Website: http://hhs.unr.edu/schs//mph_specializations.html
UNR MPH Epidemiology Specialization: http://www.unr.edu/public-health/epi.html
UNR MPH Social Behavioral Health Specialization: http://www.unr.edu/publichealth/soc_behav_health.html
UNR MPH Application Process: http://www.unr.edu/public-health/mph_specializations.html
Final Self Study, October 2010 Page 142
UNR School of Community Health Sciences
UNR On-Line Catalogue: http://www.collegesource.org/displayinfo/catalink.asp?pid={BEBD014F-27B7-4E88-8602-
907D92100065}&oig={5A4EB770-8240-435B-B867-8595F430D8C9}&vt=5
UNR Graduate School: http://www.unr.edu/grad/
UNR Academic Calendars: http://www.unr.edu/catalog/uccc/text/10-
11cat_1stDRAFT/10CALENDAR.pdf
Additional recruitment materials to be developed.
MPH Student Handbook (see Appendix N).
4.4.d.
Quantitative Information on the number of applicants, acceptances, and enrollment, by specialty area for each of the last three years.
Table 4.4.d. Quantitative Information on Applicants, Acceptances, and Enrollments by
Program Area, 2007 to 2010.
Epidemiology Applied
Accepted
Enrolled
Academic Year
2007 to 2008
3
3
3
Academic Year
2008 to 2009
7
7
7
Academic Year
2009 to 2010
9
8
7
Social/Behavioral
Health
Applied
Accepted
Enrolled
Applied
7
7
7
0
3
3
3
0
12
12
9
4 MPH/MD**
Accepted
Enrolled
0
0
0
0
4
4
**Accepted students beginning 2009-2010.
Our acceptance rates are high. We feel this reflects well on our pre-application advisement with prospective students (see section 4.6.a.). We spend time as needed with prospective students to ensure our program matches their career interests including arranging for them to meet with current students and alumni. In addition, many students apply after taking 1 or 2 courses as a graduate special (see below). In those cases, both the student and the faculty have realized that our program is the right fit for the student. There are cases in which students do not reflect their desired area of emphasis (e.g., epidemiology or social/behavioral health) in the application.
These students are more likely to be rejected: Of the 7 who applied in 2009-2010 and did not select an emphasis, only 3 were accepted (43%; data not reflected in Table 4.4.d.). For those we accept, we work with the incoming student to determine the best area of emphasis for them based on their stated purpose for choosing an MPH, their career plans, and their strengths. None of the
3 accepted with area unspecified enrolled.
Final Self Study, October 2010 Page 143
UNR School of Community Health Sciences
4.4.e.
Quantitative information on the number of students enrolled in each specialty area identified in the instructional matrix, including headcounts of full- and part-time students and a full-time equivalent conversion, for each of the last three years. Explain any important trends or patterns, including a persistent absence of students in any Program or specialization.
Table 4.4.e. Students Enrolled in Each Degree Program by Area of Specialization, 2007 to
2010.
2007 to 2008 2008 to 2009 2009 to 2010
HC
FT
HC
PT
FTE HC
FT
HC
PT
FTE HC
FT
HC
PT
FTE
Epidemiology
Social/Behavioral
Health
9
4
1
5
9.56
6.83
10
5
6
6
12.72
9.17
MPH/MD** NA NA NA NA NA NA
**NA = not applicable. Accepted students beginning 2009-2010.
11
5
3
9
13
1
15.06
11.22
3.83
In addition to the students enrolled in a degree program, there are about 15 students who are taking MPH courses as graduate specials. Graduate specials can take up to 9 credits without being admitted to a degree program. Graduate special status allows potential students to learn more about the MPH program. Almost every graduate special student decides to apply to the program.
4.4.f.
Identification of outcome measures by which the Program may evaluate its success in enrolling a qualified student body, along with data regarding the performance of the
Program against those measures for each of the last three years.
Table 4.4.f.
Outcome Measures, Targets, and Data for Students Admitted to MPH
Program.
2007-2008 2009-2010 1) Goal: “To prepare future public health practitioners, researchers, educators and leaders.”
Objective 1): Recruitment/Admissions
1a. By 2011, 80% of students enrolled in the
MPH program will have an overall undergraduate GPA that exceeds 3.2.
1b. By 2011, 40% of students enrolled in the
MPH program will have verbal and quantitative GRE scores that exceed the 50 th percentile.*
53%
31%
67%
33%
70%
47%
*N = those students with GRE scores. A few students complete other entrance exams (e.g.,
MCAT, LSAT).
4.4.g.
Assessment of the extent to which this criterion is met.
Final Self Study, October 2010 Page 144
UNR School of Community Health Sciences
This criterion is met with commentary.
Strengths
The Graduate Director and faculty value personal meetings with prospective students.
A high percentage of completed applications are obtained from prospective students who inquire about the MPH program after meeting with the Graduate Program Director, with current students, or talking to faculty with related interests.
Overall faculty involvement in recruitment and admissions is high.
The MPH student base supports word-of-mouth marketing.
Potential students are known due to personal contact prior to admission and are well screened for good match with program.
Applicants demonstrate diverse backgrounds/degrees, especially in academic training and interests within the field.
Alumni support through the school’s advisory board is strong.
Resources have been obtained to recruit students externally from UNR (e.g., to go to
APHA or similar conferences to reach out to potential students).
Suggested Improvements
The school needs improved website design and content. The program website is one of our weaknesses. The steering committee has discussed solutions during the 2009-2010 academic year. The following changes were made: More program control of the website has been obtained (compared to Division or UNR oversight); Progam staff have been trained in webdesign; Current MPH students evaluated the usability of the website; A graduate assistant has taken on the oversight of the student webpage, and in the summer of 2010 a new website was launched which is a significant improvement over the previous site. An ongoing goal is to have it be more engaging for prospective students.
A plan for this goal is to increase videos from students on the site and this material is currently being obtained.
Communications and marketing would be enhanced with more formal written materials to hand out to referral areas and potential students. Updated materials have recently been produced; however we recognize that more is needed.
The program could host workshops on public health issues on campus for current students.
SCHS could hold Webinars for our community partners. A plan to achieve this is the increasing number of courses we are offering online. Faculty have been asked to develop an online course in the next year and university resources have been obtained to provide training in this area.
SCHS should develop a 3 + 2 BS/MPH program – students complete their BS and MPH in five years (see Section 2.10).
Final Self Study, October 2010 Page 145
UNR School of Community Health Sciences
4.5 Student Diversity . Stated application, admission, and degree-granting requirements and regulations shall be applied equitably to individual applicants and students regardless of age, gender, race, disability, sexual orientation, religion or national origin.
4.5.a. Description of policies, procedures and plans to achieve a diverse student population.
The MPH program values diversity within its students, faculty, and staff. The program seeks to recruit, retain, and serve diverse populations and to contribute to a climate of tolerance, inclusion, and collaboration within the program, the University, and the community. We believe that diversity supports and creates a rich learning environment, more effective public health professionals and initiatives. Key program values - professionalism, integrity, diversity, community/collaboration and, building knowledge and learners - were collectively established by faculty, staff, and students and reflect a culture of inclusion.
Diversity issues are interspersed throughout the curriculum - addressing the majority of the
ASPH competencies in diversity and culture (60% of the competencies in the MPH core and
100% in the Social and Behavioral Health specialty area). Many courses focus on diversity issues, including world health, cultural diversity, rural health issues, HIV/AIDS, and most recently, a course on health care systems in other countries that will include course activities conducted in Toronto, Canada is planned for summer 2011.
The University is an Equal Opportunity/Affirmative Action employer and does not discriminate against faculty, students or staff on the basis of race, color, religion, sex, age, creed, national origin, veteran status, physical or mental disability, or sexual orientation in any program or activity it operates. ( http://www.unr.edu/eoaa/ada.html
). The University’s Division of Student
Services’ ( http://www.unr.edu/stsv/vpstsv/ ) policy statement includes a commitment to diversity with seventeen objectives to foster and support diversity in the areas of student learning and success; hiring, training, and professional development; and collaboration and outreach.
4.5.b. Description of recruitment efforts used to attract a diverse student body, along with information about how these efforts are evaluated and refined over time.
Specific efforts to recruit a diverse student body have included efforts to personally encourage diverse undergraduate students to apply to the program, to recruit from diverse groups affiliated with UNR, and graduate school diversity `recruitment fairs. Students who express an interest in the program are contacted and provided with information about the program and the field.
The program expects and fosters student success. The graduate director and the graduate committee oversee program efforts to recruit and retain a diverse student body. The MPH
Student Affairs Committee assesses student progress, identifies potential student difficulties, and supports students and faculty to promote student success. These committees meet monthly and at least three times a semester, respectively, in order to review activities and revise strategies as needed. The entire faculty serves a crucial role in advising and mentoring students as they investigate career options and interests, during their graduate school application process, and throughout the program. The program is aware of the need to help students transition as they begin a new academic program and move to a new geographical or cultural location. The program actively seeks to assist students in this transition; for example, the program often facilitates social networking for students with similar backgrounds/cultural experiences.
Final Self Study, October 2010 Page 146
UNR School of Community Health Sciences
All of these recruitment and retention efforts are tracked qualitatively to monitor what efforts are taking place, where modifications need to be made, and identifying new opportunities to increase and maintain a diverse student body. Feedback is regularly sought from students, alumni, and faculty and used to make improvements.
The University has several programs that support recruitment and retention of a diverse student body. The University participates in Western Interstate Commission on Higher Education’s
(WICHE) Western Regional Graduate Program (WRGP) which provides graduate students from
14 states reduced tuition rates. The University maintains a website
(http://www.unr.edu/diversity/) that provides information and resources for diverse groups. The site also provides committee reports related to diversity issues from five regularly-standing diversity committees. The Graduate School offers diversity fellowships for incoming students which covers 100% of tuition costs. In 2007, an incoming MPH student unsuccessfully applied for the fellowship following a recommendation by the school’s graduate program director. The student was awarded a departmental graduate assistantship position, however.
The University’s Center for Student Cultural Diversity (http://www.unr.edu/stsv/cscd/) provides numerous “programs and services that promote recruitment and retention, the pursuit of academic success and graduation” for students that self-identify as African American, Asian
American/Pacific Islander, American Indian, Hispanic/Latino, first-generation college students, low-income, and lesbian, gay, bisexual or transgendered. Several diversity groups exist on campus including, the Black Culture Cooperative, Asian Pacific Islander Heritage Project, Las
Culturas, Intertribal Higher Education Program, Pride Collaborative, and Mosaic. The Office of
International Students and Scholars provides ( http://www.unr.edu/oiss/students/clubs.html
) programs and a very active International Club. The Associated Students of the University of
Nevada and the Graduate Student Association ( http://www.unr.edu/gsa/default.html
) run household item and food pantry programs for students in need of temporary assistance, as well as support over a dozen student-led diversity groups.
The graduate catalog ( http://www.unr.edu/grad/forms/grad_catalog.asp
) and Graduate Student
Association (GSA) handbook ( http://www.unr.edu/grad/forms/docs/GraduateSurvivalHandbook.pdf
) cover information regarding local housing, transportation, health care resources, and cultural/recreation opportunities; as well as GSA-sponsored activities and funding, graduate student rights and responsibilities, academic services, and vital information and resources available for international students. The handbook also provides information regarding policies and procedures to address academic problems, legal issues, student advocacy, sexual harassment, counseling services, and financial crisis assistance.
4.5.c. Quantitative information on the demographic characteristics of the student body, including data on applicants and admissions, for each of the last three years. Data must be presented in table format. See CEPH Data Template L.
Final Self Study, October 2010 Page 147
UNR School of Community Health Sciences
Table 4.5.c.1. Demographic Characteristics of Student Body from 2007 to 2010.
2007-2008 2008-2009 2009-2010
Applied
M F
1
M F
1
M F
African American Accepted
Enrolled
1
1
1
1
Caucasian
Applied
Accepted
Enrolled
12
12
11
1
1
1
6
6
6
6
6
5
13
13
12
Hispanic/Latino
Applied
Accepted
Enrolled
Asian/Pacific Islander Applied
Native
American/Alaska
Native
Accepted
Enrolled
Applied
Accepted
Unknown/Other
Enrolled
Applied
Accepted
Enrolled
Applied
International Accepted
Enrolled
Applied
TOTAL Accepted
3
2
2
3
2
1
1
1
2
2
1
2
2
2
2
20
20
1
1
1
2
2
1
1
1
1
1
2
2
2
11
11
2
1
5
3
1
13
10
1
1
1
19
1
1
5
4
3
20
Enrolled 2 14 2 10 6 16
Table 4.5.c.1. includes students accepted into some emphases which are not being submitted for accreditation review due to: 1) the need to update the curriculum (MSN/MPH) and 2) because the emphasis is no longer viable due to the loss of faculty (environmental/occupational health and health policy/administration). We are no longer accepting students into these emphases.
When the dual MSN/MPH curriculum is updated to be in line with CEPH standards, we will reopen that emphasis and submit it for accreditation review at the appropriate time. Health policy/administration and environmental/occupational health will not be considered for degree offerings unless more faculty are obtained. Table 4.5.c.2. presents the breakdown of the 2007-
2010 student body by emphasis. There are 6 students currently enrolled (fall 2010) in emphases not being submitted for accreditation (2 students in the MSN/MPH dual degree, 1 student in environmental/occupational health, and 3 students in health policy/administration.
Final Self Study, October 2010 Page 148
UNR School of Community Health Sciences
Table 4.5.c.2
. Students accepted and enrolled by emphasis for the last 3 years.
Emphasis 2007-2008 2008-2009 2009-2010
Epidemiology
Social Behavioral
MPH/MD
Total students enrolled in emphases submitted for accreditation
Environmental/occupational health
3
7
0
10
1
7
3
0
10
7
9
4
20
1
Health ethics/policy/administration
Nursing/MPH
Area unspecified
2
2
1
1
1
1
Total all students accepted and enrolled
16 12 22
Table 4.5.c.3. Demographic Characteristics of Total Enrolled Student Body for the Last 3 Years, 2007-2008, 2008-2009, 2009- 2010.*
2007-2008 2008-2009 2009-2010
African American
Caucasian
Hispanic/Latino
Asian/Pacific Islander
Native
American/Alaska
Native
Other: Iranian
International
TOTAL
M
6
3
9
F
3
27
2
2
1
1
36
M
5
1
4
10
F
3
21
2
1
3
30
M
8
1
4
13
F
1
29
2
2
5
39
*Includes MPH students enrolled in emphases which are no longer admitting students
(e.g., generalist, health ethics/policy).
4.5.d. Identification of measures by which the program may evaluate its success in achieving a demographically diverse student body, along with data regarding the program’s performance against these measures for each of the last three years.
The program has adopted goals and objectives to promote recruitment of a diverse student body.
These targets, with data for the last three years where available, are presented in Table 4.5.d.1.
Final Self Study, October 2010 Page 149
UNR School of Community Health Sciences
Table 4.5.d.1. Outcome Measures for Student Diversity in the MPH Program.
Outcome Target 2007-2008 2008-2009 2009-2010
Measure
Number and type of recruitment efforts for students
By 2011, efforts to recruit underrepresented populations for the
MPH program will increase by 10%.
1
Attended
California
Diversity Fair
1
Attended
California
Diversity Fair
2
Attended
California
Diversity and
Women in
Higher
Education Fairs
4% Race/ethnicity information for students admitted to the program
Work or volunteer experience reported in students’ program applications
By 2011, historically underrepresented racial/ethnic populations will comprise 20% of the students enrolled in the
MPH program.
By 2011, 20% of MPH applicants will report experience working with underrepresented populations.
13%
100%
25%
90% 73%
The program includes a number of international students from countries including Belize, Africa,
India, and China who are not reflected in our data on underrepresented students. The faculty felt that the objective should focus on historically underrepresented minorities in the United States.
However, the students have commented that the diversity represented by students from other countries has greatly enhanced their learning experiences. In addition to historically underrepresented racial/ethnic minorities, we have had a number of openly gay/lesbian/bisexual/transgender students which speaks to our inclusive environment and further enriches the students’ experiences. In the newly admitted cohort for 2010-2011, 3 students (of
14 accepted) are members of a racial/ethnic minority group (21%).
Final Self Study, October 2010 Page 150
UNR School of Community Health Sciences
4.5.e. Assessment of the extent to which this criterion is met.
This criterion is partially met.
Strengths
There is widespread support in the program and from faculty and in the University’s values, policies, and resources for a diverse student body.
There exist some procedures to foster student success and involvement.
We have a history of diverse students in the program.
Suggested Improvements
The MPH program will develop strategic plan to increase recruitment and enrollment of students from diverse populations. A graduate committee taskforce on student recruitment has been developed. In particular, a current MPH student is reaching out to student diversity groups on campus.
The SCHS will add statements of inclusion and diversity, as well as the program’s values, on school and program websites, recruitment materials, brochures, and program student handbook.
SCHS will increase outreach and recruitment efforts that are tailored for diverse populations.
SHCS will seek to increase financial support for diverse students. One recent source identified is the University’s McNair scholars program which prepares underrepresented juniors and seniors for doctoral study by offering tuition support, mentoring, GRE testtaking support and assistance with writing letters of application.
Final Self Study, October 2010 Page 151
UNR School of Community Health Sciences
4.6. Advising and Career Counseling. There shall be available a clearly explained and accessible academic advising system for students, as well as readily available career and placement advice.
The MPH Program provides personal academic advising and career and placement counseling for its students.
4.6.a. Description of the advising and counseling services, including sample orientation materials such as student handbook.
Advising. Applicant advising - Interested students initially meet with the Graduate Director to explore options and to ask questions about the admission process and coursework. Students with particular foci of interest are then referred to faculty in that area of emphasis for more formal advisement.
Formal Advising – Upon admission, MPH students are matched with an advisor based upon their program specialization and personal interests. The advisor assists them with their Program of
Study (POS) and course selection, and begins the development of their MPH experience.
Advisors meet with students each semester, assisting in planning their coursework, then working with them to find an appropriate internship. They also assist the student while they are in the
MPH Capstone Course, all in alignment with the student’s career goals and objectives.
MPH Student fall Orientation - An annual half-day orientation is held in August for new MPH students. It is a time to meet faculty, other students and alumni, and to become familiar with the
MPH Student handbook (see Appendix N) and to ask any questions. Those who do not come to the orientation meet with the Graduate Director and/or advisor to receive the information provided at orientation.
MPH Graduate Special - At UNR, students who are not officially admitted into a program of study, and/or are in the process of completing their application, may take up to 9 units of classes.
When admitted to the MPH program, these courses can transfer into their program of study. The number of Graduate Special students is an indicator of interest in the program and of future admissions. All Graduate Special students are initially advised by the Graduate Director and/or a course faculty member until admitted into the program. However, with the increasing numbers of Graduate Specials in the program this past year, there needs to be greater emphasis, tracking, and advisement of these students, in order to assist them in transitioning into our MPH program in order to keep them on progression.
Mentoring - The mentorship is formalized with the advisor and committee chair (if different), although many other faculty are involved with mentoring students. Students are also mentored by other graduate assistants, second year students, former and current colleagues of students, graduate assistant supervisors, internship supervisors, alumni, and guest speakers. Mentoring relationships come from many places and create connections throughout the student body. A significant source of mentoring occurs during the student’s culminating experience when the advisor in his/her role as committee chair and the other project committee members guide the student through that process and discuss the student’s career plans. We value this professional development aspect of our relationships.
Final Self Study, October 2010 Page 152
UNR School of Community Health Sciences
Career Counseling
Career counseling is done both formally and informally. In the formal manner, we are a central hub for career opportunities and internship postings from many organizations in the Northern
Nevada area as well as out of the area employers. These are posted on the graduate Bulletin
Board, shared on our list-serve as well as our WebCampus site for our students. We use
WebCampus postings for internships, fellowships, and job openings. The MPH Bulletin Board in the school’s building has fliers from graduate schools and other job openings in the area and nationally
The other more formal resources are both the Graduate School and the Graduate Student
Association http://www.unr.edu/gsa/ who represent groups committed to the professional development of our students at UNR. They host a graduate school fair each fall for all UNR students to explore graduate programs including the MPH program. Each spring, a UNR career and internship fair is held on campus and students are encouraged to attend.
We have continued support from the College of Business Career Development staff and website: http://www.business.unr.edu/career/ They also host career fairs each semester that our students attend.
There is a Counseling Service on campus which support students personal and family needs: http://www.unr.edu/stsv/cs/
In the less formal and more MPH Program specific career counseling, there are many who contribute to the students’ future: their advisor, other MPH faculty, alumni, and faculty/community mentors. Public health professionals are frequent guest speakers to our classes and are available during and afterwards for students to consult with about their career choices and possibilities. As students are completing their internships, they are encouraged to meet other people at their sites, besides the preceptor, in order to create a greater networking loop. We also provide a required pre-internship meeting with students at which the Graduate
Program Director presents a session on professionalism. This has paid off with student internships becoming student employment opportunities.
Career counseling is also provided in classes. For example, in CHS 712, epidemiology, a panel discusses future job possibilities in epidemiology, how to land a job with the state or county health departments and other agencies. In addition, the classes’ webcampus site has a section that lists internship and job openings.
Professional Development Sessions and Assignments
A good deal of career counseling occurs during the professional development portion of the capstone class. Special sessions and assignments related to professional development include: group facilitation and mediation, public speaking, how to be a good supervisor, resume development, how to land a job, public health ethics, and the future of public health as a profession.
Near the end of the course students complete a competency assessment to identify competencies that need to be further developed. Students use this assessment to develop a post-graduation professional development plan. Graded assignments include:
Final Self Study, October 2010 Page 153
UNR School of Community Health Sciences
1) Resume
2) Job search and application development
3) Oral presentation (including professional dress and conduct)
4) Post-graduation professional development plan
5) Ethical issues in public health practice
The relevant professional development competencies for the capstone course are to:
Embrace a definition of public health that captures the unique characteristics of the field
(e.g., population-focused, community-oriented, prevention-motivated and rooted in social justice) and how these contribute to professional practice (J9)
Value commitment to lifelong learning and professional service including active participation in professional organizations (J11)
Because all students have advisors, a major source of career counseling is 1:1 mentoring related to the job application process. Faculty review job applications, resumes, and cover letters. This is something we continue to offer for program alumni.
Many students attend the local Nevada Public Health Association and APHA with faculty and there are networking opportunities which are promoted by faculty. Faculty attending these conferences will then also introduce them to their colleagues as well. In the last two years, faculty have arranged practice sessions for students giving presentations at professional meetings. These practice sessions are open to faculty and other students and much feedback is given to the presenter.
At our fall MPH Community Advisory Board meeting, we asked if members would be available for mentoring our students and they have agreed. This information will be shared with our students beginning with the capstone course meetings starting in October.
One of the purposes of our MPH Student Affairs Committee is also to support MPH students’ wellness. For example, our faculty has been great support for students who have cognitivelearning issues.
4.6.b. Description of the procedures by which students may communicate their concerns to program officials, including information about how these procedures are publicized and about the aggregate number of complaints submitted for each of the last three years.
See section 1.4.e.
4.6.c. Information about student satisfaction with advising and counseling services
In the past three years, there have been 3 requests by students to change advisors. This is a small percentage and is one indicator that there is satisfaction with the services provided. We also understand and support students in seeking out advising and career support from many sources beyond their advisor and beyond our walls.
Final Self Study, October 2010 Page 154
UNR School of Community Health Sciences
Each semester, the graduate assistants are surveyed confidentially about their relationships with their supervising faculty member. Results are reviewed by the graduate program director and the graduate committee. Aggregate feedback from the students is shared with all faculty who have served as supervisors.
The results from the MPH alumni survey (see Table 2.7.f.2.) demonstrate that all graduates from
2007-2008 who returned surveys rate the quality of advisement from fair to excellent. All 2008 alumni who returned surveys (the data for the most recent year available) rated the advisement quality as excellent. Interviews with all the MD/MPH students were conducted by the graduate program director at the end of their first year in the program and the students completed a evaluation of the program using Survey Monkey. The students were very satisfied with their experiences with faculty and in the classroom (2 of 3 rated their experience as “excellent”; the 3 rd as “good”). Although this feedback is encouraging, it must be noted that response rates for the alumni survey are low and there are a limited number of dual MD/MPH students.
4.6.d. Assessment of the extent to which this criterion is met.
This criterion is met.
Strengths
Faculty demonstrates strong commitment to student success.
Counseling and advisement are built into the program and students receive guidance and provide feedback at various points as they progress through program.
MPH Alumni are now in key management positions around the Northern Nevada area.
The MPH enjoys strong support from the College of Business Career Development
Center.
Many paths to advisement and career counseling are supported and encouraged.
Suggested Improvements
Website content about career opportunities should increase.
The program should conduct student surveys during their programs of study regarding satisfaction of advising services.
The program shold work to increase response rates from the alumni survey regarding advising and career counseling.
Final Self Study, October 2010 Page 155