regional services plan guidelines
advertisement
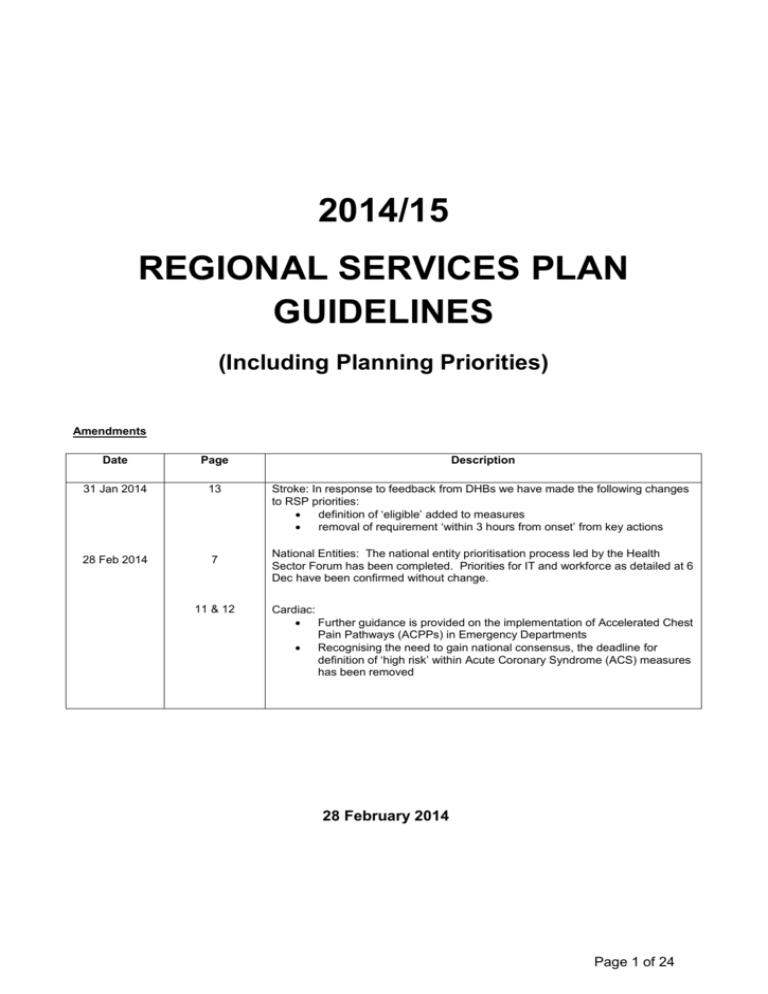
2014/15 REGIONAL SERVICES PLAN GUIDELINES (Including Planning Priorities) Amendments Date Page Description 31 Jan 2014 13 Stroke: In response to feedback from DHBs we have made the following changes to RSP priorities: definition of ‘eligible’ added to measures removal of requirement ‘within 3 hours from onset’ from key actions 28 Feb 2014 7 11 & 12 National Entities: The national entity prioritisation process led by the Health Sector Forum has been completed. Priorities for IT and workforce as detailed at 6 Dec have been confirmed without change. Cardiac: Further guidance is provided on the implementation of Accelerated Chest Pain Pathways (ACPPs) in Emergency Departments Recognising the need to gain national consensus, the deadline for definition of ‘high risk’ within Acute Coronary Syndrome (ACS) measures has been removed 28 February 2014 Page 1 of 24 CONTENTS FOR REGIONAL SERVICES PLAN GUIDANCE TOOLKIT 1. Introduction 2. Regional Services Plan Priorities 2.1. Health Of Older People as a Required Priority 2.2. Major Trauma as a New Priority 2.3. Enablers 2.3.1. Regional and National Information Technology 2.3.2. Regional Workforce 2.3.3. Capital 2.4. Sub-Regional Initiatives 3. Regional Governance and Leadership 3.1. Regional Governance and Decision Making 3.2. Supporting Clinical Networks and Clinical Leadership 4. Strategic Position 5. Line of Sight across RSPs and APs 5.1. The planning process across Regional and Annual Plans 5.2. Linkages with Māori Health Plan 6. National Entities 6.1. Health Quality and Safety Commission 6.2. National Health Committee Appendix One: 2014/15 Regional Services Plan Priorities Appendix Two: Line of Sight – worked examples For further information please contact: Karina Kwai – Manager, Planning National Health Board, Ministry of Health. Contact details: Mobile 027 229 0902 DDI 04 816 3318 Email Karina_Kwai@moh.govt.nz Page 2 of 24 1. Introduction DHBs are expected to work together at a regional level to make the best use of available resources, strengthen clinical and financial sustainability and increase access to services. Improving regional collaboration between District Health Boards (DHBs) has been an evolving process over time. In the last few years, significant progress has been made in establishing the key foundations to assist regional working and DHBs are in a good position to continue implementing their regional and sub-regional priorities. The purpose of a Regional Services Plan (RSP) is to provide a mechanism for DHBs to document their regional collaboration efforts and align service and capacity planning in a deliberate way. The RSPs include national and local regional priorities, and outline how DHBs intend to plan, fund and implement these services at a regional or sub-regional level. The plans have a specific focus on reducing service vulnerability, reducing costs and improving the quality of care to patients. In 2014/15, the visibility of contributions by DHBs to achieve regional service priorities has been strengthened with a Line of Sight guidance framework. The framework has been introduced to encourage greater alignment between Annual Plans (AP) and RSPs, and to allow DHBs to demonstrate how individual DHBs contribute to achieving regional objectives. 2. Regional Services Plan Priorities The 2014/15 RSP priorities are noted below. These are mostly a continuation from 2013/14 with the exceptions of Health of Older People (which is now a required priority) and Major Trauma as a new priority. 1. 2. 3. 4. 5. 6. 7. 8. 9. Elective Services Cancer Services Cardiac Services Mental Health and Addictions Stroke Services Health of Older People Major Trauma Information Technology Workforce DHBs are to include additional priority services which are appropriate for their region. 2.1 Health of Older People as a Required Priority Improving services for people with dementia is a priority area for DHBs and regions in 2014/15. In November 2013, the Government launched the "New Zealand Framework for Dementia Care". Regions are expected to develop and implement components of their dementia care pathways at the regional level. Regions are to achieve this by working with the sector (e.g. primary health care, community support groups) and supporting the implementation of DHB dementia care pathways through shared learning and resources. Regions are expected to develop and commence delivery of dementia awareness and responsiveness education programmes for primary health care clinicians to improve the timeliness for dementia diagnosis in 2014/15. Page 3 of 24 2.2 Major Trauma as a New Priority There is clear international evidence that regional major trauma systems can reduce the number of deaths, disability levels, improve patient outcomes and satisfaction levels. In 2010, the National Health Board (NHB) undertook a service review of major trauma care which highlighted variable service quality and patient outcomes in New Zealand. The initial focus for major trauma is to develop and implement regional major trauma systems nationally. DHBs are expected to produce a three year plan on establishment of the local and regional major trauma systems and implement a process to collect data for a national minimum data set to contribute to a National Trauma Registry by 1 July 2015. 2.3 Enablers The National Health IT Plan and Health Workforce Regional Work Plan outline the strategic focus for these areas, and include key priorities and programmes which are expected to be implemented regionally by DHBs. The regional priorities for 2014/15 for Information Technology (IT) and Workforce are outlined in Appendix One and the requirements for enablers can be incorporated into specific service priorities where applicable. Further context on how these enablers link with regional objectives in RSPs is noted below. 2.3.1 Regional and National Information Technology IT provides the platform to support improved information sharing and integrated healthcare. The priority national initiatives such as cardiac, cancer and elective services are underpinned by national information platforms. Well-designed IT solutions help us work smarter to reduce costs, improve efficiency and give patients better, safer treatment. The National Health IT Plan Update refines the focus areas, ranks the priorities, and sets out the key performance indicators and action plan for success. Key risk mitigations for IT delivery rely on strong regional governance and decision making, security of systems and moving from tactical to strategic IT delivery. Regions should include their prioritised three year plan of all local, regional and national IT initiatives, including the applicable critical priorities listed in Appendix One. The following level of information should be provided for each initiative: 2.3.2 Description of the initiative Budget allocation by DHB Benefits, enablers and actions, milestones and measures Regional Workforce More standardised ways of delivering services are needed to meet increased demand for services. This will release resources for use elsewhere and build a platform to develop a workforce with more generic skills that is flexible and able to work in integrated service models across hospital and community settings. Regionally, DHBs are expected to continue to work with the Regional Training Director and build on the workforce section of the 2013/14 RSP demonstrating further progress on actions they are undertaking to meet key milestones. Key milestones for 2014/15 are outlined in Appendix One. 2.3.3 Capital Regional services planning remains an integral part of capital investment planning. Where it is appropriate, potential capital impacts should be identified. However, quarterly reporting on capital Page 4 of 24 will not be required via RSPs. In 2014/15, the NHB will collect the regional capital plans separately. The NHB considers a separate process will reduce administrative workload for DHBs and focus DHBs on regional capital planning. 2.4 Sub-Regional Initiatives Current and emerging sub-regional initiatives where DHBs are working together to provide improved value to their populations should be identified in the RSP. Measurable and time bound actions are required to be set out in the AP (Annual Plan Toolkit, Module 2: Delivering on Priorities and Targets). 3. Regional Governance and Leadership DHBs are expected to continue to provide effective regional governance, accountability and decision making. All DHB Chairs and Chief Executives from each region will be required to agree and sign RSPs on behalf of their individual boards. 3.1 Regional Governance and Decision Making RSPs should provide information about how implementation will be governed, costed, funded and managed, including how DHBs will manage performance. Information may include: roles and responsibilities, an outline of arrangements to provide support and assistance to other DHBs to meet the regional and/or sub-regional performance expectations, and how barriers and issues will be resolved. Some regional (including sub-regional) work programmes may require specific governance and leadership approaches with tailored membership to appropriately represent the key stakeholders and to ensure the best outcome is achieved (e.g. involvement and alignment with primary care, NGOs, patient representative groups). DHBs may also wish to include other examples of regional collaboration, for example, crossappointed board members and clinicians and regular engagement between DHB boards in the region. DHBs are expected to assist their colleagues in finding and implementing solutions to financial or clinical issues which arise. This may include making staff with expertise available to work with the National Health Board to resolve the issue. An indication of how the region will arrange this should be included. 3.2 Supporting Clinical Networks and Clinical Leadership In the 2013/14 year, both nationally and regionally, clinicians had a positive influence in regional decision making processes. In 2014/15, it is expected that clinical integration will continue to be visible in the development of service priorities. RSPs are to adopt a proactive approach to strengthening clinical integration by developing and supporting clinical networks. In particular, the RSPs are to: Identify how the region can work with clinical leaders to make better use of clinical networks to support improved clinical and financial sustainability of services; and Identify services within the region that may benefit from the development of a regional clinical network. Page 5 of 24 4. Strategic Position In the development of the strategic section, regions should reflect on progress to date, identifying and explaining any significant changes from earlier years, and identifying the direction of travel for 2014/15 and future years. The strategic section of the RSP should also be consistent with national strategic imperatives, as well as all trends and key outcomes outlined in: the DHB’s Statement of Intent (SOI) that articulates the ability of each DHB in the region to deliver improved services into the future; and the Strategic Intentions section of the DHB’s AP where each DHB examines how health services can be most effectively and efficiently coordinated and delivered. 5. Line of Sight across RSPs and APs The focus of 2014/15 is to ensure that there is greater alignment between RSPs and APs. The RSPs are expected to set out the regional priorities and how DHBs intend to work as a region to achieve these. The requirements of IT, workforce and capital to implement service priorities are also expected to be incorporated where applicable. 5.1 The planning process across Regional and Annual Plans A Line of Sight guidance framework is provided below to improve linkages across RSPs and APs and to demonstrate how individual DHB actions contribute to achieving regional priorities. The Line of Sight framework outlines common objectives, actions, milestones, costs and measures for regional service priorities. It also provides guidance on inputs, resources, roles and responsibilities. Individual contributions by DHBs to regional priorities will be included in APs. Worked examples for Electives and Mental Health are attached as Appendix Two. Table One: Guidance Framework for RSP Priorities Line of sight across Regional and Annual Plans RSP - Common Priorities and Objectives Priorities and objectives that DHBs within a region want to achieve. RSP - Key Actions, Milestones and Measures Key actions to set out what the region will do to achieve its objectives (and where appropriate significant individual DHB contributions are identified) Key milestones required to reach regional objective Measures the region will use to assess actions agreed to achieve milestones, including setting of baselines RSP - Inputs / Resources The nature of inputs may vary and could include: Costs to implement actions in order to achieve priority People / teams / and/or new roles required to progress actions RSP - Responsibilities Accountable roles Organisations and/or networks required to implement priority e.g. PHOs Page 6 of 24 RSP – Requirements of Enablers to Achieve Regional Priorities Workforce, IT and capital requirements to deliver on regional services priorities should be explicitly identified where relevant to achieving a regional objective. AP – Individual DHB’s Contribution to Regional Priorities The AP in Module 2 sets out the DHB’s individual actions to deliver against regional priorities and targets. This should include: Key individual DHB actions to deliver on regional milestones and priorities (links to regional actions) Measures to demonstrate progress on regional milestones and priorities Budget allocation by DHB To streamline reporting, the local actions of DHBs to deliver on regional objectives are reported quarterly within a consolidated regional report by Shared Services Agencies on behalf of DHBs. This is intended to streamline reporting as individual DHBs will not be required to report local actions to support regional priorities through their local DHB quarterly reports. 5.2 Linkages with Māori Health Plan Activities to improve Māori Health must be included within each regional service priority area. The activities are to include performance measures that must be measurable as part of the DHB accountability framework. Performance expectations for Māori must be set at the same level for the total population. Intervention mechanisms, actions or plans will include a mixture of universal and tailored activities. 6. National Entities Linkages with other work, in particular across the National Health IT Plan, HWNZ, Capital, the National Health Committee (NHC), and the Health Quality and Safety Commission (HQSC) also need to be considered. 6.1 Health Quality and Safety Commission DHBs are required to incorporate Health Quality and Safety Commission programmes into their regional services plans, as outlined in the Commission’s Statement of Intent 2012-15. In particular, DHBs are encouraged to demonstrate a commitment to the Open for better care national patient safety campaign, and ensure that activities support the campaign. Each region is expected to: involve consumers (patient and family) at every level of activity; maintain and participate in regional governance approaches that ensure regional and local leadership of the campaign; work with the Commission to design the topic-specific approaches to the campaign; work with the Commission to implement the campaign regionally and locally; and develop networks to support the campaign and build capability for improvement. Outside the important work of Open for better care, DHBs should also maintain appropriate mortality and morbidity review systems including supporting national Mortality Review Committee processes. Page 7 of 24 6.2 National Health Committee RSPs should describe how regions will work with the National Health Committee (NHC) to establish regional networks for the prioritisation of health interventions. These regional prioritisation networks are expected to become operational in 2014. Plans should include some discussion of how prioritisation will be coordinated with the NHC work programme, and how prioritisation decisions will be implemented by DHBs within the region. The NHC is an independent statutory committee charge with prioritising new and existing health technologies and making recommendations to the Minister of Health. Technologies under consideration by the NHC or a regional prioritisation network may not be implemented, or be expanded if already in use, by DHBs until the results of assessments are made available for implementation. Page 8 of 24 Appendix One: 2014/15 Regional Services Plan Priorities It is expected DHBs will use the Line of Sight framework to develop and document content for 2014/15 RSP priorities. This section provides more specific information about the requirements and expectations of the priorities to assist DHBs when completing content for their plans. 1. 2. 3. 4. 5. 6. 7. 8. 9. Elective Services Cancer Services Cardiac Services Mental Health and Addictions Stroke Services Health of Older People Major Trauma Information Technology Workforce 1. ELECTIVES I Regional Objectives Improve access to elective services; Reduce waiting times for elective first specialist assessment (FSA) and treatment; and Improve equity of access to services, so patients receive similar access regardless of where they live. Key Actions Identify the actions that the region will undertake to improve access to elective services, reduce waiting times and improve equity of access. These actions will differ by region but could include: Developing a regional delivery plan that supports achievement of local intervention rates, maximised regional capacity, optimal use of specialist resources and sub-specialist capability, increased access to less complex surgery and local Health Target Delivery. Developing consistent pathway, access criteria, and clinical protocols for individual services. Establishing and delivering sub-regional agreement to facilitate cross-boundary patient care. Implementing sub-regional referral management and scheduling systems. Delivering actions agreed to in regional Elective Services Productivity and Workforce Programme (ESPWP) contracts. Measure For the 2014/15 year it is expected that: your region’s Electives Health Target will be met; by the end of December 2014, zero patient’s will wait more than 4 months for First Specialist Assessment (FSA) or elective treatment; and a maximum waiting time of 4 months is maintained from January 2015 onwards (ESPI 2 & ESPI 5). Page 9 of 24 Information Technology Identify the actions that the region will undertake to support improved information management. For example, establishing a regional oversight role to ensure any actions required to contribute to or implement the National Patient Flow collection are regionalised where possible. Workforce Identify the actions that the region will undertake to maximise workforce resources. For example, completing a forecast through to 2017/18 of future workforce requirements, developed based on service demands and maintaining a local and regional view of specialist workforce capacity and capability. 2. CANCER SERVICES I Regional Objectives Implementing the priorities of the National Cancer Programme remains the focus for regional planning. In particular to improve: access to cancer services; timeliness of services across the whole cancer pathway; and the quality of cancer services delivered. Key Actions Identify the actions your region will undertake to improve access, timeliness and the quality of cancer services. For example: Improve the functionality and coverage of multidisciplinary meetings (MDMs) by implementing the regionally agreed MDM priorities; and Implement actions that support the region to deliver on the priorities for cancer as outlined in the DHB annual plan guidance, e.g. regional radiation oncology and medical oncology services. Measures For each quarter of the 2014/15 year it is expected that: The cancer treatment health target will be met; Improvement in performance against the policy priority (PP30) faster cancer treatment indicators is evidenced; Progress against specific agreed actions to support the regional objectives is demonstrated; and Improvement in coverage and functionality of MDMs as reported against the policy priority (PP24) improving waiting times – cancer multidisciplinary meetings, is demonstrated. Page 10 of 24 3. CARDIAC SERVICES I Regional Objectives The focus for regions in 2014/15 will be to continue to improve access to cardiac services including: improved and timelier access to cardiac services; patients with a similar level of need receive comparable access to services, regardless of where they live; more patients survive acute coronary events, and likelihood of subsequent events are reduced; and patients with suspected Acute Coronary Syndrome (ACS) receive seamless, co-ordinated care across the clinical pathway. Key Actions To continue to work with regional cardiac clinical networks and the New Zealand Cardiac Network to implement actions to improve outcomes for people. To provide quarterly reporting at regional and DHB level, utilising the ANZACS-Q1 and Cardiac Surgery registers. Secondary Services Develop and deliver a regional (or sub-regional in South Island) plan for cardiac services, ensuring appropriate access to cardiac surgery, percutaneous revascularisation and coronary angiography. All cardiac surgery patients are prioritised, and treated in accordance with assigned priority and urgency timeframes. Sustain performance against cardiac surgery waiting list management expectations. Acute Coronary Syndrome The phased introduction of Accelerated Chest Pain Pathways1 (ACPPs) in Emergency Departments will begin in 2014/15. A working group linked to the New Zealand Cardiac Network and Emergency Department Clinical Groups has commenced preliminary work on ACPPs. Support will be provided to DHBs to develop, implement and measure ACPPs. Implement regionally agreed protocols, processes and systems to ensure prompt local risk stratification and management of suspected ACS patients. Implement systems for prompt transfer of high risk patients to tertiary centres for the appropriate interventions. Measures Secondary Services Standardised intervention rates: o Cardiac surgery: 6.5 per 10,000 of population o Percutaneous revascularisation: 12.5 per 10,000 of population o Coronary angiography: 34.7 per 10,000 of population 1 Accelerated Chest Pain Pathways (ACPPs) are patient assessment pathways that speed up the diagnostic process for patients with chest pain, without compromising patient safety. ACPPs have significant potential as diagnostic tools to improve patient outcomes and save time and resources in Emergency Departments. Page 11 of 24 Proportion of patients scored using the national cardiac surgery Clinical Priority Access Criteria (CPAC) tool, and proportion of patients treated within assigned urgency timeframe. The waiting list for cardiac surgery remains between 5% and 7.5% of planned annual cardiac throughput, and does not exceed 10% of annual throughput. No patient waits longer than five months for cardiac surgery during 2014 and waiting times are reduced to a maximum of four months by the end of December 2014. Acute Coronary Syndrome Report quarterly on regional activity that supports Accelerated Chest Pain Pathway development and implementation Each region will have established measures of ACS risk stratification and timeliness for patients to receive appropriate intervention 70% of high-risk patients will receive an angiogram within 3 days of admission. (‘Day of Admission’ being ‘Day 0’) Over 95% of patients presenting with ACS who undergo coronary angiography have completion of ANZACS-QI ACS and Cath/PCI registry data collection within 30 days Please note: A national definition for the counting of high risk will be made available as soon as it is agreed. 4. MENTAL HEALTH AND ADDICTIONS I Regional Objectives Our objectives for 2014/15 are to improve: access to the range of eating disorder services; adult forensic service capacity and responsiveness through the national forensic network; youth forensic service capacity and responsiveness; perinatal and maternal mental health service options as part of a service continuum; and mental health and addiction service capacity for people with high and complex needs. Key Actions Identify and deliver on at least two actions for each of the following that will lead to: continued regional provision of eating disorder inpatient services (Midland and Northern regions to implement the recommendations from the service review to ensure sustainable inpatient and community services); improved Mental Health and Addiction Service capacity for people with high and complex needs; robust regional contribution to the national network of forensic inpatient services AND: Develop and implement actions for a Community Youth Forensic Service Plan with the agreed number of additional FTEs. In the North Island, the regions Northern, Midland and Central develop and implement the appropriate options to establish a perinatal and maternal mental health service as part of a continuum of care. Measures A reduction in waiting lists and times for people in prisons requiring assessment in forensic services. For example: a reduction in waiting lists from x to y with targets set for each quarter. Page 12 of 24 Increased access to community youth forensic services through the development of sustainable youth forensic services and availability of liaison officers in court. For example: the number of liaison officers in court will increase from x to y with progress tracked each quarter. Increased access in the North Island to perinatal and maternal mental health services. For example: x being current numbers to be increased to y with progress measured each quarter. 5. STROKE SERVICES I Regional Objectives To improve stroke prevention, stroke event survival, and reduce subsequent stroke events; and to improve access to organised acute and rehabilitation stroke services. Key Actions Continue to implement NZ Clinical Guidelines for Stroke Management 2010 (the Stroke Guidelines). This will include: People with stroke admitted to hospital and treated in a stroke unit with an interdisciplinary stroke team. Smaller DHBs, as defined in the Stroke Guidelines, are expected to develop models of stroke care that adhere as closely as possible to the criteria for stroke unit care. All eligible patients, as specified in the clinical definition previously supplied to DHBs, have access to thrombolysis. All stroke patients receive early active rehabilitation by a multidisciplinary stroke team All people with stroke have equitable access to community stroke services, regardless of where they live. All members of the multidisciplinary stroke team participate in ongoing education and training according to the Stroke Guidelines. Measures Provision of quarterly reports that provide progress on: 6% of potentially eligible stroke patients thrombolysed; 80% of stroke patients admitted to a stroke unit, or for smaller DHBs, stroke patients admitted to an organised stroke service with a demonstrated stroke pathway; AND: percentage of eligible* patients receiving active rehabilitation (as recommended in the Stroke Guidelines) as part of their acute in-patient event; and percentage of eligible* patients following discharge who receive community based stroke rehabilitation services. *Defined as those patients referred for rehabilitation by lead physician/neurologist Workforce Identify actions that the region will take to develop and implement an ongoing education programme that supports a sustainable and quality clinical workforce. Information Technology Identify actions that the region will take to support improved information management, e.g. establishing a regional oversight role. Page 13 of 24 6. HEALTH OF OLDER PEOPLE I Regional Objectives To ensure people with dementia and their families and whānau are valued partners in an integrated health and social support system that supports wellbeing and control over their circumstances. The focus for regions in 2014/15 will be that Regional Dementia Care Pathway Groups (with involvement from secondary, primary and community care) will: develop regional components of the dementia care pathways and share learnings and resources across the region; improve awareness and responsiveness in primary health care, working in partnership with the dementia sector and primary health care organisations; continue to provide support and overview of the development and implementation of DHB dementia care pathways following the New Zealand Framework for Dementia Care; and provide representation at a national level when requested by the Ministry of Health (approximately twice a year) to provide an overview of DHB development and implementation of dementia care pathways and share learnings and ideas nationally. Key Actions Regions identify and develop components of dementia care pathways that are best achieved at a regional level. For example, x components of dementia care pathways that are best achieved at a regional level are identified by 30 September 2014; y components of dementia care pathways are developed at a regional level by 31 March 2015. Regions develop and commence delivery of dementia awareness and responsiveness education programmes for primary health care clinicians. For example, z number of primary care clinicians have attended dementia awareness and responsiveness programmes (number reported each quarter). Regions provide representation at national dementia meetings organised by the Ministry of Health. Measures Report quarterly on regional activity that supports DHB dementia care pathway development and implementation. Report six monthly on the development and commencement of dementia awareness and responsiveness education programmes in Primary Health Care (as set out in the CFA variations). x regional representatives attended national meetings organised by the Ministry of Health. Workforce Regions develop dementia awareness and responsiveness education programmes that educate primary health care clinicians on: the importance of an early diagnosis of dementia; diagnosing dementia (e.g. diagnostic tools, use of CT scanning); diagnosing delirium; and managing dementia (including optimal use of acetylcholinesterase inhibitors and training on the use of the local dementia care pathway). Page 14 of 24 7. MAJOR TRAUMA I Regional Objectives To ensure more patients survive major trauma and recover with a good quality of life the Major Trauma National Clinical Network is developing major trauma systems across New Zealand. Key Actions Regions develop and implement a three year regional action plan that in year 1 supports the collection and reporting of a nationally consistent major trauma data set for each DHB in the region. Progress in years 2 and 3 focuses on the implementation of local and regional major trauma systems. Establish a process so that each DHB in a region collects and reports the data required to implement a national major trauma register by 1 July 2015. This will involve aligning local trauma definitions with those used in the New Zealand Major Trauma Minimum Dataset (NZMTMD). Regions identify a designated clinical lead and co-ordinator at each DHB to provide a focus for major trauma care delivery and quality initiatives in 2014/15. Measures Where DHBs already have capacity to report on the NZMTMD, quarterly reporting on the NZMTMD on at least 50% of the fields will commence on 1 July 2014. Where regions and DHBs are building capacity, it is expected that processes for measuring and commencing reporting on the full NZMTMD will be established by 1 July 2015. All DHBs will have commenced reporting on the full NZMTMD by 1 July 2015. Information Technology All regions and DHBs will establish data systems capable of recording the fields in the NZMTDS to be able to report that data to the national major trauma registry. Page 15 of 24 INFORMATION TECHNOLOGY I Initiative Description DHBs/Regions impacted Service priorities enabled by the initiative Measures eMedicines Reconciliation (eMR) with eDischarge Summary Implementation of electronic reconciliation of medicines on admission and discharge from hospital. All DHBs Health of Older People and Long term conditions (Cancer, Cardiac and Stroke) All DHBs have implemented eMR and the national clinical standard for eDischarges Regional Clinical Workstation (CWS) and Clinical Data Repository (CDR) Implementation of a regional Clinical Workstation (Orion, Concerto) and Clinical data repository (mixed products). Midland and Central regions Supports all service priorities – the CWS and CDR are the key clinical systems in the hospital 100% of the applicable population have a CDR record available through a regional view Northland, Auckland, Whanganui, MidCentral, Wairarapa, Nelson Marlborough, Canterbury and South Canterbury DHBs Supports all service priorities – the PAS is one of the backbones of the hospital All affected DHBs will be implementing a supported PAS The CWS is a web based system, accessed via a single sign-on that connects multiple clinical applications and data sources to provide clinicians with secure access to patient data. A CDR is a database of patient identifiable clinical information such as medications, laboratory results, radiology reports, care plans, patient letters and discharge summaries. Replacement of legacy Patient Administration Systems (PAS) The 8 DHBs with legacy PAS need to progress implementation of a supported system that is aligned with the regional plan. The PAS supports and manages the administrative details of a patients encounter with a hospital or DHB service. It supports the management of the hospital resources used to provide patient care such as clinical staff, rooms, beds and equipment. National Patient Flow National Patient Flow will create a new national collection that provides a view of wait times, health events and outcomes in a patient’s journey through secondary and tertiary care. All DHBs Elective Services, Long term conditions – cancer services All DHBs have implemented phase 2 of National Patient Flow Finance Procurement and Supply Chain The Finance procurement and Supply Chain programme will implement a single finance management information system, common catalogue for the ordering of goods and services, and centralised procurement and distribution processes for DHBs. All DHBs – as per the HBL implementation plan Supports financial sustainability As per the HBL implementation plan Page 16 of 24 Self-Care Portal Portals are an on-line IT tool that will enable individuals to have access to their own health information. It will enable patients to communicate with their primary health practitioners and add information to their health record. Each of the General Practice Patient Management System (PMS) vendors are developing portals, and Orion Health is developing a portal in conjunction with Canterbury DHB eSCRV project. All PHOs Health of Older People, Mental Health and addictions 75% of PHOs provide an afterhours summary to ED 25% of the PHO eligible population have accessed a self-care portal The critical IT priorities for 2014/15 are largely a continuation of the previous years. This is reflective of the size and complexity of some initiatives that are being implemented in a phased approach. 8. HEALTH WORKFORCE I Regional Objectives Strengthen health workforce capability and capacity through improving recruitment and retention. Strengthen and improve regional initiatives that: o maximise workforce resources, reduce duplication; o encourage flexibility and integrated team working; and o use all training settings, including primary and community integration and private settings. Key Actions DHBs to work with their Regional Training Hub Director to develop and deliver a workforce plan as part of the 2014/15 Regional Service Plan (RSP). The workforce plan will include actions and key milestones: to implement workforce initiatives that will: o deliver on regional service priorities, as identified in the 2014/15 RSP and local workforce priorities as identified in the DHBs’ annual plans o increase participation of Maori and Pacific from x to y FTEs in the workforce (e.g. scholarship programmes, supporting high school based programmes) o reduce number of non-vocational registrars in PGY 3 and above from x to y o increase the number of New Zealand trained SMOs from x to y o provide x number of nursing graduates, registered and enrolled nurses, with a one year internship using innovative strategies without increasing expenditure o meet the 70/20/10 funding criteria2 for post-entry training in medical disciplines in the region’s DHBs. The funding model is part of the DHB’s new medical training agreement with HWNZ, effective from 1 January 2014 and was provided to the DHBs on 24 September 2013. This new agreement is for a three-year term and it is anticipated that the funding model will be adjusted annually, after consultation and agreement with DHBs. 2 Page 17 of 24 to achieve the workforce mix and distribution required for the future. The workforce plan will use baseline workforce data collated over the last five years, service demand forecasts and will take account of workforce requirements in hard-to-staff clinical specialties and geographical high need areas. to implement systems to provide all HWNZ funded trainees with career advice, pastoral care and a career plan that aligns individual career aspirations with regional and national identified future health workforce needs. Build on the workforce section of the 2013/14 RSP and detail progress with actions and key milestones to: standardise at least four PGY1 and 2 programmes (in addition to the eight already standardised during 2012/13 and 2013/14), roll programmes out to other professional groups as appropriate, and optimise implementation across regions; implement at least two new roles/innovative ways of working, assist deployment of these across the region and share successes. (For example: registered nurse first surgical assistant, credentialing for primary care nurses in mental health and addictions, physician assistant, and simulation based training for multi-disciplinary teams); report on at least two clinical networks, detailing progress on network development and multi-disciplinary approaches. (For example: eye healthcare network, palliative care network, and cancer network); and report on at least two regional training programmes for the unregulated healthcare workforce, detailing progress. (For example: training for clinical exercise physiologist and allied health assistant). Measures Regional and local DHB level progress reporting on the above requirements and key actions to be provided via quarterly RSP reports. Page 18 of 24 Appendix two: Line of Sight – worked examples Outlined below are worked examples to demonstrate how a regional objective could be integrated with annual planning information requirements for electives and mental health. The tables demonstrate examples as to how a guidance structure could be developed and to show implementation across a region in a DHB’s Annual Planning template. An example of information that could be provided to demonstrate regional implementation in a DHB’s Annual Planning template for electives Electives Context Better Sooner More Convenient Health Services for New Zealanders in relation to electives means improved and more timely access to elective services. Objectives A health system that functions well for Electives is one that is: a) Increasing elective surgery discharges b) Increasing first specialist assessments c) Reducing waiting times for people requiring elective services d) Improving prioritisation and selection of patients e) Supporting innovation and service delivery Linkages f) Link with Outcomes Framework (Module 1 & 2) g) Links include with National, Regional, Local Actions to deliver improved performance Health system success is measured by Reporting Requirements Electives funding will be allocated to support increased levels of elective surgery, specialist assessment, diagnostics, and alternative models of care. Delivery against agreed volume schedule, including a minimum of xx elective surgical discharges in 2014/15 towards the Electives Health Target (will be provided in electives funding advice). Electives Initiative and Ambulatory Initiative: Monthly Health Target: Quarterly Standardised intervention rates and/or other mechanisms (such as demand analysis) will be used to assess areas of need for improved equity of access. Refer to SI4: Elective services standardised intervention rates. Quarterly: cardiac. Annually: major joints, cataracts. Actions that contribute to regional priorities Health system success is measured by Reporting requirements DHB C will support the development of a regional agreed pathway for X service by (date) by XYZ actions. Measures agreed within the Regional Services Plan Quarterly regional report DHB C will manage a service delivery contract with X DHB to see and treat X of our domiciled patients Measures agreed within the Regional Services Plan Quarterly regional report Include local component of common measures used monitor its contribution to the delivery of its regional milestones. Measures agreed within the Regional Services Plan Quarterly regional report Mental Health and Addictions Services Plan Context: Rising to the Challenge: Rising to the Challenge clearly articulates prioritised service developments to 2017. The Plan aims to improve client access and service responsiveness across the spectrum of health promotion, primary, specialist treatment and support services. Service integration will be strengthened while improving value for money and delivering improved outcomes for people using mental health and addiction services. As ALTs mature DHBs will be expected to incorporate a broader range of service development involving the appropriate stakeholders within the ALTs. In the 2014/15 year DHBs are expected to develop an alliancing arrangement that follows the principles of partnership and joint service development and implementation with appropriate stakeholders for the Mental Health and Addiction Plan Module. Refer to the Alliance Charter for a description of the principle of partnership that must underpin any service development. Rising to the Challenge overarching objectives Actively using our resources more effectively Building infrastructure for integration between primary and specialist services Cementing and building on gains in resilience and recovery Delivering Increased access Actions to deliver improved performance Health system success is measured by Health system success is measured by: For each of the four key objectives from Rising to the Challenge identified below, provide at least 2 actions for each area, with targets and 6 monthly milestones for 2014/15. Expected 1. Make better use of resources/value for money Expected 2. 3. Improve integration between primary and specialist services Expected Cement and build on gains in resilience and recovery (this includes developing services for Children of Parents with Mental illness and Addictions). Expected. 4. Deliver increased access for all age groups Expected Deliver and report on required actions with targets and 6 monthly milestones for 2014/15 which will either increase access or improve outcomes for each of the following Government work programmes: a. Drivers of Crime b. Welfare reforms Expected Implementation of the New Zealand Suicide Prevention Action Plan 2013-2016. DHBs are expected to provide evidence of how the following will be met: train health workers to identify and support individuals with self-harm injuries or at risk of suicide and refer them to the Reporting Requirements Meeting agreed performance measure expectations for: - PP6, PP7,PP8 ,PP26 &OS10 - quarterly reporting on SDP progress against actions Performance against agreed measures. Progress on specific actions. All above indicators are expected TBC Submit district suicide prevention plans for review in the second quarter reporting. Expected services they need. Expected develop and implement a district suicide prevention plan. Expected facilitate integrated cross-agency collaboration in respect to suicide prevention and response to suicide clusters/contagion. Expected develop and implement a district suicide postvention plan. Expected Mental health and addiction service provision ringfence. Please explain how the mental health and addiction ringfence is assured in the planning process. The ringfence calculation will include demographic and cost pressure increases, supplemented by expenditure under- spends to bring forward growth so that the long term growth path can be maintained Also show the connection between maximising ringfence funding and addressing service gaps. Expected TBC TBC Actions that contribute to regional priorities * Health system success is measured by Reporting requirements DHB C will commit to delivery of the actions agreed in Region A’s Regional Service Plan. Measures agreed within the Regional Service Plan Quarterly regional report