Procedural sedation fact sheet
advertisement
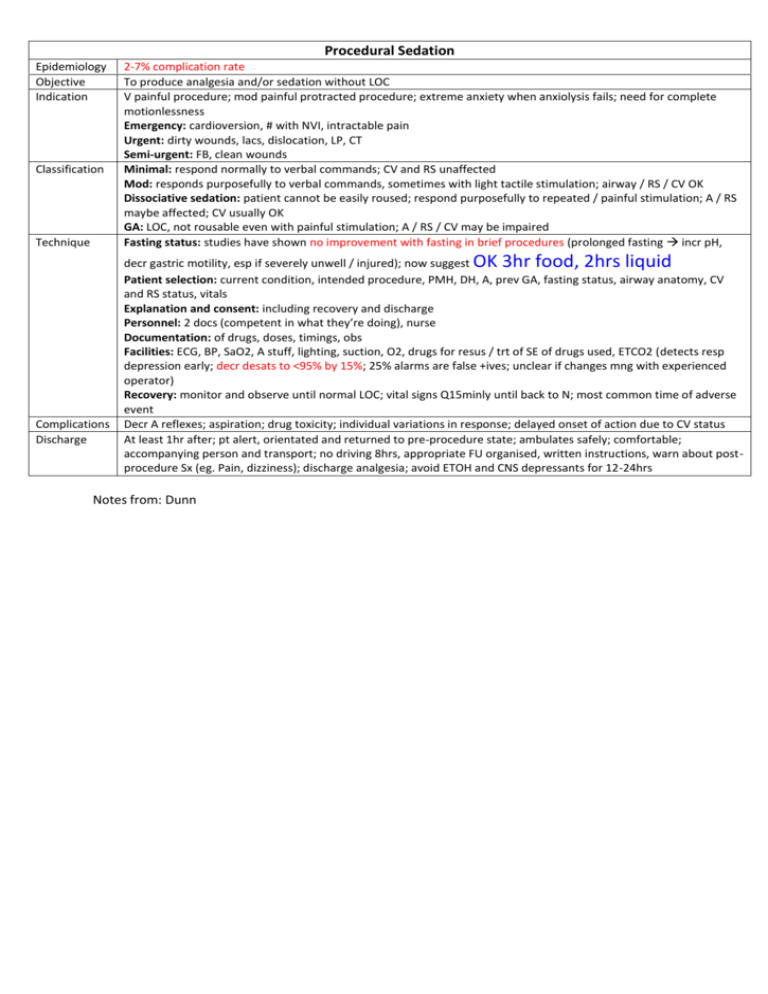
Procedural Sedation Epidemiology Objective Indication Classification Technique 2-7% complication rate To produce analgesia and/or sedation without LOC V painful procedure; mod painful protracted procedure; extreme anxiety when anxiolysis fails; need for complete motionlessness Emergency: cardioversion, # with NVI, intractable pain Urgent: dirty wounds, lacs, dislocation, LP, CT Semi-urgent: FB, clean wounds Minimal: respond normally to verbal commands; CV and RS unaffected Mod: responds purposefully to verbal commands, sometimes with light tactile stimulation; airway / RS / CV OK Dissociative sedation: patient cannot be easily roused; respond purposefully to repeated / painful stimulation; A / RS maybe affected; CV usually OK GA: LOC, not rousable even with painful stimulation; A / RS / CV may be impaired Fasting status: studies have shown no improvement with fasting in brief procedures (prolonged fasting incr pH, OK 3hr food, 2hrs liquid Complications Discharge decr gastric motility, esp if severely unwell / injured); now suggest Patient selection: current condition, intended procedure, PMH, DH, A, prev GA, fasting status, airway anatomy, CV and RS status, vitals Explanation and consent: including recovery and discharge Personnel: 2 docs (competent in what they’re doing), nurse Documentation: of drugs, doses, timings, obs Facilities: ECG, BP, SaO2, A stuff, lighting, suction, O2, drugs for resus / trt of SE of drugs used, ETCO2 (detects resp depression early; decr desats to <95% by 15%; 25% alarms are false +ives; unclear if changes mng with experienced operator) Recovery: monitor and observe until normal LOC; vital signs Q15minly until back to N; most common time of adverse event Decr A reflexes; aspiration; drug toxicity; individual variations in response; delayed onset of action due to CV status At least 1hr after; pt alert, orientated and returned to pre-procedure state; ambulates safely; comfortable; accompanying person and transport; no driving 8hrs, appropriate FU organised, written instructions, warn about postprocedure Sx (eg. Pain, dizziness); discharge analgesia; avoid ETOH and CNS depressants for 12-24hrs Notes from: Dunn tone