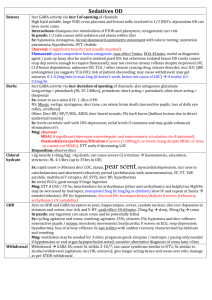
General toxicology fact sheet
advertisement

General Toxicology Mng Epidemiology Dangerous poisons In pregnancy In paeds 1. Resus Incidence 2%; 12.5% are symptomatic; 6-30% recurrence within 1yr 60% managed at home; >10% that come to hospital get admitted; 5% ICU; 20% general ward; 30% SSU; 45% discharged directly from ED 90% accidental, 10% intentional 60% >1 substance; 5% >3 substances; paracetamol in 15% ETOH present in 40% deaths 60% <5yrs (<12yrs in TinTin); peak 2-3yrs; accidental ingestion unusual >5yrs; lowest mortality 5-14yrs (40% drugs, 14% cleaning products, 13% plants, 10% cosmetics, 6% pesticides) 80% PO, 6% skin, 5% eye, 5% INH, 1% IV Leading cause of death <40yrs; <0.05% overall mortality; 90% deaths prior to any trt; 50% deaths are intentional; 1/3 hospital deaths due to PE; <1% mortality rate if admitted Resus can be assoc with good outcome even if prolonged CV: Ca channel blockers, beta-blockers, antiarrhythmics NS: TCA, cocaine Tox: paraquat, CO, OP, ETOH’s, acid/alkalis, cyanide, mushroom, HC’s, strychnine Other: chloroquine, colchicine, isoniazid, theophylline, metals Death despite good trt: paraquat, colchicine, OP, Ca channel blockers, beta blockers, antiarrhyhmic, cyanide, isoniazid, mushroom, theophylline Delayed toxicity: via bezoar / delayed gastric emptying / SR, EC / slow onset of action; paracetamol, theophylline, Ca blockers, opiates, Fe, Li, MAOI, anticonvulsants, dig, OP, amiodarone, oral hypoG, colchicine, warfarin, thyroxine Incr risk to fetus than mother in: CO, MetHb, lead, aspirin If fetus survives, risk of teratogenicity low; higher risk in 1st trim; charcoal safe 2 tabs can kill: amphetamines, Ca channel blockers, chloroquine, opioids, propanolol, sulfonylureas, theophylline, TCA (dothiepine) A sip can kill: OP’s, paraquat, HC’s, camphor, mothball 2 tabs is fine: paracetamol, Fe, colchicine, dig, rodenticide A: GCS not validated in poisoning; risk if GCS <12; may change quickly B C: give fluid bolus (large fluid resus may be needed in Fe, colchicine, theophylline, aspirin; beware pul oedema in Ca antagonist OD); may need inotrope Seizures: generalised; controlled with benzo’s (5-10mg diazepam (0.2mg/kg) rpt at necessary) phenobarb (100-300mg slow IV (10-20mg/kg) or thiopentone (3-5mg/kg); phenytoin CI’ed Most common causes: venlafaxine, buproprion, tramadol, amphetamines Signal of severe poisoning: chloroquine, propanolol, aspirin, theophylline, TCA HypoG: trt if BSL <4 50ml 50% dex (5ml/kg 10% dex) Most common causes: insulin, sulphonylurea, beta-blockers, quinine, chloroquine, salicylates, valproic acid Hyper / hypothermia: continuously measure core T if >38.5; emergent trt if T >39.5 Do emergency decontamination: paraquat, OP’s Give emergency antidote: digibind, calcium, cyanide 2. Risk assessment 3. Supportive care and monitoring 4. Investigations Agent (?dangerous one), dose (toxic dose is usually >10x therapeutic dose), formulation, route of exposure, time since ingestion, clinical features and progress, patient factors Consider drug combinations, tolerance Evaluate extent of toxicity, complications Establish reason for poisoning Causes of meiosis: opioids, cholinergics, olanzapine, clonidine, phenothiazines, barbs Causes of mydraisis: anticholinergics, stimulants Document: expected clinical course, potential complications, type of observation and monitoing, endpoints to consult doc, mng plans for agitation, criteria for changing mng, psychosocial risk assessment If coma, beware: aspiration, rhabdo, ARF, compartment syndrome, p area, hypoxic brain inj ECG; paracetamol (if non-detectable >1hr after ingestion = not significant) Drug levels helpful in: carbamazepine, phenobarb, valproic acid, phenytoin Dig ETOH, ethylene glycol, meth, CO, MetHb, paraquat (NOT cyanide – takes too long) Fe, lead, mercury, Li, arsenic methotrexate, paracetamol, aspirin, theophylline 5. Decontamination Osmolality = (2 x Na) + Ur + Glu Normal = 270-290 Osmolar gap = calculated – measured Normal -4 to +10 = amount of osmotically active substances in serum not measured by test Eg. Ca, Li, proteins (eg aa’s in ESRF), lipids, ETOH’s (normal OG does not exclude this if late presentation, as metabolised to less osmotically active substance), mannitol, acetone, formaldehyde, paraldehyde Use if: risk assessment predicts severe / life threatening toxicity, and supportive care / antidotes insufficient to ensure a satisfactory outcome; grounds to believe reasonable amount of agent remains unabsorbed and is amenable to removal In most agents, absorption complete within 1hr Pros: improved mortality and morbidity; more benign clinical course requiring decr level of care; decr need for hazardous / expensive interventions; decr hospital LOS Cons: aspiration; GI complications (eg. Perf, obstruction); distraction from resus / supportive care; diversion of departmental resources Induced emesis (Syrup of Ipecac): 90% V within 20mins 1st dose, 97% after 2nd dose; resolves in 2hrs Dose: 15-30ml with glass of water rpt at 30mins if no vomiting Indication: significant toxicity likely, no seizure / decr LOC risk, charcoal won’t work / not available, <1hr since ingestion; pill won’t fit into holes of NG tube eg. In remote areas CI: seizures, decr LOC, charcoal works, <1yr, corrosive / HC ingestion, rapid onset poisoning (eg. TCA), active/prior V Cons: interferes with charcoal administration, other therapeutic measures, 20mins delay; unreliable; Negligble effect by 1hr (decr absorption by up to 30% if given within 1hr); risks > benefits; no advantage over charcoal; prolonged vomiting (10-20%), diarrhoea (20-30%), lethargy (10%), pul aspiration, physical inj from vomiting Gastric lavage: Indication: as above; also in non-elemental mercury, arsenic, chloroquine, some HC’s Technique: lie on side, 20deg head down large bore NGT 200ml (10ml/kg) warm water drain rpt until clear effluent maybe put activated charcoal down at end CI: unprotected airway; small children; corrosive ingestion; oesophageal perf; pills that won’t fit into NGT Cons: unreliable; negligble by 1hr (25% if at 30mins, 10% if at 60mins); no advantage over charcoal; aspiration; hypoxia, laryngospasm; mechanical inj; water intoxication; hypothermia; perf Pros: immediately recovers gastric contents Single dose activated charcoal:; Doesn’t work in: alcohols, metals, acids / alkalis, OP’s, pesticides / petroleum products, ionic compounds (Li, arsenic, cyanide) Pathophysiology: adsorbs drug onto surface; 45% decr absorption if given after 30mins, 40% at 60mins, 15% at 120mins Dose: 25-50g in children (0.5-1g/kg if <1yr), 50-100g in adults PO / NG; ideally 10:1 CI: seizures, decr LOC; agent not bound; corrosive; bowel obstruction / perf Pros: more effective than above 2 if responsive substance; may absorb up to 50% product Cons: no good studies have shown benefit from this; vomiting (30%; unrelated to administration rate; prevented with antiemetics); aspiration (0.5%; potentially fatal); impaired absorption of antidotes; corneal Abrasion; decr OCP effectiveness; some preps contain propylene glycol; hyperNa (5%); hyperMg (3%); obstruction; messy Whole bowel irrigation: Indication: life threatening ingestion of SR/EC preps or Agents that don’t bind charcoal + good outcome not expected with supportive care and antidotes + patient presented before severe toxicity eg. Fe >60mg/kg, SR Li, lead, symptomatic arsenic SR KCl >2.5mmol/kg, Life threatening SR verapamil / diltiazem Body packers, pharmacobezoars Severe ingestion of other charcoal resistant substance Pathophysiology: PEG acts as osmotic agent and cleanses bowel rapidly; little net ion absorption / loss Technique: give charcoal patient seated or head of bed elevated to at least 45deg PEG via NG at 2L/hr (25ml/kg/hr infant, 0.5L/hr <6yrs, 1L/hr 6-12yrs) maxalon to control V, if sustained, decr inf rate by 50% for 30mins continue until effluent clear (may take up to 6hrs; stop if abdo distension / loss of bowel sounds) CI: uncooperative patient; can’t place NG; uncontrolled V; possibilty of decr LOC / seizure; ileus / obstruction; intubated (relative CI); GI haem; caution in infants and elderly; preceding diarrhoea Complications: N+V, NAGMA, aspiration, abdo cramps, rectal irritation Pros: no significant change in electrolytes / osm reported Cathartics: Pros: speed up GI transit Cons: osmotic effects may incr absorption; dehydration and LFT abnormalities in paeds Lipid partitioning therapy: Indication: LA’s, propanolol, TCA, verapamil; life-threatening OD of lipid-soluble drug where conventional trt failed Dose: 1ml/kg of 20% intralipid over 1min (max 100ml) rpt if needed 10ml/hr infusion Alternative: 400ml over 20mins 0.25ml/kg until stable Pathophysiology: acts as fluid compartment into which drug diffuses; good for high VOD, highly lipid soluble drugs CI: egg, soya, peanut allergy SE: shivers, N+V, fat overload syndrome (BM dep, hepatosplenomegaly, seizures), allergy, pul HTN, ALI 6. Enhanced elimination Others: wash skin Sorbitol: acts as osmotic laxative; can be given with charcoal but no evidence of improved efficacy; CI in preg, absent bowel sounds, obstruction / perf, ingestion of corrosive substance, vol depletion, significant electrolyte imbalance, <1yr, elderly; SE = incr absorption of some substances, decr BP, aspiration, N+V+D Indicated if: severe toxicity + poor outcome likely with supportive care / antidotes + slow endogenous rates of elimination or impaired method of distribution (and clearance can be increased by >30%) + suitable pharmacokinetic properties (small VOD) MDAC: Indication: substances that form bezoars, that slow GI fx, have entero-hepatic circn Effective: carbamazepine coma (most common indication) phenobarb coma (1st line) theophylline, phenytoin, aspirin, dapsone metHb, quinine, mushrooms Probably effective in: amitriptyline, dig, verapamil, sotalol Pathophysiology: interrupts entero-hepatic circ (works if entero-hepatic circ + small VOD); GI dialysis (works if small molecule, small VOD, low protein binding, long elimination HL, low endogenous clearance); may enhance elimination of substances even after absorption complete (by GI dialysis) Technique: 50g (1g/kg) PO 25g (0.5g/kg) Q2hrly (or 50g Q4hrly); check for bowel sounds before each dose and stop if gone; rarely required beyond 6hrs Endpoint: continue until improved condition / bloods CI: decr LOC, seizures, bowel obstruction Complications: V (30%); aspiration; constipation; bezoar formation obstruction, perf; corneal abrasion Urinary alkalinisation: Indication: phenobarb coma (2nd line; do if toxic despite MDAC) aspirin (do if symptomatic / mod severe, pH <7.1; if severe established toxicty, do haemodialysis) methotrexate Pathophysiology: drug must be filtered at glomerulus, small VOD, be weak acid, low pKa, mainly distributed in ECF, low protein binding, excreted renally in unchanged form; drug is ionised in alkaline urine excreted Technique: correct hypoK 1-2mmol/kg NaHCO3 IV bolus 10-100mmol NaHCO3 in 1L 5% dex at 250ml/hr; can add 20mmol KCl to infusion to prevent hypoK; check HCO3 and K Q4hrly; aim urine pH >7.5 and serum pH 7.5-7.55 Endpoint: continue until evidence toxicity is resolving CI: fluid overload, hypoK, renal failure Complications: alkaemia, hypoK, hypoCa, vol overload, pH shifts Haemodialysis / filtration: Indication: severe Li (>6mmol/L in acute, >2.5mmol/L in chronic) severe aspirin, theophylline, alcohols, metformin lactic acidosis, life threatening K, severe valproic acid, severe carbamazepine, phenobarb coma Other: amphetamines, camphor, chloral hydrate, metals Generally reserved for when other methods are failing and progressive end organ failure occuring, in ICU setting Doesn’t work for: Fe Pathophysiology: must be small molecule, small VOD, rapid resditrubtiuon from tissues and plasma, slow endogenous elimination, water soluble, low molecular weight, low protein binding, renal elimination, pKa less than serum pH Pros: corrects electrolyte abnormalities, can remove substances that don’t bind charcoal, removes substances already absorbed CI: CV instability, very small children, profound bleeding Complications: fluid shifts, electrolyte imbalances, infection and bleeding at catheter site, intracranial haem 7. Antidotes 8. Disposition NaHCO3 Use Charcoal haemoperfusion: superior to haemodialysis if charcoal adsorbs; can also do Fuller’s earth haemoperfusion in paraquat poisoning Indication: theophylline, paraquat, paracetamol, aspirin, carbamazepine, quinine, amanita, phenobarb, phenytoin Pathophysiology: agent must be lipophilic, adsorbed by charcoal, low protein binding Complications: requires systemic heparinisation; low plt, decr neuts, decr BP, blood loss, air embolic, hypoCa Required in <2% poisonings Admit SSU: ongoing cardiac monitoring not needed, adequate sedation achieved, clinical deterioration not expected; 4hrs observation provides medical clearance in 75% Pros: ready availability of appropriate staff, resources, training 24hrs; open plan environment for observation; ethos geared towards assessment and disposition; prevents self harm; dedicated SW; psych; monitors and telemtry; resus; duress alarms; nurse-pt ratio; tox concentrated in one area; security Admit ICU: airway control, ventilation, prolonged / invasive haemodynamic monitoring / support, haemodialysis A, B, C, sedation, seizure control, Glu, fluids, nutrition, pressure areas, thromboembolism prophylaxis, bladder care Other: psych, CYFS, SW, CADS Indication and dose: Hydrofluoric acid toxicity Correction of severe metabolic acidosis: 0.5mmol/kg for each desired incr in HCO3; endpoint HCO3 >8, clinical improvement of shock / dysrhythmias; incr pH to no greater than 7.2 HCO3 <3, pH <7.2, severe hyperchloraemic acidaemia Cyanide poisoning Isoniazid OD Ethylene glycol, methanol, other toxic alcohols Cardiotoxicity (arrest, VF/VT, hypoT) 2Y to fast Na channel blockade: repeated doses of 2mmol/kg IV until stability achieved 100mmol diluted in 1L N saline at 100-250ml/hr; aim pH 7.5-7.55; stop when no longer cardiotoxic; will likely need K supplementation TCA Type 1a and 1c antiarrhythmics: flecainide, quinidine, quinine Chloroquine / hydroxychloroquine Propanolol Urinary alkalinisation in OD enhanced elimination: 1-2mmol/kg IV bolus 100mmol in 1L 5% dex at 250ml/hr; add 20mmol KCl to infusion to maintain normal K; aim urinary pH >7.5 Salicylate – moderate severity not requiring haemodialysis (pH <7.1) Phenobarbitone – if continued toxicity despite MDAC Methotrexate Rhabo Prevention of drug redistribution to CNS – incr unionized amount of drug Salicylate SE: extravasation, gastric distension, hyperNa, hyperosmolality, vol overload, pul oedema, alkalosis (pH >7.6 bad for CV function), L shift of O2-Hb diss curve (impaired O2 unloading), hypoK, hypoCa (usually not clinically significant); incr lactate production; resp acidosis (ventilation must account for incr CO2 production) CI: hypoK, hypoCa, alkalosis, acute pul oedema, renal failure, severe hyperNa Notes from: Tox book, Dunn, TinTIn, Cameron