The Immune System - Body Defenses
advertisement

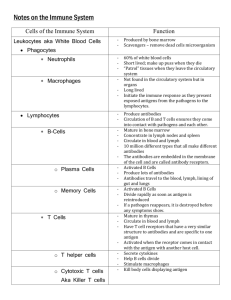
BIO2305 Immune System Body Defenses Reconnaissance, Recognition, and Response Must defend from the many dangerous pathogens it may encounter in the environment Detect invader/foreign cells Communicate alarm & recruit immune cells Suppress or destroy invader Two major kinds of defense have evolved that counter these threats Innate immunity and acquired immunity Innate Immunity Innate immunity provides broad defenses against infection Present before any exposure to pathogens and is effective from the time of birth Involves nonspecific responses to pathogens A pathogen that successfully breaks through an animal’s external defenses encounters several innate cellular and chemical mechanisms that impede its attack on the body Innate Immunity Non-selective No lag time – immediate response No previous exposure required Protects against infections, toxins Works with specific (acquired) immune response Acquired (Adaptive) Immune Response Depends on B and T lymphocytes Specific immune response directed attack against pathogens (antigen) Lag time Previous Antigen exposure required Protects against pathogens and cancer cells Types: Antibody-mediated Immunity (aka Humoral Immunity) B Lymphocytes (B cells) Cell-mediated immunity T Lymphocytes (T cells) 1 Types of Immunity Types of Immune Cells Body Defenses 2 Innate Immunity Physical barriers, secretions, chemical toxins Phagocytosis – macrophages, neutrophils engulf and digest recognized "foreign" cells, molecules Inflammatory response – localized tissue response to injury producing swelling, redness, heat, pain Natural Killer cells – special class of lymphocyte-like cells that destroy virus infected cells and cancer cells Complements system – activated proteins that destroy pathogen plasma membranes and enhance phagocytosis, inflammation Interferon – proteins that non-specifically defend against viral infection Innate Immunity/External Defenses Barriers - prevent entry of microorganisms and viruses Physical barriers Epidermis Mucous Membranes Hair, Cilia Excretions - lacrimal, saliva Chemical barriers Skin acidity between 3 and 5, which is acidic enough to prevent colonization Sebum toxic to microbes Lysozymes digests the cell walls of many bacteria Innate Immunity – Phagocytosis Functions: Scavenge dead and dying body cells, remove cellular debris Destroy abnormal cells (cancerous and virus-infected cells) Protect from pathogens & foreign molecules: parasites, bacteria, viruses Exhibit Margination – leukocyte adhesion to the inner endothelial lining of capillaries of affected tissue Move via Diapedesis – movement across capillary walls Exhibit Chemotaxis – concentration-dependent movement of a cell in response to the detection of chemokines Innate Immunity – Phagocytosis Monocyte - Macrophage System: vessel-bound, free, and fixed monocytes and macrophage that accumulate in lymph nodes, spleen, and lungs Monocytes: Macrophage-precursors that remain within vessels Macrophages: Monocytes that have left the body’s vessels Take longer to get to site of infection, but arrive in larger numbers Monocytes become free (roaming) macrophages, once they leave the capillaries Destroy microbes and clean up dead tissue following an infection 3 Innate Immunity – Phagocytosis Neutrophils Fastest response of all WBC to bacteria and parasites Direct actions against bacteria Release lysozymes which destroy/digest bacteria Release defensive proteins that act like antibiotics Release strong oxidants (bleach-like, strong chemicals) that destroy bacteria Eosinophils Leave capillaries to enter tissue fluid Attack parasitic worms Phagocytize antibody-antigen complexes Dendritic Cells a type of antigen presenting cells (with the broadest range) present in tissues in contact with the external environment Examples: Langerhans cells of the skin and follicular dendritic cells in the lymph nodes Phagocytic Cells Phagocytes attach to their prey via surface receptors and engulf them, forming a vacuole that fuses with a lysosome Phagocytosis Mechanisms Chemotaxis Attraction to certain chemical mediators Released at the site of damage Chemotaxins induce phagocytes to injury Opsonization Identify (mark) pathogen Coated with chemical mediators (antibodies, compliment proteins) Marked for death, and phagocytized by phagocyte Toll-like receptors (TLR’s) Phagocytic cells studded with plasma membrane receptor proteins Bind with pathogen markers Recognition - Allow phagocytes to “see” and distinguish from self-cells 4 Inflammatory Response Inflammation – histamine release from mast cells and other chemicals released from injured cells promote changes in blood vessels Changes allow more fluid, phagocytes, and antimicrobial proteins to enter tissues Effects of inflammation include Mobilization of local, regional, and systemic defenses Slow the spread of pathogens Temporary repair of injury Inflammatory Response Macrophages and Mast cells release histamine Localized vasodilation Capillary permeability - increased gaps in capillaries bring more WBC's & plasma proteins Swelling, redness, heat and pain are incidental Injured cells and phagocytes release cytokines (chemical signals) Kinins - stimulate complement system (plasma proteins) Chemotaxins – attract more phagocytes Clotting factors – walling off invasion 5 Natural Killer Cells Patrol the body and attack virus-infected body cells and cancer cells Recognize cell surface markers on foreign cells Destroy cells with foreign antigens Rotation of the Golgi toward the target cell and production of perforins Release of perforins by exocytosis Interaction of perforins causing cell lysis Natural Killer Cells Kill Cellular Targets Antimicrobial Proteins Proteins function in innate defense by attacking microbes directly or impeding their reproduction Complement System - About 30 proteins involved in the lysis of invading cells and helps trigger inflammation Interferons – small proteins provide innate defense against viruses and help activate macrophages 6 Complement System System of inactive proteins produced by liver circulating in blood and on cell membranes Cascade of plasma complement proteins activated by antibodies or antigens causing cascade of chemical reactions Direct effect is lysis of microorganisms by destroying target cell membranes Indirect effects include: Chemotaxis Opsonization Inflammation Recruit phagocytes, B & T lymphocytes Complement Activation 7 Innate Cytokines – Interferons Small antiviral proteins released by lymphocytes, macrophages, virally infected cells Type I interferons – Alpha and Beta Induced during many virus infections IFN- a: Mainly by leukocytes IFN- b: Mainly by fibroblast cells Binds to membranes of adjacent, uninfected cells Triggers production of proteins that interfere with viral replication Enhances macrophage, natural killer, and cytotoxic T cell & B cell activity Slows cell division and suppresses tumor growth Type II Interferon - gamma Activates macrophages and other immune cells 8 Integrated Defense Acquired Immunity In acquired immunity, lymphocytes provide specific defenses against infection Involves Cell mediated immunity Antibody mediated immunity 9 Acquired Immunity Antigen triggers an immune response Activates T cells and B cells T cells are activated after phagocytes exposed to antigen T cells attack the antigen and stimulate B cells Activated B cells mature and produce antibody Antibody attacks antigen Properties of Acquired Immunity Specificity – activated by and responds to a specific antigen Versatility – is ready to confront any antigen at any time Memory – “remembers” any antigen it has encountered Tolerance – responds to foreign substances but ignores normal tissues Lymphatic System Primary lymphatic organs – Bone marrow and Thymus Secondary lymphatic organs - Lymph nodes, Spleen Lymph nodes – Exchange Lymphocyte w/ lymph (remove, store, produce, add) Resident macrophages remove microbes and debris from lymph Lymphocytes produce antibodies and sensitized T cells released in lymph Spleen – Exchange Lymphocytes with blood, residents produce antibodies and sensitized T cells released in blood 10 Lymphocytes B and T cells originate in bone marrow B cells remain in bone marrow for maturation T cells leave bone marrow, and migrate to thymus gland for maturation 11 Lymphocytes – B and T cells B cells – Antibody-mediated immunity (grenade launchers) T cells – Cell-mediated immunity (hand-to-hand combat) Antigens An antigen is any foreign molecule that is specifically recognized by lymphocytes and elicits a response from them A lymphocyte actually recognizes and binds to just a small, accessible portion of the antigen called an epitope or antigenic determinant Antigenic determinants - Specific regions of a given antigen recognized by a lymphocyte Antigenic receptors -Surface of lymphocyte that combines with antigenic determinant Antigen Recognition by Lymphocytes A single B cell or T cell has about 100,000 identical antigen receptors All antigen receptors on a single cell recognize the same epitope 12 Cell-Mediated Immunity – T Cells Antigens that stimulate this response are mainly intracellular (cell to cell). Requires constant presence of antigen to remain effective Involves numerous cytokines, over 100 have been identified Stimulate and/or regulate immune responses Interleukins: Communication between WBCs Interferons: Protect against viral infections Chemotaxins: Attract WBCs to infected areas Lymphocyte Communication Over 18 different types of interleukins are known; designated IL-1, IL-2…IL-18, etc. IL-1 and IL-2 are primarily responsible for activating T and B lymphocytes, with IL-2 being a stimulant of T- and B-cell growth and maturation IL-1, along with IL-6, is also a mediator of inflammation. IL-4 often leads to an increase in antibody secretion by B lymphocytes IL-12 causes a greater number of the leukocytes cytotoxic T cells and natural killer cells to be made The set of interleukins produced by the presence of a specific infectious agent determines which cells will respond to the infection Types of T cells Cytotoxic T cells – attack foreign cells Helper T cells - activate other T cells and B cells Suppressor T cells– inhibit the activation of T and B cells Memory T cells – function during a second exposure to antigen T cell membranes contain CD markers: CD3 markers present on all T cells CD8 markers on cytotoxic and suppressor T cells CD4 markers on helper T cells T Cell Activation T cells are activated when they detect and bind to small fragments of antigens that are combined with to cell-surface glycoproteins called major histocompatibility complex (MHC) molecules Lymphocytes respond to antigens bound to either class I or class II MHC proteins depending on the source of the MHC molecule and the antigen presenting cell Class I MHC molecules are displayed on the surface of infected nucleated cells Class II MHC molecules are displayed on the surface of phagocytes Class I MHC molecules Infected cells produce Class I MHC molecules which bind to antigen fragments and then are transported to the cell surface in a process called antigen presentation Binds and activates with Cytotoxic T cell receptor Cytotoxic T cell response: Clonal production of cytotoxic T cells and memory cells Destruction of virus-infected cells, tumor cells, and tissue transplants 13 Cytotoxic T (TC) Cells – CD8 Recognize and destroy host cells that are infected with viruses or bacteria, cancer cells, transplanted tissue Release protein called perforin which forms a pore in target cell, causing lysis of infected cells. Produce cytokines, which promote phagocytosis and inflammation Undergo apoptosis when stimulating antigen is gone. Class II MHC molecules Produced by dendritic cells, macrophages, and B cells Macrophages & dendritic cells phagocytize antigens, proteins broken down into antigen fragments (peptides) and combined with Class II MHC molecules Binds and activates Helper T cells Clonal production of Helper T cells Activation of Cytotoxic T cells Activation of B cells T Helper (TH) Cells – CD4 T Helper (TH) Cells: main role in immune response Recognize antigen on the surface of antigen presenting cells Secrete Interleukin II (T-cell growth factor), interferon and cytokines which stimulate lymphocyte activity Production and activation of Cytotoxic T cells and more Helper T cells Stimulate B cells to produce antibodies 14 T Cell Overview Memory T-Cells Can survive a long time and give lifelong immunity from infection Can stimulate memory B-cells to produce antibodies Can trigger production of killer T cells Thymosin - hormone important in T cell lineage, enhances capabilities of existing T cells and the proliferation of new T cells in lymphoid tissues - decreases after age 30-40 15 Proliferation of Lymphocytes Antibody-Mediated (Humoral) Immunity Involves production of antibodies against foreign antigens Plasma cells - B cells that are stimulated and begin actively secrete antibodies Antibodies (immunoglobulins, Ig) are Y-shaped proteins found in extracellular fluids (blood plasma, lymph, mucus, etc.) and the surface of B cells Defend against bacteria, bacterial toxins, and viruses that circulate freely in body fluids, before they enter cells Also cause certain reactions against transplanted tissue Antibody-Mediated (Humoral) Immunity 1000s of different B cells, each recognizes a different antigen on the surface of a macrophage (specificity) Each antigen stimulates production of a single specific antibody that the B cells (along with T cells) come in contact with They are stimulated (by TH cells) to produce many clones, plasma cells, which make antibodies. Memory B cells provide secondary response (faster, more sensitive) 16 Antibody Structure Antibodies or Immunoglobulins (Ig) Classes: IgG, IgM, IgA, IgE, IgD Structure Variable region - combines with anitgenic determinant of antigen Constant region - responsible for other binding activities Consequences of Antigen-Antibody Binding Agglutination - antibodies cause antigens (microbes) to clump together Opsonization and Phagocytosis – coating foreign substance with antibodies, allowing Phagocytes to grip and engulf the invader Complement System / Inflammatory Response – lyse the invader and attract other immune cells (chemotaxis) Neutralization – coat foreign substance, rendering it harmless Antibody dependent NK/eosinophil cell response – Directly attack and lyse the cell using perforins 17 Consequences of Antigen-Antibody Binding Antigen-Antibody Complex On B Cell Activate B lymphocyte production of: Memory B cells for secondary immune response to that antigen Active Plasma Cells that secrete antibodiess Immunoglobulin Classes IgG Percentage serum antibodies: 80% Location: Blood, lymph, intestine, Only lg that crosses placenta, thus conferring passive immunity on fetus Promotes opsonization, neutralization, and agglutination of antigens, protects fetus and newborn. IgA Percentage serum antibodies: 10-15% Location: Secretions (tears, saliva, intestine, breast milk), blood and lymph Provides localized defense of mucous membranes by agglutination and neutralization of antigens Localized protection of mucosal surfaces. Presence in breast milk confers passive immunity on nursing infant IgM Percentage serum antibodies: 5-10% Location: Blood, lymph, B cell surface (monomer) First antibodies produced during an infection. Effective against microbes, complement activation and agglutinating antigens 18 IgD Percentage serum antibodies: 0.2% Location: Found primarily on surface of naive B cells that have not been exposed to antigens Acts as antigen receptor in antigen-stimulated proliferation and differentiation of B cells (clonal selection) IgE Percentage serum antibodies: 0.002% Location: Bound to mast cells and basophils throughout body Triggers release of histamine and other chemicals that cause allergic reactions B Cell Sensitization And Activation Sensitization – the binding of antigens to the B cell membrane antibodies Activation - Helper T cells present same antigen to stimulate B cell Division - Stimulated B cells divide into many clones called plasma cells, which actively secrete antibodies Secretion - Each B cell secrete antibodies that will recognize only one antigenic determinant Differentiation - Active B cells also differentiate into Memory B Cells 19 Immunological Memory Primary Response: After initial exposure to antigen, no antibodies are found in serum for several days. A gradual increase number of Abs, first of IgM and then of IgG is observed. Most B cells become plasma cells, but some B cells become long living memory cells. Gradual decline of antibodies follows. Secondary Response: Subsequent exposure to the same antigen displays a faster/more intense response due to the existence of memory cells, which rapidly produce plasma cells upon antigen stimulation Clonal Selection Clonal Selection: B cells (and T cells) that encounter stimulating antigen will proliferate into a large group of cells. Why don’t we produce antibodies against our own antigens? We have developed tolerance to them. Tolerance: To prevent the immune system from responding to self-antigens Clonal Deletion: B and T cells that react against self antigens are normally destroyed during fetal development Preventing activation of lymphocytes – activate Suppressor T cells, control the immune system when the antigen / pathogen has been destroyed Apoptosis Apoptosis - Programmed cell death (“Falling away”) Human body makes 100 million lymphocytes every day. If an equivalent number doesn’t die, will develop leukemia B cells that do not encounter stimulating antigen will self-destruct and send signals to phagocytes to dispose of their remains Many virus infected cells will undergo apoptosis, to help prevent spread of the infection Autoimmune Diseases: Failure of “Self-Tolerance” Some diabetes mellitus – attack - cells Multiple sclerosis – attack on myelin nerve sheath Rheumatoid arthritis – attack joint cartilage Myasthenia gravis – ACh-receptors at endplate attacked 20 Allergic Response: Inflammation Reaction to Non-pathogen First exposure: sensitization Activation Clone B cells Form antibodies Memory cells Re-exposure Many antibodies Activated T cells Intensified Inflammation Hemagglutination Agglutination of red blood cells used to determine ABO blood types and to detect influenza and measles viruses 21 Summary Body defends itself with barriers, chemicals & immune responses WBCs and relatives conduct direct cellular attack: phagocytosis, activated NK & cytotoxic T cells and produce attack proteins (i.e. antibodies, complement, & membrane attack complex) Cytokines, communicate cell activation, recruitment, swelling, pain, & fever in the inflammation response Defense against bacteria is mostly innate while viral defense relies more on acquired immune responses Autoimmune diseases are a failure of self-tolerance 22