peds review 3
advertisement

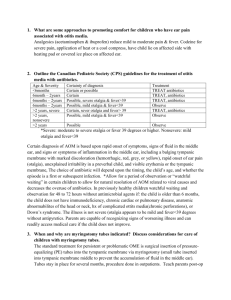
1. What are some approaches to promoting comfort for children who have ear pain associated with otitis media. Analgesics (acetaminophen & ibuprofen) reduce mild to moderate pain & fever. Codeine for severe pain, application of heat or a cool compress, have child lie on affected side with heating pad or covered ice place on affected ear. 2. Outline the Canadian Pediatric Society (CPS) guidelines for the treatment of otitis media with antibiotics. Age & Severity <6months 6month – 2years 6months – 2years 6months – 2years >2 years, severe >2 years, nonsevere >2 years Certainty of diagnosis Certain or possible Certain Possible, severe otalgia & fever>39 Possible, mild otalgia & fever<39 Certain, sever otalgia and fever> 39 Possible, mild otalgia & fever<39 Treatment TREAT antibiotics TREAT, antibiotics TREAT, antibiotics Observe TREAT, antibiotics Observe Possible Observe *Severe: moderate to severe otalgia or fever 39 degrees or higher. Nonsevere: mild otalgia and fever<39 Certain diagnosis of AOM is based upon rapid onset of symptoms, signs of fluid in the middle ear, and signs or symptoms of inflammation in the middle ear, including a bulging tympanic membrane with marked discoloration (hemorrhagic, red, grey, or yellow), rapid onset of ear pain (otalgia), unexplained irritability in a preverbal child, and visible erythemia or the tympanic membrane, The choice of antibiotic will depend upon the timing, the child’s age, and whether the episode is a first or subsequent infection. *Allow for a period of observation or “watchful waiting” in certain children to allow for natural resolution of AOM related to viral causes and decreases the overuse of antibiotics. In previously healthy children watchful waiting and observation for 48 to 72 hours without antimicrobial agents if: the child is older than 6 months, the child does not have immunodeficiency, chronic cardiac or pulmonary disease, anatomic abnormabilites of the head or neck, hx of complicated ottits media(chronic perforations), or Down’s syndrome. The illness is not severe (otalgia appears to be mild and fever<39 degrees without antipyretics. Parents are capable of recognizing signs of worsening illness and can readily access medical care if the child does not improve. 3. When and why are myringotomy tubes indicated? Discuss considerations for care of children with myringotomy tubes. The standard treatment for persistent or problematic OME is surgical insertion of pressureequalizing (PE) tubes into the tympantic membrane via myringotomy (small tube inserted into tympanic membrane middle to prevent the accumulation of fluid in the middle ear). Tubes stay in place for several months, procedure done in outpatients. Teach parents post-op to administer ear drops, avoid water entry into ears, wear earplugs while bathing/swimming. PE tubes allowing for adequate hearing & speech development but do not prevent middle ear infection. If infection occurs allow infected fluid to drain from ear, and contract doctor. 4. Differentiate b/w conductive, sensorineural, and mixed forms of hearing loss. Conductive hearing loss: transmissions of sound through the middle ear is disrupted, as with OME (otitis media with effusion), when fluid fills the middle ear, the tympanic membrane is unable to move properly, and partial or complete hearing loss occurs. Sensorineural hearing loss: cause by damage to the hair cells in the cochlea or along the auditory pathway. This may result from Mixed hearing loss: occur when the cause may be attributed to both conductive & sensorineural. 5. Name some causes of hearing loss in children and corresponding ways of reducing risk of hearing loss in children. Congenital hearing loss (1-6 infants/1000, ½ of all hearing impairments). Preterm infants and those with persistent pulmonary hypertension increased risk. Hearing loss common with congenital or genetic syndromes, & head/face anomalies. Newborn universal hearing screening laws allow for early identification of infants with congenital hearing loss. Delayed onset hearing loss: infection/fluid in middle ear (conductive), kernicterus, ototoxic medication, and intrauterine infection with CMA, or rubella, meningitis, neonatal respiratory depression, or exposure to excess noise(sensorineural). Regardless of the cause, early intervention influences child speech development. Earplugs or covers for prematures infants in NICU, hearing aids, cochlear implants, communication devices, speech education. 6. What are cochlear implants? How do they work? For what types of hearing loss are they indicated? Cochlear implants are surgically inserted electronic prosthetic devices for sensorineural hearing loss, a tiny receiver implanted in the body part behind the ear and connected to a microphone, minimum age 12 months. Respiratory disorders in children (Ateah text chapter 19) 1. Review anatomy and physiology of respiratory system. Newborns to infants (4-6weeks) breath through nose, cannot automatically open mouth to breathe if nose is obstructed, nares must be patent for successful feeding. Tongue is larger making airway obstruction more likely in unconscious child, airway d smallest at the cricoid in <8years, smaller, narrower airway make children more susceptible to airway obstruction, smaller lung capacity & underdeveloped intercostal muscles, infants and toddlers appear barrel-chested, children rely on diaphragm for breathing, lack of firm bony structure makes child more prone to retractions in respiratory distress, higher RR, and demand for O2 makes hypoxia easier to occur. 2. Review fetal development of lungs. Know physiology of “baby’s first breath” and transition from fetal/placental oxygenation to pulmonary respiration. 3. Know normal findings in RR across childhood : neonate (newborn), infant, toddler, preschooler, school-aged child, adolescent. Newborn - 6months 30 – 60/min 6 – 12 months 24 – 30/min 1 – 5 years 20 – 30/min 6 – 12 years 12 – 20/min 4. What are the signs of respiratory distress in infants and young children? tachypnea, inspiratory stridor, expiratory wheezes, barking, brassy coughing, supra/substernal or intercostal indrawing, nasal flaring, grunting, anxiety, restlessness, orthopnea(older child-can’t lie down), fatigue, exhaustion, CO2 retention, respiratory acidosis, Cyanosis circumorally (around the mouth) to central(midline, sign of hypoxia). For the following illnesses/disorders, understand the general incidence, causes/prevention, signs & symptoms, pathophysiology, medical/pharmacologic treatment options, and nursing considerations for: 5. Asthma: chronic inflammatory disorder of airways, primary case of school absenteeism, leading cause of child hospitalization, incidences are increasing, caused by genetic predisposition & environmental stimuli (smoke, smog, stress, mold/dust/dander allergens, upper respiratory infection). Inflammatory response of mast cells, eosinophils, & Tlymphocytes to stimuli caused accumulation of mucous and edema of airway, while spasm of bronchi/bronchioles decreases airflow. Symptoms: dyspnea, wheezing, coughing, decreased respiratory effectiveness leads to fatigue. Untreated can lead to barrel chest and elevated shoulders. Treatment involves chronic disease management, Peak expiratory flow meter, ongoing primary care provider. Inhalation corticosteroids, beta-adrenergic agonists (salbutamol/ventolin), MDIs. In emergency(severe respiratory distress, status asthmaticus)=ventolin mask, systemic corticosteroids, IV MgSO4 (smooth muscle relaxant) 6. Cystic Fibrosis: Inherited autosomal recessive trait (both parents carries=1:4 have CF, 2:4 carries), gene on long arm of chromosome 7. An exocrine gland dysfunction causing increased mucus secretion, obstruction of bronchi (airflow), sm. intestine(thick, sticky stool, pancreatic ducts(malabsorption), & bile ducts(biliary cirrhosis). Symptoms: large, bulky foul, frothy stools, or intestinal obstruction (meconium ileus in an infant), failure to pass stool, wt. loss, failure to grow, Vit. A, D, E, K deficiencies, respiratory wheezing, coughing, emphysema, atelectasis, frequent pneumonia. Progresses to barrel chest, clubbing & cyanosis. Chest PT several times a day, pancreatic digestive enzyme supplements, calorie/nutrient dense foods. Frequent hospitalizations for pneumonia. Defiance of treatments, sadness, & depression common with adolescents.