National Cancer Programme Update: July 2014
advertisement

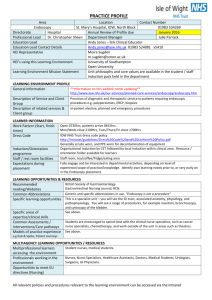
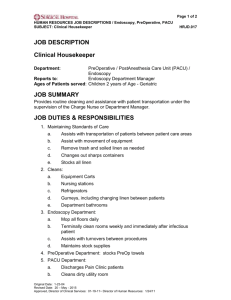
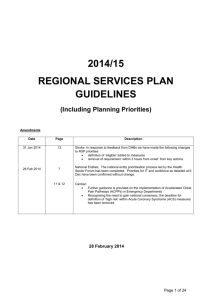
National Cancer Programme Update: July 2014 Welcome to the latest edition of our National Cancer Programme Update. We will send you a new update every few months to keep you informed about key areas of our work programme. Please forward this update to colleagues who you think may find it useful. If you don’t want to receive these updates, please reply to this email with “unsubscribe” in the subject line. Progressing the role of nurses in endoscopy An advisory group has been established to develop and implement the role of nurses in endoscopy. The move follows on from the Endoscopy Workforce Symposium hosted by the Ministry and Health Workforce New Zealand in April 2014. The advisory group will organise for the first nurses performing endoscopies to be in training in a small number of district health boards by early 2015. It will ensure trainees are well supported and have the right education and training needed to perform the role in a safe and effective manner. Development of the nurse role in endoscopy procedures will be considered in the wider context of developing advanced nurse roles that contribute to the career pathway for nurses. Nurses working in gastroenterology, and more specifically endoscopy, are expected to have a positive influence on service delivery and enable medical staff to be released to undertake more complex procedures. The role of nurses performing endoscopy is not proposed as a substitute for the role of gastroenterologists and general surgeons. Development of the nurse role in performing endoscopy, as well as an increase in the number of registrars training in gastroenterology and general surgery, are a critical part of delivering bowel screening in New Zealand. It is expected that endoscopy training for nurses, gastroenterologists, and general surgeons will be subject to identical standards and, expectations and that there will be common governance of the training available to all three groups. Bowel screening pilot first round results New data shows that more than 164 people who have taken part in the Waitemata bowel screening programme have been found to have cancer. Provisional results for the first two years of the programme (January 2012 to December 2013) show most of the cancers were found at an early stage, when they can often be cured. More than 67,500 people completed a bowel screening test and more than 4300 people with a positive result went on to have a colonoscopy through the programme. At the end of the first two year screening round, almost 54 percent of people who were invited to take part in the programme had returned a completed test. The data for the first two years is helping to build a picture of how a national bowel screening programme could be implemented and what would need to be in place to do that safely and equitably. More than 40,000 publicly funded colonoscopies are performed each year, but every year this number falls short of demand. This shortfall will increase if there is a national bowel screening programme. In 2013, $3.6 million was made available so district health boards (DHBs) could deliver additional colonoscopies, and this was followed by a further $8 million in Budget 2014 to help improve waiting times. Work is also underway to boost the endoscopy workforce. The four-year $24 million bowel screening pilot in the Waitemata DHB area will run until December 2015. Endoscopy Knowledge and Skills Framework packages A series of Directly Observed Practical Skills (DOPS) packages for endoscopy nurses has been developed as part of the ongoing work around the Endoscopy Knowledge and Skills Framework. The DOPS packages are designed to provide a consistent structure to the assessment of endoscopy nursing skills throughout New Zealand. They provide a framework for what is already being done in many units and reduce the variation in the quality of endoscopy nursing that was highlighted in the 2010 National Summary Report on endoscopy services. The lower gastrointestinal (GI) and endoscopic retrograde cholangiopancretogaphy (ERCP) DOPS have been available to the sector since early 2014. They are supported by the National Endoscopy Quality Improvement Programme (NEQIP) Nursing Workforce Development leads Gendy Bradford and Anne Cleland. The upper GI and pre and post procedure packages are in the final stages of development and will be available to the sector in September 2014. Contact: Jenni Masters, NEQIP Sector Implementation Director jenni.masters@bopdhb.govt.nz Service improvement initiatives underway More than 20 initiatives funded as part of the faster cancer treatment Service Improvement Fund (SIF) will be underway by the end of August 2014. These include a project to improve the cancer care pathway for Mâori patients in the Nelson Marlborough district, improvements to the lung and urology cancer patient pathway at Taranaki DHB, and a project across Capital and Coast, Hutt Valley and Wairarapa DHBs to establish an ambulatory model of care for all areas of service including medical oncology, haematology, transfusions and radiation treatment. A full list of SIF initiatives will be released once all contracts are finalised. Service improvement initiatives are also considering the long term impact that any change made may have on other services such as radiology. In addition to the SIF initiatives, a National Radiology Service Improvement Initiative is currently underway across the country to support CT and MRI waiting times. National Health Board National Clinical Lead, Radiology, Kim McAnulty says the improvements resulting from the initiative are expected to extend across all radiology service activities. These will include decreased waiting times in radiology services, increased patient access, and reduced waste and inefficiency. Improving waiting times for diagnostics can reduce delays for patients and improve DHB demand and capacity management. Cancer nurse coordinator forum This year’s cancer nurse coordinator (CNC) forum provided an opportunity for CNCs from around the country to focus on how these roles have developed over the last year. Nurses attending the second national CNC forum in Wellington in June 2014 heard that early evaluation data shows both patients and providers have a good understanding of the CNC role. Independent evaluators Litmus Limited took the opportunity to thank nurses for their efforts to support the evaluation and stressed the importance of having full data sets so the full story of how care coordination contributes to patient care can be told. Early evaluation data tells a promising story about how well the role is being defined and developed in district health boards around the country. The evaluation, which began in February 2013, will run until 2015. Some early evaluation data from surveys of patients, CNCs and health professionals that provide cancer care is expected to be available later this year. A final report will be published in 2016. More funding for cancer consumer representation Further Ministry funding will allow the Central Cancer Network (CCN) to continue providing overall coordination of the cancer consumer representative programme. The programme provides the infrastructure to support consumer representation across the four regional cancer networks, including coordinating and providing secretariat support for the National Cancer Consumer Representatives Advisory Group. It also provides regional cancer networks with an annual budget to support cancer consumer representative training, support and development. Supportive care services Budget 2014 delivered funding to improve psychological and social support for people with cancer. The funding will be used to establish supportive care services throughout the country to ensure the emotional and psychological needs of cancer patients are properly assessed and patients and families receive the support they need. Up to 20 cancer supportive care key workers will be employed in hospitals to provide counselling and assistance for patients. The key workers will deliver evidence-based supportive care for patients with low and medium level supportive care needs, and will refer patients to clinical psychologists where appropriate. Clinical psychologists will be funded for the six cancer centres. They will deliver treatments for cancer induced psychological distress and will lead the development of regional referral pathways. A national lead role will be established to provide overall guidance and professional support. The national lead role will support development of training standards for supportive care health professionals, provide leadership and supervision for the support workers and develop tools that assess patient distress. In 2014/15 the Ministry of Health will focus on: recruiting to the national lead role position to oversee the development and implementation of the supportive care programme working with DHBs and sector experts to scope job descriptions for the supportive care key worker role (including how this role aligns with the existing work force) undertaking an analysis of the specialist psychologist workforce capacity. The Ministry expects DHBs to be able to access funding so they can begin recruitment to the new sector roles in 2015/16. Cancer information strategy Our ability to improve patient outcomes and quality of health care is dependent on timely, accurate and easily accessible information. Clinicians, researchers and health planners are calling for improved cancer information collection and reporting systems. The sector has asked for a Cancer Information Strategy to support better alignment of activities in cancer information and ensure everyone is working towards a common vision. Over the years there have been a number of attempts to achieve a cohesive vision for cancer information, including the Cancer Collections Framework Project, published in 2006. The framework defined a five year strategic ‘roadmap’ for the development of cancer information, but has not been fully implemented. During 2014/15 the Ministry’s Cancer Services team intends to develop a cancer information strategy, with significant input from a wide range of stakeholders. The strategy will be agreed by the Cancer Programme Steering Group and the IT Health Board. Enhancing quality care through clinical decision making and monitoring In New Zealand, there is an acknowledged lack of understanding about what contributes to variation in access to services, and differences in the quality of services that lead to inequalities in cancer outcomes. There are key measures from the assessment, diagnosis and treatment of patients with cancer that can provide data to inform ongoing quality improvement activities. Clinicians are keen to have this data routinely collected and analysed to help with clinical decision making and quality improvement. This includes collecting data on adverse outcomes and overall patient outcomes. Tumour specific core data sets will be developed in 2014/15 which, once implemented, will enable consistent collection of information that will allow comparisons to be made between services and district health boards. In 2014/15 the Ministry will work with DHBs to identify the best way to: develop tools to support data capture (most likely as part of multidisciplinary meetings (MDMs)) to support and inform clinical practice and support standardisation of patient care develop regional information repositories of MDM data (using the tumour-specific core data set) that can be linked nationally to inform quality improvement and support implementation/monitoring of tumour standards care. This funding will be distributed to DHBs via a Crown Funding Agreement variation in 2015/16. The Ministry will provide DHBs with more detail on this funding in late October 2014. Update on review of services against tumour standards DHBs in the Central Cancer Network region have identified bowel, lung, gynaecological and breast as the priority tumour standards for review over the next 18 months. The data gathering phase for the review against the bowel standards has been completed and the Central Regional Faster Cancer Treatment Steering Group has begun reviewing the information before making recommendations for service improvements. Planning for the lung review is now underway. The Midland Cancer Network has prioritised and agreed the order of the regional DHB reviews against the standards. A review against the national lung cancer standards has been completed and an implementation plan for each recommendation is being developed. A review against the national bowel cancer standards is now in progress. The focus will then turn to gynae-oncology, breast cancer and consistent themes of supportive care in 2014/15. The Midland and Northern networks have agreed to work together on the regional review of gynae-oncology standards. In the Northern region, initial work on head/neck and sarcoma (conducted in 2013/14) will continue into the next financial year, subject to agreement through regional strategic planning processes. The 2014/15 reviews will include head/neck and bowel, consistent with the national working group process. More funding for cancer information network The Ministry has provided another year of funding for the Cancer Society to continue to coordinate and implement the Cancer Information Network (CINNZ) work programme. The funding will allow for completion of an up-to-date register of cancer-related resources that will eventually be accessible to the public. It will also be used to develop a cancerrelated dictionary/glossary of terms in multi-media formats. Planning radiation oncology services for the future New Zealand's first dedicated national radiation oncology plan has been released to help DHBs plan their future radiation oncology service and capacity needs through until 2022. The Radiation Oncology National Linear Accelerator and Workforce Plan (the Plan) will help ensure there is the cancer workforce and equipment to treat the country's growing and ageing population The Plan will be updated regularly so it remains a relevant planning tool for the sector. It can be downloaded from the Ministry of Health website. The Plan looks at the projected growth in cancer numbers, its implications for linear accelerators (the equipment used to deliver radiation therapy), the number of radiation oncologists, medical physicists and radiation therapists needed, along with the cost. It provides a range of scenarios, which will enable DHBs to assess the needs of their populations and make decisions around how best to provide radiation treatment at both a local and regional level in future. The Plan builds on initial capacity planning of radiation therapy services published in 2012 by the regional cancer networks. It provides national guidance and a tool - the National Linear Accelerator and Workforce Capacity Model - to project national capacity requirements for a range of future scenarios. As the model is a complex Excel Workbook, the Ministry will provide DHBs with help desk support to assist users. Issues likely to arise include: queries regarding use and functionality of the Model different versions of Excel and local IT system idiosyncrasies clarifying Model methodology issues and scenarios clarifying data issues – attendances, cancer registrations, registration forecasts. Specific details on how to access the model and support will be provided to DHBs shortly.